Medial epicondyle fractures require individualized management – fixation choice (K-wire, screw, or plate) should depend on fragment size, displacement, and patient activity.
Dr. Jaideep Das, Department of Orthopaedics, Grant Government Medical College and Sir JJ Group of Hospitals, Mumbai, India. E-mail: jaideepdas01@gmail.com
Introduction: Medial epicondyle fractures of the humerus, account for ~12–20% of pediatric elbow fractures and are often associated with elbow dislocations. Management is debated, especially for moderately displaced injuries. Conventionally, displaced fractures were sometimes treated non-operatively, yielding acceptable function but high rates of fibrous non-union. Recent evidence shows surgical fixation provides ~9-fold higher union rates without significant differences in long-term pain or nerve function. We present five patients treated with different fixation techniques to highlight management considerations and outcomes.
Case Series: Five patients (ages 15–70; 4 male, 1 female) with acute medial epicondyle fractures (presentation within 2 weeks post trauma) underwent open reduction and internal fixation using varied methods: (1) percutaneous Kirschner-wires (K-wires), (2) a single cannulated cancellous (CC) screw, (3) an antiglide plate, (4) combined K-wire plus screw, and (5) a CC screw. Surgery was performed for displacement >5 mm or instability, in line with current recommendations. Post-operative immobilization ranged 2–4 weeks (shorter for screw fixation, longer for K-wires), followed by physiotherapy. At final follow-up (12–36 months), all fractures united (mean ~12 weeks), and patients resumed full activities. Elbow range of motion was near-normal (flexion ≥130°; one transient 5° extension lag resolved after hardware removal). No growth arrests or chronic instability occurred. Functional outcomes were excellent: Mayo Elbow performance scores 90–100 (mean ~96), and quick disabilities of the arm, shoulder, and hand scores (QuickDASH) indicated minimal disability. No non-union, deep infections, or redislocation were seen, consistent with published results.
Conclusion: Medial epicondyle fractures can be effectively treated with various fixation strategies tailored to fragment size, age, and injury pattern. Rigid fixation (screws, plate) enables early mobilization and reliable union, while K-wires remain useful for smaller apophyseal fragments. All methods in this series restored elbow stability and excellent function. Fixation choice should balance fragment anatomy and potential complications: screws enhance purchase but often require removal, whereas K-wires spare the growth center but necessitate longer immobilization. This series emphasizes that diverse fixation approaches – from K-wires to plating – can achieve excellent outcomes when applied judiciously. Surgical fixation in displaced or unstable cases promotes union and allows early return to activity.
Keywords: Medial epicondyle fracture, antiglide plate, internal fixation, Kirschner-wire, cannulated screw.
Medial epicondyle fractures are avulsion injuries of the medial distal humerus, typically occurring in older children and adolescents (peak ~9–14 years). They represent roughly 12–20% of pediatric elbow fractures and are 4 times more common in boys. Up to 50% are associated with an elbow dislocation, and 15–18% of cases have the fragment incarcerated in the joint [1]. The medial epicondyle is the apophysis giving origin to the forearm flexor–pronator muscles and the ulnar collateral ligament (UCL); thus, these fractures often result from valgus stress mechanisms (e.g. fall on an outstretched hand or a sudden traction during sports), causing the flexor-pronator mass to avulse the apophysis. Patients typically present with medial elbow pain, swelling, and tenderness over the epicondyle. If associated with a dislocation, the elbow may spontaneously reduce, but one must be vigilant for a fragment trapped in the joint and for ulnar nerve injury [2]. Management of medial epicondyle fractures has been historically controversial. A primary debate is the