Ilizarov and LRS are both effective in compound tibial fractures, choice between Ilizarov and LRS should be individualized, as Ilizarov may aid faster function while long-term outcomes are comparable. Ilizarov fixation provides better early results, though both Ilizarov and LRS achieve similar long-term outcomes in compound tibial fractures.
Dr. Naman Kumar Parakhs, Department of Orthopedics, Teerthanker Mahaveer Medical College and Research Centre, Moradabad, Uttar Pradesh, India. E-mail: namanparakh1604@gmail.com
Background: Open diaphyseal fractures of the tibia, particularly Gustilo–Anderson Grade II, IIIA, and IIIB, pose significant treatment challenges due to high contamination, soft-tissue damage, and compromised vascularity. External fixation remains a preferred method in such cases. This study compares the functional and radiological outcomes of the Ilizarov ring fixator and the limb reconstruction system (LRS) in managing these injuries.
Materials and Methods: This prospective, comparative single-center-based study was conducted from December 2023 to May 2025 on a total of 68 patients aged between 20 and 70 years with Grade II, IIIA, or IIIB compound tibial shaft fractures. Four patients were excluded at the time of final analysis, out of which, three patients were lost to follow-up and in one patient had premature removal of Ilizarov frame. Patients were randomized into two groups: Group A (Ilizarov, n = 32) and Group B (LRS, n = 32). Outcomes were assessed at 6 weeks, 3, 6, and 9 months/final follow-up using the association for the study and application of the method of Ilizarov criteria and radiological callus formation scores.
Results: Both groups showed progressive improvement in bone and functional outcomes over time. At final follow-up, excellent bone results were noted in 43.8% patients of Group A and 37.5% of Group B, while excellent functional outcomes were achieved in 37.5% and 28.1% patients, respectively. Intergroup differences were statistically significant for functional results at the early follow-ups (P = 0.049 at 6 weeks) but became comparable by final follow-up.
Conclusion: Both the Ilizarov ring fixator and the LRS are effective in managing high-grade open tibial shaft fractures. We have achieved good to excellent results in terms of bony union and functional outcome in most of our patients in both Ilizarov and LRS groups, although Ilizarov scores significantly better.
Keywords: Compound tibial fracture, Ilizarov ring fixator, limb reconstruction system, association for the study and application of the method of Ilizarov criteria, bone healing, diaphyseal fracture.
The tibia is the most frequently fractured long bone, accounting for approximately 17.1–21% of all fractures and 36.7% of adult long bone injuries, with a reported incidence ranging from 17 to 21/100,000 individuals. Due to its subcutaneous anteromedial location and minimal soft-tissue coverage, the tibia is uniquely predisposed to open fractures, unlike other long bones. Optimal stabilization and early soft-tissue management are critical to improve the outcomes in such cases [1,2]. The primary etiologies include road traffic accidents (62.2%), fall from standing height (18.7%), sports injuries (7.4%), and direct trauma (8.3%). Epidemiological data indicates that around 23.5% of tibial shaft fractures are open in nature. Open tibial fractures present unique challenges due to compromised vascularity, bone loss, and the absence of adequate soft-tissue coverage, increasing their susceptibility to infection, estimated to be 10–20 times higher than in other anatomical sites and to complications such as delayed union, non-union (up to 28%), and malunion. Diagnosis is primarily based on clinical assessment and confirmed with radiographic imaging, including anteroposterior and lateral views of the affected tibia and fibula. In complex or segmental fractures, computed tomography imaging is warranted for surgical planning. Open fractures are classified according to the Gustilo-Anderson system, which guides both the urgency of surgical intervention and the choice of fixation and soft-tissue coverage strategies [3,4,5]. Current treatment modalities for compound tibial diaphyseal fractures include external fixation, intramedullary nailing, and, in selected cases, plate osteosynthesis with or without damage control orthopedics. However, in Grade II and higher-grade injuries with bone loss, extensive soft-tissue damage, or contamination, external fixation remains the preferred initial modality. The studies comparing external fixators and intramedullary nailing/plating for treating open tibia diaphyseal fractures showed that the rate of injury site infection, as well as surgical site superficial and deep infection, is significantly higher in intramedullary nailing and plating. The Ilizarov ring fixator and the limb reconstruction system (LRS) are two established external fixation techniques for fresh cases with extensive bone loss and contamination. The Ilizarov apparatus provides multiplanar stability and modularity but remains technically demanding. In contrast, the monolateral LRS offers technical simplicity and patient comfort, particularly in linear and non-segmental fractures. Both these methods facilitate bone transport and deformity correction through the principle of distraction osteogenesis/histiogenesis [4,5,6]. Although both systems are widely used, comparative data evaluating their functional and radiological outcomes in high-grade open tibial shaft fractures remains limited. This study aims to compare the efficacy of the Ilizarov ring fixator versus the LRS in the management of Gustilo-Anderson Grade II, IIIA, and IIIB compound diaphyseal tibial fractures.
Study design
This prospective, comparative single-center-based study was conducted from December 2023 to May 2025 and 68 eligible patients were enrolled, following approval from the College Research Committee and Institutional Ethics Committee (Ref No: TMU/IEC/November 23/115).
