Acromioclavicular joint dislocation with a double coracoid fracture is a rare injury that can be successfully managed by arthroscopic-assisted techniques.
Dr. Anand Kumaroth Somasundaram, Department of Orthopaedics, Villa Number 5, Abad Royal Gardens, Old MC Road, Thellakom – 686630, Kottayam, Kerala, India. E-mail: anandsvkas@gmail.com
Introduction: Acromioclavicular joint (ACJ) dislocation associated with coracoid process fracture is an uncommon injury. Herein, we report a case with such a combination of injuries. This is the first reported case of its kind to be managed with an arthroscopic technique.
Case Report: A 48-year-old female was injured by a direct fall on her right shoulder. Initial conservative management failed, which led to persistent pain and functional impairment. A late diagnosis of ACJ dislocation was made, necessitating surgical intervention. The patient was successfully treated using an arthroscopically assisted stabilization technique with tendon graft augmentation and an arthroscopic repair of a superior labral tear, which was diagnosed intraoperatively. Post-operative outcomes were favorable, showing the efficacy of this approach for managing such complex shoulder injuries.
Conclusion: This case signifies the importance of early detection of concomitant injuries of the superior shoulder suspensory complex in high-velocity ACJ injuries, which, when not diagnosed timely, necessitate complex surgical procedures later. This also highlights the possibility of minimally invasive arthroscopic techniques for managing late presentation of such an injury.
Keywords: Acromioclavicular joint dislocation, coracoid process fracture, shoulder instability, arthroscopic stabilization.
Acromioclavicular joint (ACJ) injuries are common, particularly in young and active individuals, often resulting from direct trauma to the shoulder. ACJ damage is also a common diagnosis following acute shoulder trauma, particularly among athletes and others who engage in contact sports [1]. The superior shoulder suspensory complex (SSSC) is a significant structure in shoulder biomechanics; it is composed of a ring of bony and soft tissues at the superior aspect of the shoulder. It consists of the distal end of the clavicle, the ACJ, the coracoacromial ligament, the glenoid process, the coracoid process, the coracoclavicular ligament, and the acromial process [2]. ACJ is an integral part of SSSC. Treatment, including surgery, may be necessary for instability caused by disruptions to the SSSC. ACJ separation is defined by a loss of articular contact between the distal end of the clavicle and the medial acromion [3,4]. The association with coracoid process fractures is infrequent and may be initially overlooked, leading to delayed diagnosis and suboptimal outcomes [5]. The ACJ is critical for shoulder stability, and a dislocation of this joint can significantly damage shoulder function, frequently producing pain and instability in the shoulder complex if not treated [5,6]. ACJ dislocations are typically classified using the Rockwood classification system based on the severity of ligamentous disruption and clavicular displacement, while coracoid fractures are classified according to the Ogawa classification, which differentiates between fractures at the base and those involving the tip [7]. Isolated coracoid fractures and low-grade ACJ dislocations are frequently treated conservatively, which includes rest, analgesics, and immobilization with a sling. Several surgical approaches for stabilizing the ACJ have been documented, including open reduction and internal fixation, ligament repair with tendon graft augmentation, and arthroscopic-assisted operations. This case report discusses the late onset of a concurrent ACJ dislocation and double fractures of the coracoid process in a 48-year-old female who sustained a direct fall on her right shoulder. The patient was initially treated conservatively, but chronic discomfort and functional limitations suggested more investigation. The delayed diagnosis of ACJ dislocation was verified by advanced imaging, which revealed a complex damage pattern requiring surgical intervention. Given the difficulties associated with open surgical procedures, an arthroscopically assisted stabilization treatment with tendon graft augmentation was chosen to restore joint integrity and accelerate recovery.