acceptable amount of fragment displacement for non-operative treatment. Measuring displacement on plain radiographs can be imprecise (fragments often displace anteroinferiorly out of the anterior-posterior view). Conventionally, up to 5 mm of displacement was often tolerated for closed treatment with casting. Early long-term studies reported that even markedly displaced fragments can heal with fibrous union, yet still yield good functional outcomes in children [3]. For example, Josefsson and Danielsson (1986) followed 56 unreduced medial epicondyle fractures for 35 years and found that all patients had “good” function despite a 63% non-union rate, with no difference in symptoms between those with bony union and fibrous non-union [4,5]. Such findings fostered a more conservative approach in the past. More recent literature and evolving clinical experience have shifted toward a lower threshold for surgical fixation. The reliability of older data has been questioned given modern athletic demands and the recognition that a persistent non-union could lead to pain or valgus instability in high-level activities. A 2009 systematic review by Kamath et al. demonstrated that operative management confers a significantly higher union rate than casting – the odds of bony union were ~9.3 times greater with surgery [3,6]. Importantly, that review found no difference in final pain scores or ulnar nerve symptoms between operative and non-operative groups, suggesting that many children achieve good functional outcomes either way, but surgery ensures an anatomic union. In today’s young athletes who place high demands on the elbow, a stable bony union is often considered preferable to a fibrous union to reduce the risk of late valgus instability or diminished performance [7,8]. Accordingly, many surgeons now recommend internal fixation for displaced fragments, especially beyond 5 mm, the presence of joint entrapment, marked elbow instability, or in overhead athletes [9]. This trend is supported by studies indicating high rates of return to sports and lower incidence of symptomatic non-union in patients treated with fixation (particularly in competitive athletes). On the other hand, recently, a high-level randomized trial found that cast immobilization can yield comparable short-term outcomes to surgery for certain displaced fractures. Thus, the treatment algorithm is being re-examined, and the decision to operate must weigh the degree of displacement, skeletal maturity, and patient activity level. In summary, controversy persists regarding optimal management of medial epicondyle fractures. The following case series describes five patients, each managed with a different fixation method (Kirschner-wires [K-wires], screw alone, plate, hybrid K-wire + screw, screw), along with their outcomes, and discusses these strategies in the context of current evidence.
We report five cases (ages 15–70; 4 males, 1 female) of medial humeral epicondyle fractures treated at our institution. Patient details are de-identified, and written informed consent was obtained from patients or guardians. Key clinical information is summarized in Table 1.
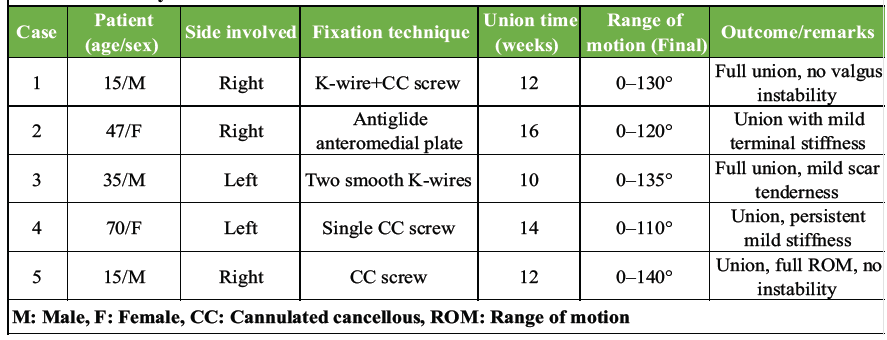
Table 1: Summary of case details and outcomes
All patients sustained an isolated medial epicondyle fracture (no other fractures) and had no prior elbow pathology. Neurovascular status was intact on initial exam in all cases (aside from transient ulnar nerve symptoms in one case). Each case highlights a distinct fixation strategy:
Case 1
(K-Wire with cannulated cancellous [CC] screw) A 15-year-old male sustained an injury while playing cricket following a fall on his outstretched arm. Examination revealed medial swelling, tenderness, and valgus instability, with radiographs confirming a malunited medial epicondyle fracture. Open reduction was performed via a medial approach. Osteotomy was done using a K-wire for temporary stabilization and a CC screw for definitive fixation. At 12 weeks, radiological union was achieved with elbow range of motion (ROM) of 0–130° and no residual instability (Figs. 1 and 2).