Inclusion criteria
Patients aged between 20 and 70 years with compound Grade II, IIIA, or IIIB diaphyseal fractures of the tibia primarily stabilized with tubular external fixator and presenting after 3 weeks of injury with wound related complications were included in the study.
Exclusion criteria
Compound tibial fractures with intra-articular extension and the presence of associated ipsilateral lower limb bony injuries other than the diaphyseal tibial fracture were excluded from the study.
Data source
After obtaining a written and informed consent, 68 eligible patients with compound diaphyseal fracture of tibia, presenting to the hospital were enrolled in the study and detailed history and clinico-radiological examination was done to diagnose and classify the patients according to the Gustilo–Anderson classification and detailed follow-up outcomes, were systematically documented.
Surgical technique
Using a computer-generated randomization sequence, patients were randomized into two groups. The Ilizarov ring fixator was used to treat Group A, while the LRS was used to treat Group B. All standard pre-operative institutional protocols were followed before the procedure. All the patients were operated in the supine position under spinal anesthesia. Copious fluid irrigation and extensive debridement of devitalized tissue were performed, and good circumferentially intact parallel bone surfaces of fracture ends were achieved before application of Ilizarov fixator or LRS. The debrided tissue was sent for culture and sensitivity and appropriate antibiotics were given to the patient. For Ilizarov, we used a preassembled three or four-ring frame construct using tensioned wires and half pins to increase the stiffness. For LRS, we used a monolateral medially placed 3 straight clamp based construct with middle mobile clamp, each using 2–3 tapered 6 mm bone screws. After application of Ilizarov/LRS, the limb lengths and bone defect were measured. If possible, an acceptable wound apposition was achieved by performing 2–3 cm of primary partial docking at fracture site with fibulotomy (if concomitant fibula fracture was not present). Low-energy, single-level corticotomy was done at either proximal or distal metaphyseal region for mono-focal bone transport. Postoperatively, intravenous antibiotics and analgesics were given until the wound became healthy, and then, oral second-generation cephalosporins antibiotics were given. Dynamic and static quadriceps exercises with range of motion exercises of knee and ankle were encouraged from the 1st post-operative day in all the cases. Weight-bearing, as tolerated with support was initiated from post-operative Day 2. Regular wound inspection and dressing were performed, and a 7-day latency period was given for tissue to recover. Distraction was started from post-operative day 7 with rate of 1 mm/day and rhythm of four distractions turns of 0.25 mm each spread out over 24 h. The same was taught to the patient. The bone transport was continued until the fracture ends approximated. All the patients were discharged on post-operative day 7 and called for regular follow-ups.
Follow-up and outcome measures
Patients were followed-up postoperatively at 3 weeks, 6 weeks, 3 months, 6 months, and 9 months and thereafter at every 3 month interval till Ilizarov frame/LRS removal with a minimum of 9 months follow-up. The clinical and radiological assessment was done using association for the study and application of the method of Ilizarov (ASAMI) criteria for functional and bone outcomes using anteroposterior and lateral radiographs of the affected leg, which were categorized as excellent, good, fair, or poor and callus formation scoring system, evaluating the percentage of callus diameter and density of the regenerate across predefined parameters. Moreover, during each follow-up, a meticulous check for wound healing, pin site infection, alignment, on-going distraction, formation and consolidation of regenerate, progression of union, or any complication was performed and recorded. Removal of the fixator was done once union in at least three cortices was confirmed on radiograph and stress test was found to be negative, that is, patient could perform full weight-bearing walk and movement without any pain. Refracture is a well-known, late but uncommon complication after frame removal. To prevent refractures, an extended period of fixator application was imposed thereby ensuring sound union and consolidation of the regenerate. Protected weight-bearing was advised in the early post-frame removal period [7,8].
Data collection and statistical analysis
Data from all cases were systematically recorded in Microsoft Excel (.xml format) and analyzed using IBM Statistical Package for the Social Sciences Statistics Version 20.0. Categorical variables were expressed as frequencies and percentages, while continuous variables were reported as mean with or without standard deviation. Inter-group comparisons of quantitative data were performed using analysis of variance, and categorical variables were compared using the Chi-square test. P < 0.05 was considered statistically significant.
A total of 68 patients were included after fulfilling the inclusion and exclusion criterion. Four patients (two from each group) were excluded at the time of final analysis, out of which, three patients were lost to follow-up and in one patient premature removal of Ilizarov frame was performed due to non-compliance and non-adherence to pin site care. The final analysis was performed on 64 patients, 32 in each group. The mean age of patients was 36.34 ± 12.54 in Ilizarov group and 38.5 ± 14.02 in LRS group. Majority of patients were male in both groups and all our patients sustained injury due to road traffic accidents. The mean follow-up was 12.62 months (range 9–16 months) in Ilizarov group and 11.85 months (range 9–15 months) in the LRS group. The mean bone defect was 4.15 cm (range 2–7 cm) in Ilizarov group and 3.86 cm (range 2–6.5 cm) in LRS group. Removal was done once union in at least three cortices was confirmed on radiograph and stress test was found to be negative, that is, patient could perform full weight-bearing walk and movement without any pain. The mean external fixator index was 62 days/cm (range 45–108 days/cm) for Ilizarov and 57 days/cm (range 42–102 days/cm) for LRS. In most of our patients’, wound size was substantially reduced after the primary partial docking and healed with secondary intention for closed approximation, except for four patients, where the wound size was substantially large and managed by an extended period of regular dressing. None of our patients received any extra procedure for wound management. The demographic characteristics were similar in both groups. The demographic characteristics and distribution of the patients across various parameters are shown in Table 1.