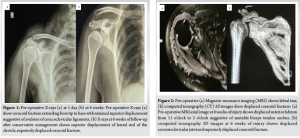
A 48-year-old female presented to the emergency room with a complaint of a fall from a height. Following the incident, the patient experienced retrograde amnesia and substantial pain in her right shoulder and hand while moving. Upon arrival, she was hemodynamically stable but was in significant discomfort. She was initially diagnosed with a right coracoid fracture and had a history of rheumatoid arthritis, for which she was receiving long-term treatment with hydroxychloroquine. During the initial evaluation, she had tenderness around the coracoid process of the right shoulder with severe painful restriction of shoulder movements. She also had symptoms and signs suggestive of a concussion injury to the brain. She had normal systemic examinations. Radiological investigations included a magnetic resonance imaging (MRI) of the cervical spine, revealing straightening due to paraspinal muscle spasm and mild posterior bulging of the C3-C6 discs without significant foraminal compromise. A computed tomography (CT) scan of the brain ruled out acute intracranial pathology. A CT scan of the thorax identified a displaced coracoid process fracture, and a right shoulder CT confirmed a double fracture of the coracoid process. However, the associated ACJ dislocation was left undiagnosed in the initial evaluation. The patient was managed conservatively with standard analgesia and a shoulder immobilizer. Despite adherence to conservative treatment, persistent pain and functional limitations were noted in subsequent follow-ups. A 6-week follow-up X-ray revealed non-union of the coracoid fracture along with ACJ dislocation, which had been previously undiagnosed. Further evaluations showed significant shoulder instability, persistent pain, and muscle wasting, with restricted movements in forward flexion, abduction, and external rotation.(Fig. 1 ). An MRI of the right shoulder later confirmed an anteroinferior labral tear, a small Hill-Sachs lesion, and ACJ dislocation. A fresh CT scan showed a double fracture of the coracoid extending to the base with superior displacement of the ACJ. Multiple ipsilateral rib fractures were also identified. Given the failed conservative management, a multidisciplinary team recommended surgical intervention.(Fig. 2 )
Surgical management
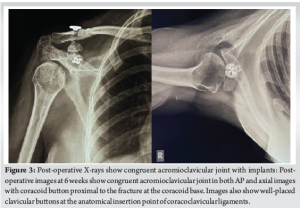
The procedure was performed in a beach chair position under general anesthesia and interscalene nerve block. The right lower extremities were separately cleaned and draped for graft harvesting. A 2.5 cm incision was made at the upper medial tibia, and the semitendinosus and gracilis tendons were harvested. A doubled semitendinosus-gracilis graft construct was prepared, measuring 7 × 220 mm with a width of 7 mm. After washing and layered closure of the incision, the right shoulder was prepped for surgery. The coracoid tip was identified, and skeletonization was performed using a 70°-scope system. Dissection of the coracoid was carried out, revealing an ununited fracture of the coracoid in longitudinal orientation along the length of the coracoid, representing a bony avulsion of coracoclavicular ligaments with superior displacement. The fracture site showed minimal mobility on probing. The fracture site was refreshed using an angled curette to promote healing. The intact portion of the coracoid base, located near the scapular neck, was identified. Using a tibial posterior cruciate ligament jig, through a 3 cm incision over the clavicle, serial drilling was performed from the clavicle to the coracoid over a guidewire using a 4.5 mm drill bit. Through a separate mid-rotator interval portal and an anterolateral portal, suture passage was performed. A dog-bone button construct with two suture tapes was fixed at the coracoid base and passed through the clavicular drill hole. The semitendinosus-gracilis tendon construct was then looped around the coracoid and secured anteriorly and posteriorly to the clavicle in a figure-of-eight configuration. After reducing the ACJ, the suture tapes were tied and trimmed, and a cortical button was placed over the clavicle. The tendon grafts were further tightened and sutured in place. Fluoroscopy confirmed acceptable reduction and stabilization of the ACJ. Using standard mid-rotator interval and anterolateral portals, along with a Wilmington portal, the labral repair was performed using three knotless suture anchors and suture tapes. Biceps long head tenodesis was completed in the groove using a separate knotless anchor and fiber wire sutures. At the end of the procedure, the ACJ and glenohumeral joints exhibited stability, and the biceps tenodesis remained intact. All surgical portals were closed in layers, and compression dressings were applied. The patient’s shoulder was protected in an arm sling pouch.(Fig. 3 )