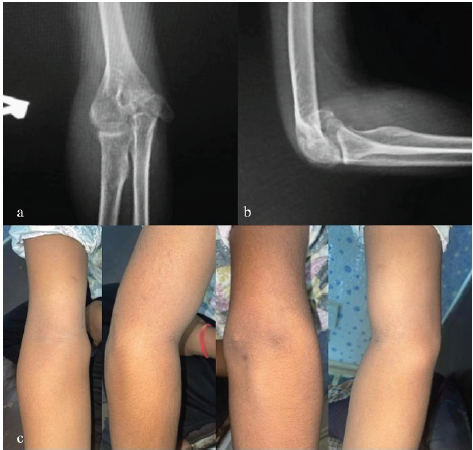
Figure 1: Pre-operative right elbow X-rays and clinical pictures (a) X-ray right elbow anterior-posterior view, (b) X-ray right elbow lateral view, (c) clinical pictures of right elbow.

Figure 2: Pre-operative computed tomography (CT) image, intra-operative clinical picture, and post-operative X-rays (a) CT images of right elbow, (b) intra-operative clinical picture of exposure and osteotomy, (c) post-operative X-ray right elbow anterior-posterior view, (d) post-operative X-ray right elbow lateral view.
Case 2
(Antiglide plate) A 47-year-old female sustained a slip-and-fall at home. Clinical findings included gross swelling, ecchymosis, and painful restriction of motion. Imaging demonstrated a comminuted fracture of the medial epicondyle with extension into the trochlea. Open reduction via an anteromedial approach was followed by fixation with an antiglide plate and screws. By nearly 16 weeks, union was achieved; final ROM was 0–120°, with mild terminal stiffness but functional independence (Fig. 3).
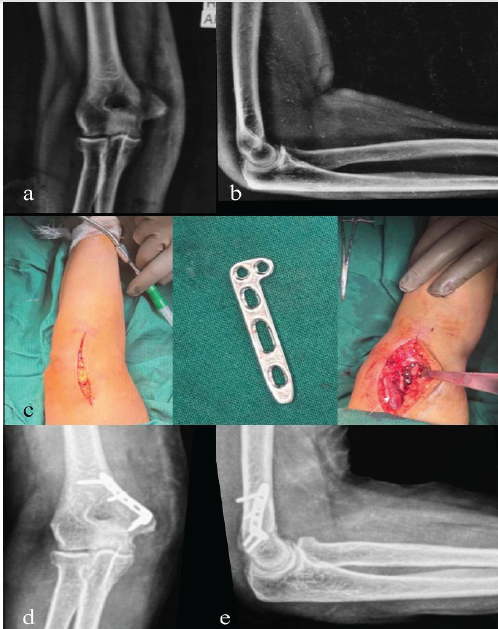
Figure 3: Pre-operative X-rays, intraoperative clinical picture, and post-operative X-rays (a) pre-operative X-ray right elbow anterior-posterior (AP) view, (b) pre-operative X-ray right elbow lateral view, (c) intra-operative clinical pictures of incision, antiglide plate, and plate placement, (d) post-operative X-ray right elbow AP view, (e) post-operative X-ray right elbow lateral view.
Case 3
(K-wire) A 35-year-old male presented after injury by blades of a fan, with contused lacerated wound over elbow with pain, swelling, and restricted motion with a transected ulnar nerve. Radiographs showed a displaced, comminuted medial epicondyle fragment. He underwent open reduction and fixation with two smooth K-wires, along with ulnar nerve repair with graft. At 10 weeks, the wires were removed, and union was confirmed. Final ROM was 0–135°, with only mild scar tenderness reported (Fig. 4).