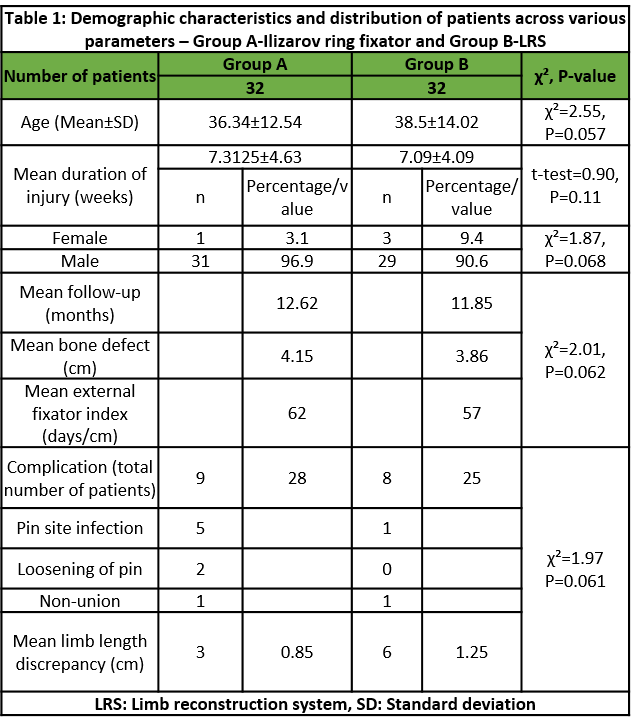
Table 1: Demographic characteristics and distribution of patients across various parameters – Group A-Ilizarov ring fixator and Group B-LRS
In Group A, both bone and functional outcomes improved over time. Excellent bone results increased from 31.3% at 3 months to 43.8% at final follow-up, while poor results disappeared after 6 months. Functional scores also improved, with excellent outcomes rising from 12.5% to 37.5% by 9 months or final follow-up (P = 0.026 for bone, P = 0.014 for function). In Group A, good to excellent bone results were achieved in 90.7% and good to excellent functional results were achieved in 84.4% patients (Table 2).
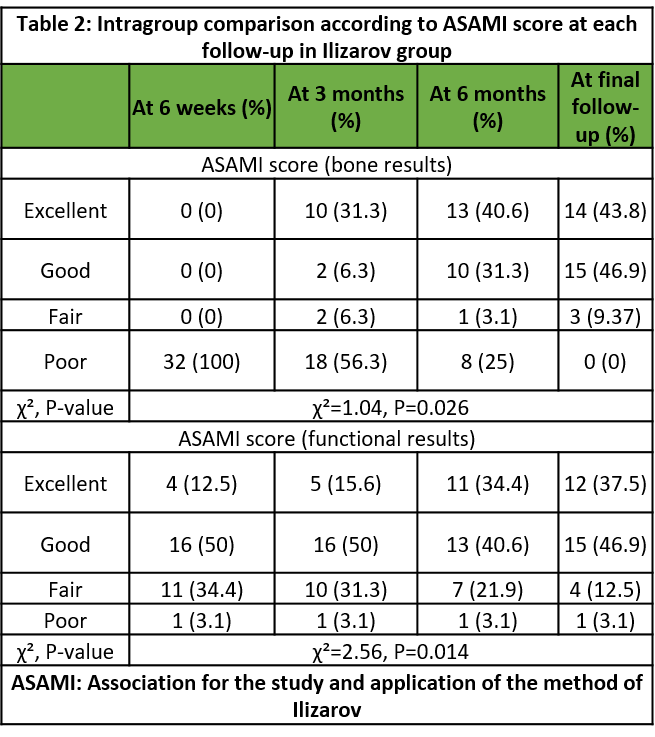
Table 2: Intragroup comparison according to ASAMI score at each follow-up in Ilizarov group
In Group B, bone results improved progressively with excellent outcomes rising from 28.1% at 3 months to 37.5% at final follow-up, and poor results disappeared after 6 months (P = 0.04). Functional outcomes also showed steady improvement, with excellent scores increasing from 6.3% to 28.1% over time and poor results reduced from 15.6% to 3.1% (P = 0.018). In Group B, good to excellent bone results were achieved in 87.5% and good to excellent functional results were achieved in 71.9% patients (Table 3).