Outcome
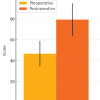
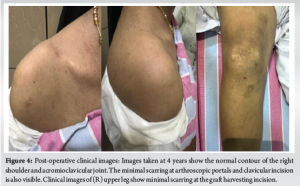
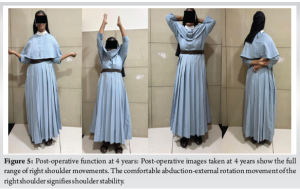
At a 4-year follow-up, the patient’s shoulder is stable and has a full, pain-free range of motion. She has no limitations on activities of daily living.(Fig. 4 and 5 )
ACJ injuries occur in all age groups. ACJ dislocation combined with a coracoid process fracture is an unusual injury. It typically happens in young male adults in the setting of high-energy traumas such as road traffic accidents, falls from height, or sports injuries. ACJ dislocations can be classified into six types using Rockwood classification. Types I and II are frequently treated conservatively; the treatment of type III is uncertain, whereas types IV, V, and VI often require surgical management. Coracoid process fractures are categorized into two forms based on their placement relative to the CC ligaments: type I fractures are proximal to the insertion of the capsule and coracoclavicular (CC) ligaments, and type II fractures are distal [6,7]. We present a case of a 48-year-old female with an acromioclavicular joint dislocation and double fractures of the coracoid process (fractures of the tip and bony avulsion of CC ligaments with fracture line extending from the tip to the base of the coracoid) as a result of a fall from height. The management of ACJ dislocation with an associated coracoid process fracture remains controversial in the orthopedic field. Concomitant coracoid fractures can hide ACJ injuries, resulting in missed diagnoses and extended patient suffering. The Rockwood classification is the standard one used to diagnose these injuries, and it guides many surgeons in their surgical decisions [8,9]. Plain radiographs are the standard imaging investigation after injury to the ACJ [5,10-12]. Our case further supports these findings, as the ACJ dislocation was only identified 6 weeks after the initial injury, and further advanced imaging was required to identify associated labral injuries. Labral injuries in ACJ dislocations were reported to be 27% [13]. Conservative treatment is typically recommended for isolated coracoid fractures and low-grade ACJ dislocations [14,15]. In our case, initial conservative management failed, which led to persistent pain and functional impairment and necessitated surgical management. The patient was managed arthroscopically. Arthroscopic-assisted methods offer reduced surgical morbidity, improved visualization, and faster recovery [16-19]. In our study, the patient showed uneventful post-operative recovery with restored stability and function of the shoulder. Tendon graft augmentation was done in our patient as it offers enhanced stabilization and improved long-term outcomes [20,21]. The present case indicates the efficacy of arthroscopically assisted ACJ stabilization with tendon graft augmentation in a late presentation of ACJ dislocation with coracoid fracture; nevertheless, more comparative researches with bigger sample sizes are required to develop standardized treatment standards. Future studies should look at the biomechanical benefits of different graft materials and fastening procedures for improving clinical outcomes in patients with complex ACJ injuries associated with coracoid fractures.
The late presentation of ACJ dislocation with double coracoid fractures poses an uncommon but significant clinical problem. Early detection is critical for avoiding problems such as chronic discomfort, instability, stiffness, and functional restrictions. Arthroscopic-assisted stabilization with tendon graft augmentation is a minimally invasive and successful method for improving joint stability and fracture healing. This example emphasizes the significance of conducting thorough clinical and radiographic examinations in complex shoulder trauma to ensure timely diagnosis and proper treatment.
Our case is a learning example for having a high index of suspicion of ACJ injuries in patients who present with apparently isolated coracoid fractures in the setting of major shoulder trauma. It also teaches us the valuable lesson of serially following these patients with stress radiographs of ACJ, which can potentially aid in diagnosing the injuries relatively earlier. Advanced imaging modalities such as MRI can help diagnose associated glenohumeral pathology. Even in a delayed presentation of this injury, a well-planned arthroscopic assisted procedure can yield acceptable results.