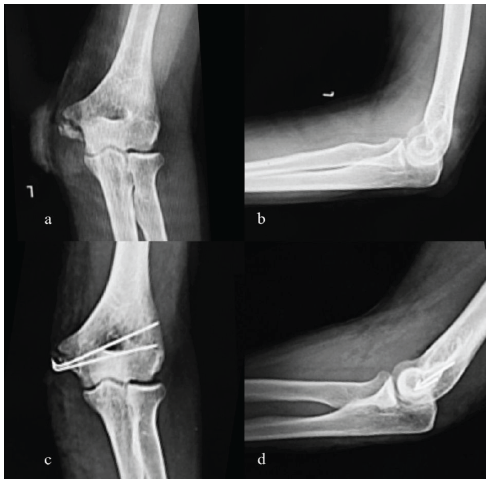
Figure 4: Pre-operative and post-operative X-rays left elbow (a) pre-operative X-ray left elbow anterior-posterior (AP) view, (b) pre-operative X-ray left elbow lateral view, (c) post-operative X-ray left elbow AP view, (d) post-operative X-ray left elbow lateral view.
Case 4
(CC screw) A 70-year-old female sustained fall onto her left elbow. The patient was previously operated with radial head replacement. Examination revealed swelling, pain, and limited flexion. Radiographs demonstrated a large medial epicondyle fragment and a radial head implant. The fracture was fixed with a single 4.5 mm CC screw after anatomical reduction. Union was evident at 14 weeks; she regained a 0–110° arc of motion, with mild persistent stiffness but independence in daily activities (Fig. 5).
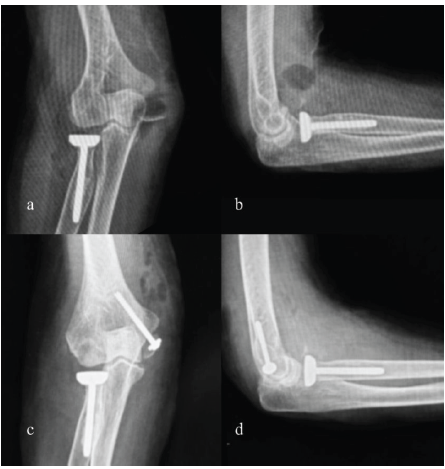
Figure 5: Pre-operative and post-operative X-rays right elbow (a) pre-operative X-ray right elbow anterior-posterior (AP) view, (b) pre-operative X-ray right elbow lateral view, (c) post-operative X-ray right elbow AP view, (d) post-operative X-ray right elbow lateral view.
Case 5
(CC screw) A 15-year-old sustained a valgus stress injury. Clinical findings included medial tenderness and valgus instability. Radiographs revealed a displaced medial epicondyle fragment with intra-articular entrapment. Open reduction was performed, and fixation achieved with a 4.0 mm CC screw. By 12 weeks, union was achieved with full ROM (0–140°), no instability, and return to sport. Across all cases, radiographic union occurred within 10–16 weeks (mean ~12 weeks). Final functional outcomes were excellent, with restoration of elbow stability and satisfactory ROM in each patient. No major complications such as non-union, deep infection, or ulnar nerve dysfunction were observed (Fig. 6).

Figure 6: Pre-operative and post-operative X-rays left elbow (a) pre-operative X-ray left elbow anterior-posterior (AP) view, (b) pre-operative X-ray left elbow lateral view, (c) post-operative X-ray left elbow AP view, (d) post-operative X-ray left elbow lateral view.
Across all five cases, outcomes were uniformly excellent. Radiographic union was achieved in all patients by a median of ~12 weeks (range 10–16 weeks), with no non-union. Alignment and carrying angle were preserved, and no growth disturbances occurred (Table 1). Elbow motion was near normal in all patients. Four regained full extension; Case 3 had a mild 5° extension lag that resolved after hardware removal. Flexion ranged 130–140°, and forearm rotation was normal in all. These findings align with the literature noting that minor loss of terminal extension is the most common residual deficit. Functional outcomes were excellent. Mean Mayo elbow performance score (MEPS) was 96/100 (range 90–100), with four “excellent” and one “good.” quick disabilities of the arm, shoulder, and hand (QuickDASH) scores (three cases) were 0, 0, and 5, reflecting minimal disability. All patients returned to pre-injury activity levels; three resumed competitive sports (Cases 1, 2, 5), while the other two returned to full recreational activity by 6–9 months. Complications were minor. No intraoperative issues, deep infections, or permanent ulnar nerve injuries occurred. One patient (Case 4) had superficial pin-site irritation, resolved with removal. Two patients required elective hardware removal for prominence (Case 5: Screw; Case 3: Plate). All elbows were stable to valgus stress, with no residual medial laxity or subjective instability. Although our series lacks a non-operative comparison group, recent trials suggest that casting can yield comparable functional outcomes in selected displaced fractures [4]. However, all our cases had clear surgical indications, including substantial displacement, intra-articular fragments, or high-demand athletic goals. Our findings demonstrate that, when appropriately indicated, surgical fixation – whether K-wires, screws, plates, or hybrid constructs – results in reliable union, restoration of stability, and excellent function.