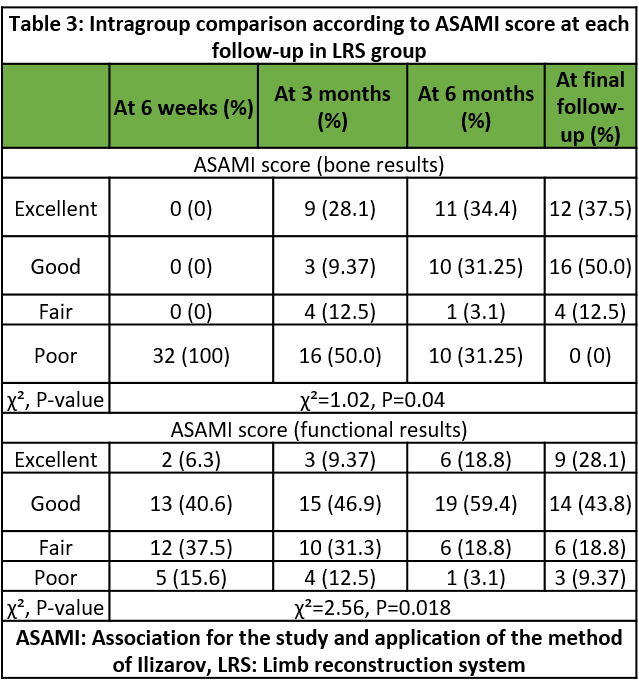
Table 3: Intragroup comparison according to ASAMI score at each follow-up in LRS group
Intergroup comparison revealed that both groups showed progressive improvement in ASAMI bone and functional scores over time. At each follow-up, Group A (Ilizarov) consistently showed slightly better bone and functional outcomes than Group B (LRS). Significant differences were noted in functional results at all-time points (P < 0.05), while bone results became statistically significant from the 3-month mark onwards, with Group A demonstrating a trend toward superior outcomes (Table 4).
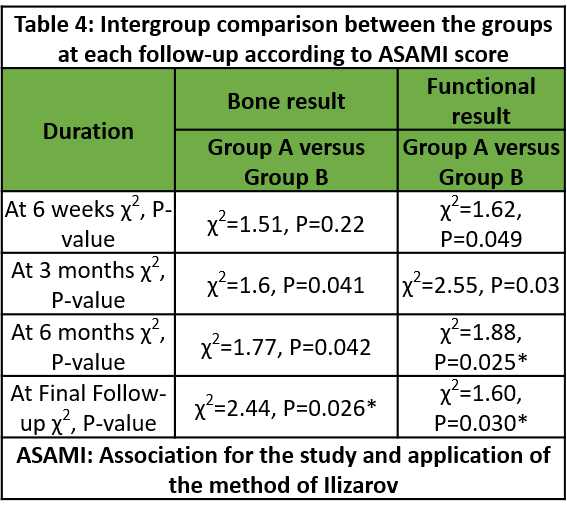
Table 4: Intergroup comparison between the groups at each follow-up according to ASAMI score
In Group A (Ilizarov ring fixator), there was a statistically significant improvement in both callus diameter and density over time. Callus diameter showed progressive maturation, with scores shifting from predominantly score 1 at 6 weeks to higher scores (4 and 5) by final follow-up in 87.5% of patients (χ2 = 1.12, P = 0.004*). Similarly, callus density also improved, with an early predominance of lower scores transitioning to higher scores by 6–9 months or final follow-up in 90.65% (χ2 = 1.68, P = 0.035*), indicating effective bone healing in Group B (LRS), both callus diameter and callus density showed statistically significant progression over time. Initially, the majority had lower diameter scores (1 and 2), which gradually shifted to higher scores (4 and 5) by final follow-up in 81.3% of patients (χ2 = 1.2, P = 0.030). Similarly, callus density improved from predominantly score 2 at 6 weeks to scores 3 and 4 by final follow-up in 84.37% of patients (χ2 = 2.0, P = 0.043), indicating a steady enhancement in bone healing throughout the follow-up period (Table 5).