References
- 1.Sirin E, Aydin N, Mert Topkar O. Acromioclavicular joint injuries: Diagnosis, classification and ligamentoplasty procedures. EFORT Open Rev 2018;3:426-33. [Google Scholar]
- 2.Goss TP. Double disruptions of the superior shoulder suspensory complex. J Orthop Trauma 1993;7:99-106. [Google Scholar]
- 3.Albishi W, AlShayhan F, Alfridy A, Alaseem A, Elmaraghy A. Acromioclavicular joint separation: Controversies and treatment algorithm. Orthop Rev (Pavia) 2024;16:94037. [Google Scholar]
- 4.Kiel J, Taqi M, Kaiser K. Acromioclavicular joint injury. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2025. Available from: http://www.ncbi.nlm.nih.gov/books/nbk493188 [Last accessed on 2025 Feb 25]. [Google Scholar]
- 5.Kose O, Canbora K, Guler F, Kilicaslan OF, May H. Acromioclavicular dislocation associated with coracoid process fracture: Report of two cases and review of the literature. Case Rep Orthop 2015;2015:858969. [Google Scholar]
- 6.Galán-Olleros M, Lopiz Y, Arvinius C, García-Fernández C, Marco F. Acromioclavicular joint dislocation associated with a coracoid process fracture: Report of 2 cases. JSES Int 2020;4:564-8. [Google Scholar]
- 7.Sonnier JH, Kemler B, Coladonato C, Paul RW, Tjoumakaris FP, Freedman KB. Surgical management of acute, high-grade acromioclavicular joint separations: A systematic review. JSES Rev Rep Tech 2023;3:10-20. [Google Scholar]
- 8.Chillemi C, Franceschini V, Dei Giudici L, Alibardi A, Salate Santone F, Ramos Alday LJ, et al. Epidemiology of isolated acromioclavicular joint dislocation. Emerg Med Int 2013;2013:171609. [Google Scholar]
- 9.Haugaard KB, Bak K, Seem K, Hölmich P, Barfod KW. Rockwood type III is the most common type of acromioclavicular joint dislocation: A prospective cohort study investigating the incidence and epidemiology of acute acromioclavicular joint dislocations in an urban population. Shoulder Elbow 2023;15:505-12. [Google Scholar]
- 10.Granville-Chapman J, Torrance E, Rashid A, Funk L. The Rockwood classification in acute acromioclavicular joint injury does not correlate with symptoms. J Orthop Surg (Hong Kong) 2018;26:2309499018777886. [Google Scholar]
- 11.Pogorzelski J, Beitzel K, Ranuccio F, Wörtler K, Imhoff AB, Millett PJ, et al. The acutely injured acromioclavicular joint - which imaging modalities should be used for accurate diagnosis? A systematic review. BMC Musculoskelet Disord 2017;18:515. [Google Scholar]
- 12.Lee SY, Kwon SS, Chung CY, Lee KM, Park MS. What role do plain radiographs have in assessing the skeletally immature acromioclavicular joint? Clin Orthop Relat Res 2014;472:284-93. [Google Scholar]
- 13.Mansour J, Nassar JE, Estephan M, Boulos K, Daher M. Acromioclavicular joint dislocation and concomitant labral lesions: A systematic review. Clin Shoulder Elb 2024;27:247-53. [Google Scholar]
- 14.Duan X, Zhang H, Zhang H, Wang Z. Treatment of coracoid process fractures associated with acromioclavicular dislocation using clavicular hook plate and coracoid screws. J Shoulder Elbow Surg 2010;19:e22-5. [Google Scholar]
- 15.Galvin JW, Kang J, Ma R, Li X. Fractures of the coracoid process: Evaluation, management, and outcomes. J Am Acad Orthop Surg 2020;28:e706-15. [Google Scholar]
- 16.Tomlinson DP, Altchek DW, Davila J, Cordasco FA. A modified technique of arthroscopically assisted AC joint reconstruction and preliminary results. Clin Orthop Relat Res 2008;466:639-45. [Google Scholar]
- 17.Passaplan C, Beeler S, Bouaicha S, Wieser K. Arthroscopic management of a coracoid fracture associated with acromioclavicular dislocation: Technical note. Arthrosc Tech 2020;9:e1767-71. [Google Scholar]
- 18.Ruzbarsky JJ, Nolte PC, Arner JW, Elrick BP, Tross AK, Millett PJ. Arthroscopic acromioclavicular joint treatment with coracoclavicular fixation and allograft coracoclavicular ligament reconstruction for acute acromioclavicular dislocations. Arthrosc Tech 2020;9:e1219-25. [Google Scholar]
- 19.Tingle M, Wang T, Hoenecke HR Jr. Current trends in surgical treatment of the acromioclavicular joint injuries in 2023: A review of the literature. JSES Int 2024;8:389-93. [Google Scholar]
- 20.Naziri Q, Williams N, Hayes W, Kapadia BH, Chatterjee D, Urban WP. Acromioclavicular joint reconstruction using a tendon graft: A biomechanical study comparing a novel “sutured throughout” tendon graft to a standard tendon graft. SICOT J 2016;2:17. [Google Scholar]
- 21.Pérez Rodríguez M, Paniagua González A, González Gómez I, Aguado Fernández JP, Minuesa Asensio ÁJ. Reconstruction of the acromioclavicular joint using a double augmentation with hamstrings tendon and dermal graft. Arthrosc Tech 2023;12:e433-40. [Google Scholar]