Management of medial epicondyle fractures should be individualized based on fragment size, displacement, skeletal maturity, and patient activity [10]. The most common mechanism of injury is an avulsion fracture that occurs as usually after a fall as a result of a valgus stress being placed on the extended elbow. The origin of the UCL at the medial epicondylar apophysis, if put under valgus stress, avulses it. It can also occur due to a pure avulsion by the forearm flexors and rarely with a direct blow to the elbow. If there is a complete fracture, the avulsed apophysis will displace distally due to pull of the forearm flexor mass originating on it [11]. Our case series illustrates the spectrum of fixation techniques, each with specific indications and advantages.
K-wire fixation
Smooth K-wires offer a minimally invasive option, particularly for small apophyseal fragments in younger children. They provide stable fixation when screws cannot be securely placed. Wires require a period of immobilization and eventual removal to avoid pin migration, and prolonged casting can contribute to stiffness. In our series, early wire removal at 3 weeks facilitated motion, and no complications occurred. Literature supports K-wire use in pediatric cases, showing high union rates and excellent long-term function.
CC screw fixation
Cannulated screws are preferred for larger fragments, providing rigid interfragmentary compression that allows early mobilization. Case 4 in our series achieved solid union and full function. Key technical considerations include selecting an appropriate screw size, avoiding joint protrusion, and protecting the ulnar nerve. Screws restore bony continuity and soft-tissue attachment, and studies report high union rates and excellent functional outcomes, including early return to sport.
Plate fixation
Plating is uncommon for medial epicondyle fractures but can be valuable for comminuted or complex fragments, as in Case 2. Plates allow stabilization when single-point fixation is insufficient, particularly in older adolescents or adults. Hardware removal may be necessary due to prominence or motion limitation, but plates can restore stability in challenging fracture patterns.
Hybrid fixation (K-wire plus screw)
Combining devices can address unique fracture characteristics. In Case 1, a K-wire provided anti-rotational support while the screw ensured compression. Hybrid approaches may also include tension-band wiring or suture anchors in selected cases, particularly when soft-tissue attachments require augmentation. This allows surgeons to tailor fixation to fragment anatomy and biomechanical needs, ensuring union and stability.
Non-operative management
Conservative treatment remains appropriate for minimally displaced fractures (<5 mm), particularly in skeletally immature patients without ulnar nerve symptoms or instability. Immobilization in an above-elbow cast for 3–4 weeks typically results in satisfactory healing and function. However, close radiographic monitoring is necessary to ensure fragment stability. Some studies suggest that fibrous union may be functionally adequate in low-demand patients, but displaced fragments or those associated with elbow instability, valgus laxity, or ulnar nerve symptoms generally require operative intervention. Conservative cases healed uneventfully with good ROM, reinforcing that patient selection is critical. Medial epicondyle fractures require individualized management; there is no “one-size-fits-all” approach. K-wires are suitable for small fragments in skeletally immature patients, screws provide rigid fixation for larger fragments, plates stabilize comminuted patterns, and hybrid constructs address complex configurations. Careful implant selection, attention to soft-tissue attachments, and timely post-operative mobilization are critical for restoring function and minimizing complications. Early rehabilitation is essential. Motion was initiated as soon as fixation allowed: 1–2 weeks for screws and plates, and 3–4 weeks for K-wire cases after removal. Immobilization beyond 4 weeks was avoided to prevent stiffness. All patients achieved near-normal elbow motion. Functional outcomes were excellent. Mean MEPS was 96/100, QuickDASH scores were minimal, and all patients returned to pre-injury activities, including competitive sports in three cases. Complications were minor: One superficial pin-site irritation and two elective hardware removals for prominence. No deep infections, permanent nerve injuries, or non-unions occurred, and all elbows were stable to valgus stress. Our findings align with the literature showing high union rates and reliable functional recovery after open reduction and internal fixation. While non-operative management may yield comparable function in selected cases, surgical fixation provides predictable union and stability, particularly for active patients, those with displacement >5 mm, incarcerated fragments, or elbow instability. Anatomic fixation also minimizes the risk of late valgus instability in high-demand athletes
Medial epicondyle fractures can be effectively treated using different fixation techniques when management is individualized to fracture characteristics and patient demands. In this series, all fixation methods achieved reliable union, restored elbow stability, near-normal ROM, excellent functional scores (MEPS/QuickDASH), and return to pre-injury activity levels, emphasizing the importance of appropriate implant selection based on fragment size, displacement, and activity level.