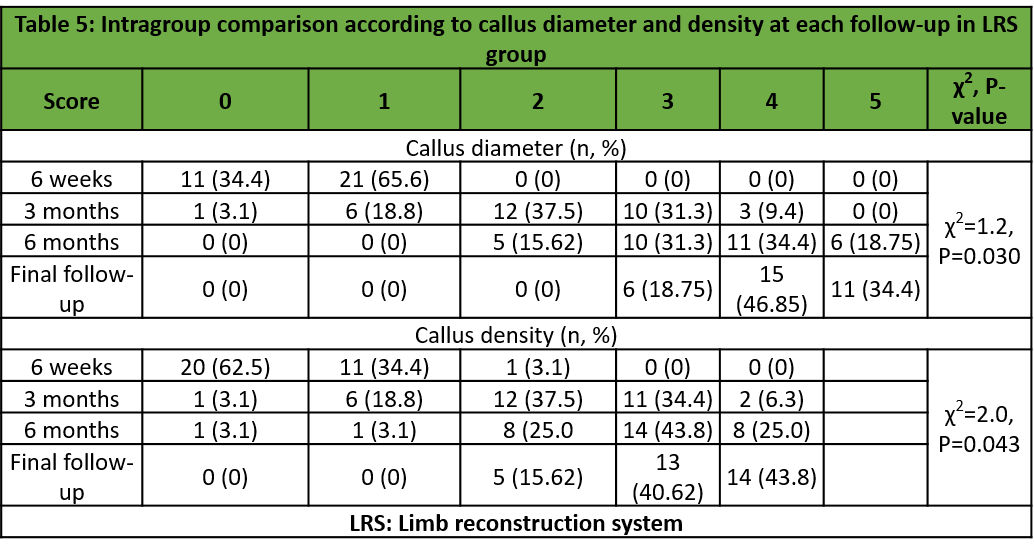
Table 5: Intragroup comparison according to callus diameter and density at each follow-up in LRS group
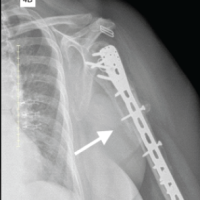
Among the study patients, external fixation was achieved either with the Ilizarov ring fixator or the LRS. A representative case from the Ilizarov group is illustrated in Fig. 1, while two patients treated with the LRS fixator is shown in Fig. 2 and 3.
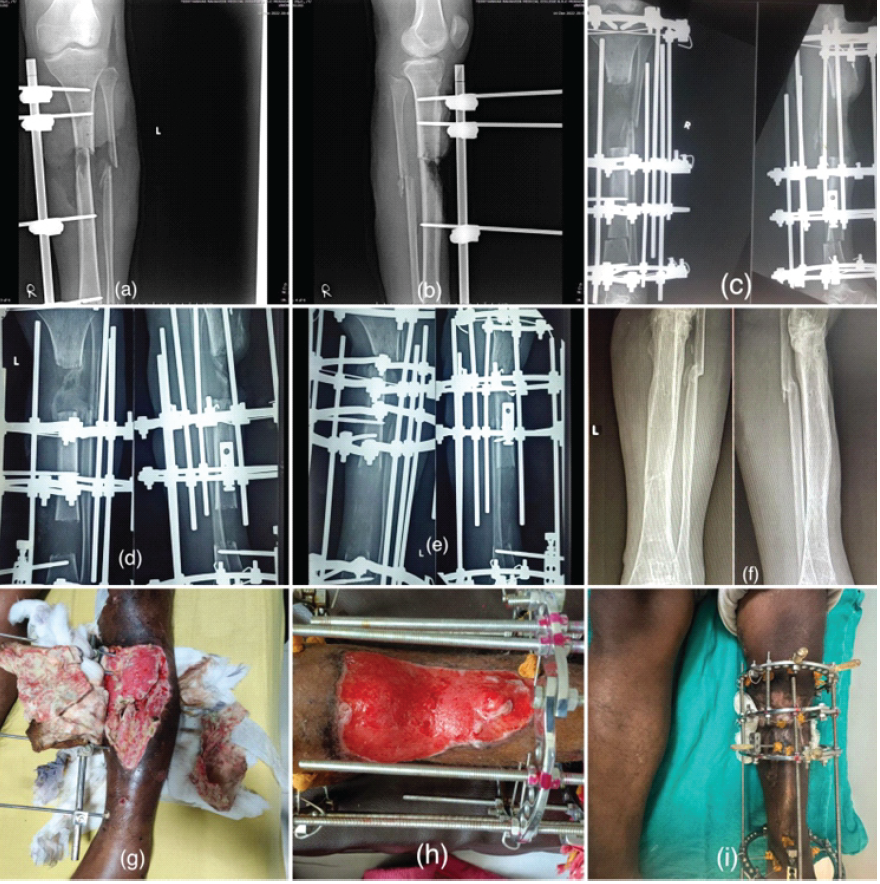
Figure 1: 40-year-old male with compound Grade III B diaphyseal fracture of both bone leg presenting after 4 weeks of injury (a and b) anteroposterior and lateral radiographs at presentation. (c) Immediate post-operative radiograph of leg after application of Ilizarov ring fixator with corticotomy (d and e) sequential radiographs at 3 months and 9 months follow-up showing regenerate formation and completion of distraction. (f) Radiograph after removal of Ilizarov ring fixator showing sound union and consolidated regenerate. (g) Wound at presentation. (h) Healthy granulation of the wound after 1 month. (i) Healed wound after 3 months with no signs of infection.

Figure 2: 38-year-old male patient with compound Grade III B diaphyseal fracture of both bone leg presenting after 3 weeks of injury (a) anteroposterior and lateral views of the affected limb on presentation (b) immediate post-operative radiograph after application of limb reconstruction system (LRS) with corticotomy. (c, d, e) sequential radiographs at 3, 6, and 9 months follow-up, respectively, showing distraction of the fragment and consolidation of the regenerate. (f) Radiograph after removal of the LRS. (g) Wound at presentation. (h) Healthy Granulation of the wound after 1 month. (i) Wound at 3 months follow-up after surgical release of the incarcerated tissue.
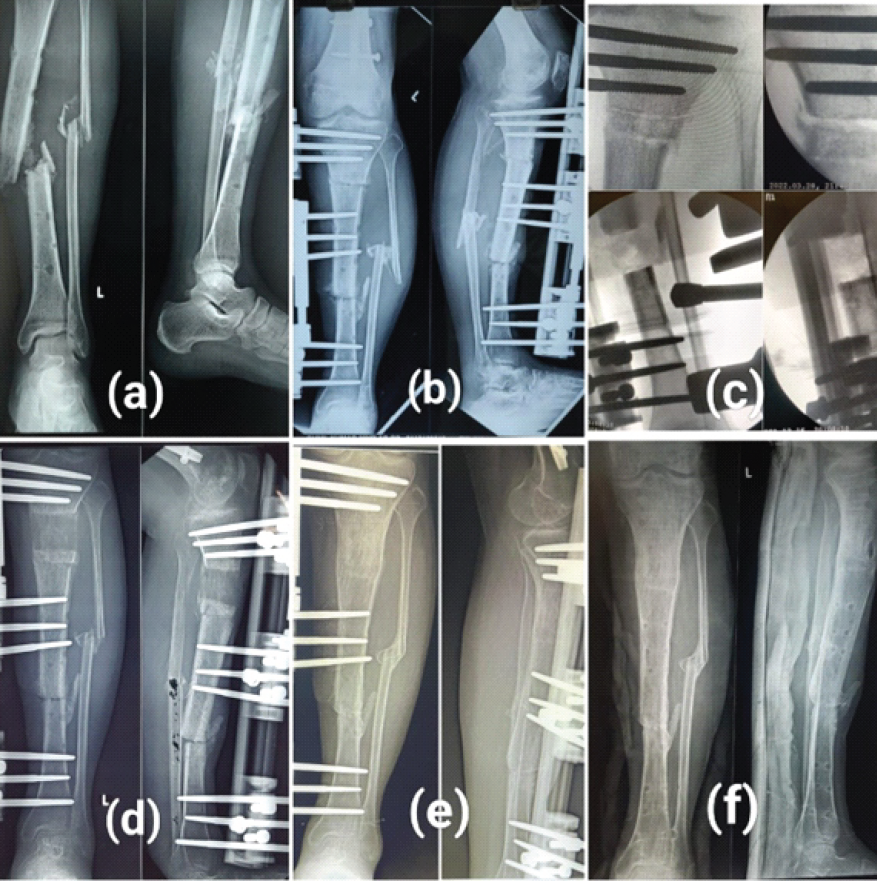
Figure 3: 33-year-old male patient of compound Grade 3B diaphyseal fracture of the tibia and fibula presenting after 4 weeks of injury. (a) Radiograph at presentation (b) radiograph after 1 month of limb reconstruction system (LRS) application and corticotomy. Patient was lost to follow-up resulting in union at the corticotomy site (c) intraoperative images of repeat corticotomy at the proximal tibia and osteotomy of the mid diaphysis of tibia. (d) 3 month follow-up radiograph showing regenerate formation and completion of distraction. (e) 9 months follow-up radiograph showing complete consolidation of the regenerate and union at the compression site (f) final radiograph after LRS removal.
The intergroup comparison showed a statistically significant difference in callus density at 3 months, 6 months, and at final follow-up, with Group A demonstrating better density scores (P = 0.045, 0.049, and 0.031, respectively). Callus diameter also differed significantly at 6 weeks (P = 0.04), favoring Group A, while the differences at 3 months, 6 months, and at final follow-up were not statistically significant. However, Group A consistently exhibited better scores overall. These results indicated that the LRS had provided slightly improved early radiological outcomes compared to the Ilizarov fixator (Table 6).
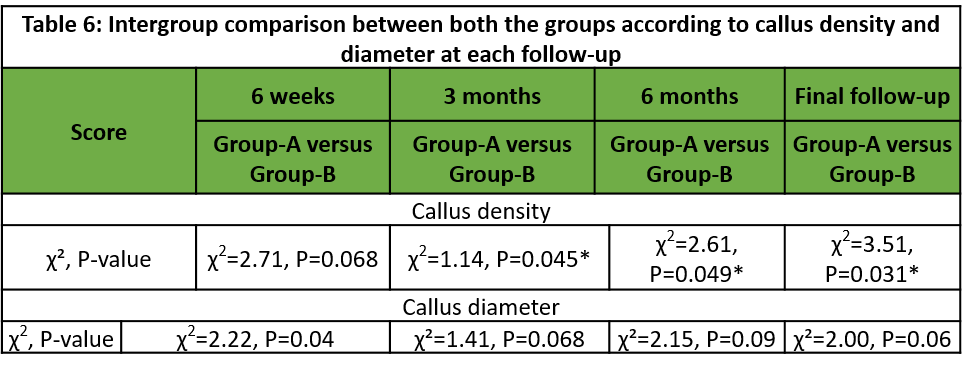
Table 6: Intergroup comparison between both the groups according to callus density and diameter at each follow-up
Seventeen of our patients had post-operative complications (nine in Ilizarov group and eight in LRS group). Six patients developed pin site infection (five in Ilizarov group and one in LRS group) and four of them were treated with meticulous pin site dressing twice daily and a short course of oral antibiotics. Two of those patients in Ilizarov group developed loosening of wire at pin infection site and treated by removal of the loosened wire and addition of a drop/half pin. All the patients achieved sound union except for two patients, one in each group, who landed in nonunion at the docking site and were treated with secondary autologous bone grafting. Limb length discrepancy was found in three patients in the Ilizarov group and six patients in the LRS group with a mean of 0.85 cm and 1.25 cm, respectively (Table 1).