Medial epicondyle fractures require individualized management. The choice of fixation – K-wires, cannulated screws, or plates – should be guided by fragment size, displacement, skeletal maturity, and patient activity level to achieve stable union and excellent functional outcomes.
References
- 1. Pathy R, Dodwell ER. Medial epicondyle fractures in children. Curr Opin Pediatr 2015;27:58-66. [Google Scholar] [PubMed]
- 2. Cruz AI Jr., Steere JT, Lawrence JT. Medial epicondyle fractures in the pediatric overhead athlete. J Pediatr Orthop 2016;36 Suppl 1:S56-62. [Google Scholar] [PubMed]
- 3. Kamath AF, Baldwin K, Horneff J, Hosalkar HS. Operative versus non-operative management of pediatric medial epicondyle fractures: A systematic review. J Child Orthop 2009;3:345-57. [Google Scholar] [PubMed]
- 4. Josefsson PO, Danielsson LG. Epicondylar elbow fracture in children. 35-year follow-up of 56 unreduced cases. Acta Orthop Scand 1986;57:313-5. [Google Scholar] [PubMed]
- 5. Grahn P, Helenius I, Hämäläinen T, Kivisaari R, Nietosvaara Y, Sinikumpu JJ, et al. Casting vs surgical treatment of children with medial epicondyle fractures: A randomized clinical trial. JAMA Netw Open 2025;8:e258479. [Google Scholar] [PubMed]
- 6. Patel NM, Ganley TJ. Medial epicondyle fractures of the humerus: How to evaluate and when to operate. J Pediatr Orthop 2012;32 Suppl 1:S10-3. [Google Scholar] [PubMed]
- 7. Hines RF, Herndon WA, Evans JP. Operative treatment of medial epicondyle fractures in children. Clin Orthop Relat Res 1987;223:170-4. [Google Scholar] [PubMed]
- 8. Lawrence JT, Patel NM, Macknin J, Flynn JM, Ganley TJ, Cameron D, et al. Return to competitive sports after medial epicondyle fractures in adolescent athletes: Results of operative and nonoperative treatment. Am J Sports Med 2013;41:1152-7. [Google Scholar] [PubMed]
- 9. Kamath AF, Cody SR, Hosalkar HS. Open reduction of medial epicondyle fractures: Operative tips for technical ease. J Child Orthop 2009;3:331-6. [Google Scholar] [PubMed]
- 10. Lu Y, Canavese F, Xia Y, Lin R, Huang D, Chen T, et al. Diagnosis and treatment of “medial to lateral diagonal injury of the elbow” in children: Concomitant medial epicondylar and radial neck fractures. J Child Orthop 2023;17:339-47. [Google Scholar] [PubMed]
- 11. Azar FM, Beaty JH, Canale ST, Campbell WC. Campbell’s Operative Orthopaedics. Amsterdam: Elsevier; 2021. [Google Scholar] [PubMed]