Open tibial fractures are the most common among long bone fractures, largely due to the tibial shaft’s sparse soft-tissue coverage, making it not only difficult to treat but also prone to infection. Effective management aims to prevent infection, preserve limb length, alignment and rotation, minimize further tissue damage, protect circulation, and create an environment favorable for bone healing. External fixation methods, including Ilizarov ring and LRS rail fixators, support these objectives. These techniques, based on distraction histiogenesis, promote bone tissue regeneration through gradual distraction [9,10,11,12]. The mean age in our study was 37 years with a male predominance, similar to a study done by Wani et al. and Nain in our study, excellent radiological as well as functional outcomes showed significant improvement in both the Ilizarov and the LRS group. These findings were like those observed by Pal et al., who also found a significant improvement in radiological and functional outcomes in a similar group of patients treated by the same procedures. We observed good to excellent results in the Ilizarov group in terms of functional as well as radiological outcomes throughout the follow-up period, analogous to the studies done by Wani et al, Nain, and Paley et al. [12,13,14,15]. Pal et al., conducted a similar study on 32 patients of compound diaphyseal tibia fractures with or without infected non-union, to compare the outcomes in Ilizarov and LRS groups and found that the radiological outcome was good to excellent in 87.55% of LRS patients and 75% in Ilizarov fixator patients. The functional results were satisfactory in 75% of LRS group and 68.75% of Ilizarov fixator group. On the contrary, our study showed that radiological/bone results were good to excellent in 90.7% of Ilizarov patients and in 87.5% of LRS patients, functional results were good to excellent in 84.4% of Ilizarov patients and 71.9% of LRS patients. The possible explanation of these results may be that in multiple patients of our LRS group, early docking was performed without achieving normal limb length due to malalignment of the transported fragment at the docking site which we have avoided in Ilizarov patients with minor adjustments. This mal alignment is due to the curved anatomy of the tibia in the sagittal plane, which led to translation of the transport fragment in its terminal transport stage with relation to the docking site, particularly in cases of smaller distal or proximal fragment [14]. Radiologically, the Ilizarov group showed marked improvements in callus diameter and density, with low initial scores maturing significantly by 9 months or final follow-up. The LRS group also showed improvement, although to a lesser extent, as compared to the Ilizarov group. Li et al., stated that before removing the fixator, surgeons should assess the quality of the regenerate bone using the radiographic appearance of callus and bone mineral density. Tirawanish and Eamsobhana assessed callus diameter and density scores with relation to regenerate quality and its related complications such as subsidence, angulation, and fracture and advocated that the fixator should be removed when the callus in the regenerate zone involves at least 80% of its diameter and has a homogeneous density, that is, score 4 or 5 in diameter and a score of 4 in the density. Hence, a total score of 8 or more is a good way to determine when to remove the fixator. In our study, more than 80% of patients fall in this category, though we have not considered the callus scoring system as a basis for frame removal, but rather to assess the quality of regenerate formation and its consolidation [8,16,17]. Since its inception, Ilizarov remained a terrific and ultimate tool for management in non-union of long bone fractures with high-grade compounding, specially where the potential presence of infection cannot be rule out. In recent decades, LRS and other systems based on distraction histiogenesis have also proved their effectiveness in treating these fractures. These studies collectively affirm the effectiveness of distraction-based fixation systems. Although our study has showed comparatively superior results with the Ilizarov method due to its versatility and high modularity, we have achieved good to excellent results in both Ilizarov and LRS groups. Hence, we advocate both Ilizarov and LRS fixators in high grade, compound diaphyseal fractures of the tibia as a definitive management procedure to prevent patient’s morbidity and financial burden arising from long hospital stays and multiple surgical procedures. Our study had various limitations. First, it was performed on a small sample size and was a single-center-based study, so generalization of the study population may not be possible. The relatively small cohort reduces statistical power and the ability to perform subgroup analyses (e.g., by Gustilo grade or age). Second, lack of surgeon and assessor blinding may have led to observer bias. Furthermore, lack of heterogenecity in aspects such as bone loss, soft-tissue injury, and timing of debridement could have influenced outcomes. Third, functional assessment relied mainly on ASAMI and callus scores, without consideration of patient reported quality of life or return to work measures. Another limitation of the study was that economic evaluation and detailed microbiological analysis of infections were not performed. Finally, surgeon preference in terms of choice of intervention could also have introduced bias. To evaluate complications such as refracture, post-traumatic arthritis and limb function, a long-term follow-up of the patient population is mandatory.
This study has supported the role of distraction histiogenesis in long bone fracture management and demonstrated its effectiveness in high-grade, compound diaphyseal fractures of the tibia using Ilizarov and LRS, particularly in cases where the wound condition is compromised and the viability of the exposed bony fragment is questionable. We have achieved good to excellent results of bony union and functional outcome in most of our patients in both Ilizarov and LRS groups, though Ilizarov scores significantly better. Therefore, we advocate the use of Ilizarov ring fixator and LRS as a valid option in high-grade injuries, being a secure, simple, cost-effective, reliable, and effective method. Considering the excellent functional and radiological outcomes observed, additional prospective studies with larger cohorts from the Indian population are recommended to substantiate and extend these findings.
For orthopedic surgeon’s worldwide, high-grade compound tibia fracture is one of the toughest fractures to achieve sound bone union and a good functional outcome. Careful selection of patients for primary definitive Ilizarov and LRS fixation, by assessing the soft-tissue status and fracture pattern, can optimize patient satisfaction, produce good results, and make the surgeon’s life easier.
References
- 1. Kyrö A, Tunturi T, Soukka A. Conservative treatment of tibial fractures. Results in a series of 163 patients. Ann Chir Gynaecol 1991;80:294-300. [Google Scholar] [PubMed]
- 2. Olson SA. Open fractures of the tibial shaft. Instr Course Lect 1997;46:293-302. [Google Scholar] [PubMed]
- 3. Giannoudis PV, Papakostidis C, Roberts C. A review of the management of open fractures of the tibia and femur. J Bone Joint Surg Br 2006;88:281-9. [Google Scholar] [PubMed]
- 4. Mangukiya HJ, Mahajan NP, Pawar ED, Mane A, Manna J. Functional and radiological outcome in management of compound tibia diaphyseal fracture with AO monolateral fixator versus limb reconstruction system. J Orthop 2018;15:275-81. [Google Scholar] [PubMed]
- 5. Wiss DA, Stetson WB. Unstable fractures of the tibia treated with a reamed intramedullary interlocking nail. Clin Orthop Relat Res 1995;315:56-63. [Google Scholar] [PubMed]
- 6. Henley MB, Chapman JR, Agel J, Harvey EJ, Whorton AM, Swiontkowski MF. Treatment of type II, IIIA, and IIIB open fractures of the tibial shaft: A prospective comparison of unreamed interlocking intramedullary nails and half-pin external fixators. J Orthop Trauma 1998;12:1-7. [Google Scholar] [PubMed]
- 7. Hassankhani EG, Birjandinejad A, Kashani FO, Hassankhani GG. Hybrid external fixation for open severe comminuted fractures of the distal femur. Surg Sci 2013;4:176-83. [Google Scholar] [PubMed]
- 8. Tirawanish P, Eamsobhana P. Prediction of callus subsidence in distraction osteogenesis using callus formation scoring system: Preliminary study. Orthop Surg 2018;10:121-7. [Google Scholar] [PubMed]
- 9. Court-Brown CM, Rimmer S, Prakash U, McQueen MM. The epidemiology of open long bone fractures. Injury 1998;29:529-34. [Google Scholar] [PubMed]
- 10. Esterhai JL Jr., Queenan J. Management of soft tissue wounds associated with type III open fractures. Orthop Clin North Am 1991;22:427-32. [Google Scholar] [PubMed]
- 11. Tucker HL, Kendra JC, Kinnebrew TE. Management of unstable open and closed tibial fractures using the ilizarov method. Clin Orthop Relat Res 1992;280:125-35. [Google Scholar] [PubMed]
- 12. Wani N, Baba A, Kangoo K, Mir M. Role of early ilizarov ring fixator in the definitive management of type II, IIIA and IIIB open tibial shaft fractures. Int Orthop 2011;35:915-23. [Google Scholar] [PubMed]
- 13. Nain G. A study to evaluate the functional and radiological outcome of the ilizarov ring fixator in the treatment of infected non-union fracture shaft of tibia. Int J Orthop Sci 2023;9:24-8. [Google Scholar] [PubMed]
- 14. Pal CP, Kumar H, Kumar D, Dinkar KS, Mittal V, Singh NK. Comparative study of the results of compound tibial shaft fractures treated by ilizarov ring fixators and limb reconstruction system fixators. Chin J Traumatol 2015;18:347-51. [Google Scholar] [PubMed]
- 15. Paley D, Catagni MA, Argnani F, Villa A, Benedetti GB, Cattaneo R. Ilizarov treatment of tibial nonunions with bone loss. Clin Orthop Relat Res 1989;241:146-65. [Google Scholar] [PubMed]
- 16. Li R, Saleh M, Yang L, Coulton L. Radiographic classification of osteogenesis during bone distraction. J Orthop Res 2006;24:339-47. [Google Scholar] [PubMed]
- 17. Lakhani A, Singh D, Singh R. Outcome of rail fixator system in reconstructing bone gap. Indian J Orthop 2014;48:612-6. [Google Scholar] [PubMed]