Vascular status should be critically assessed even in simple looking pure type 1 Salter-Harris physeal injuries.
Dr. Nishant Bhatia,
Department of Orthopaedic Surgery,
Maulana Azad Medical College and Associated Lok Nayak Hospital,
New Delhi, India.
E-mail: bhatianishant1111@gmail.com
Introduction: Physeal injuries of proximal tibia are uncommon and constitute only 1% of all physeal injuries. Major vessel injuries are also rare in children and occur in 0.6% trauma cases, out of which, injuries of popliteal artery comprise only 5%. The combination of these is an extremely rare injury pattern but is potentially limb threatening. Most of the cases of physeal injuries of proximal tibia along with popliteal artery compromise, reported in the literature include Salter Harris (SH) type II, III, and IV patterns (type II being most common) with pure type I being extremely rare.
Case Report: We describe a rare posteriorly displaced pure SH I injury of proximal tibial physis with compromised vascularity of the limb. Immediate closed reduction and stabilization with Kirschner wires (K-wires) restored the vascularity of the limb and the patient went on to have a good functional recovery at the last follow-up of 1 year.
Conclusion: Vascular injuries occurring in SH 1 proximal tibial physeal fractures are often overlooked or missed due to the relatively benign appearance of slip with no sharp fragments to injure major vessels. Close monitoring of neurovascular status and a low threshold for fixation, for example, with K-wires, are important to prevent limb threatening ischemia in these relatively simple appearing injuries.
Keywords: Hyperextension injury, physeal injury, proximal tibia, Salter-Harris 1, vascular injury.
Physeal injuries of proximal tibia are uncommon and constitute only 1% of all physeal injuries [1]. The rarity of this part for fracture is due to the fact that the periphery of the epiphysis is free of any ligamentous attachments. The collateral and capsular ligaments are attached on metaphysis, distal to the physis thus shielding the epiphysis from severe forces. Moreover, the physis buttresses laterally on the upper fibular end which further adds to the stability [2]. The injury mechanism determines the type of fracture, with type II Salter Harris (SH) injury being most common. A hyperextension injury causes the metaphyseal fragment to displace posteriorly while a flexion injury causes the epiphyseal fragment to displace posteriorly [3, 4]. These injuries can be very disastrous for the limb, due to hampered vascularity or compartment syndrome [5]. The vascular injury rate in these cases has been reported to be as high as 10% with popliteal artery being most commonly involved [6]. Thrombosis or laceration of the popliteal artery usually occurs in the part lying immediately distal to the physis as the vessel is relatively fixed to tibia in this region. Most of the cases of physeal injuries of proximal tibia along with popliteal artery compromise, reported in literature include SH type II, III, and IV patterns (type II being most common) with pure type I being extremely rare [7, 8, 9]. In this report, we describe a rare posteriorly displaced pure SH I injury of proximal tibial physis with compromised vascularity of the limb. Immediate closed reduction and stabilization with Kirschner wires (K-wires) restored the vascularity of the limb and the patient went on to have a good functional recovery at the last follow-up of 1 year.
A 12-year-old boy came to us in emergency department with an injury to his left leg in the form of a direct impact to the anterior aspect of his proximal leg from an oncoming biker who was driving on the wrong side of the road. He was not able to put weight on the injured limb and had to be carried to the hospital. Examination showed a gross swelling in his knee region and posterior sag in his left leg, with a visible step distal to the joint line. There were some bruises and marked tenderness was present in the proximal tibial region. The calf had no tenderness and was soft on palpation; however, the periphery was relatively cold with absent peripheral pulses and, delayed pin prick, and capillary refilling time. He did not have any motor or sensory deficit in the limb.
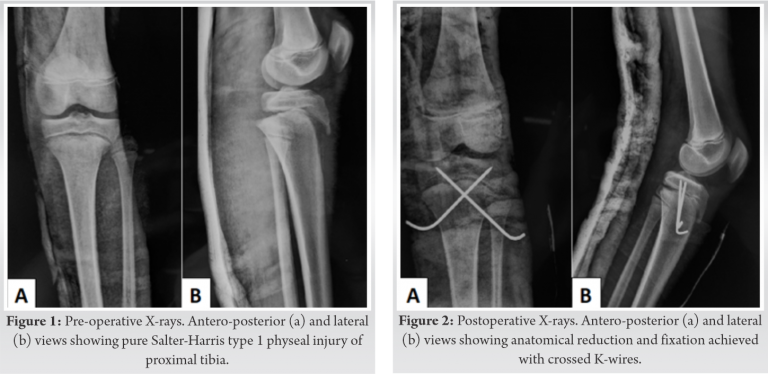
Radiographs revealed SH I proximal tibial physeal injury with posteriorly displaced tibial metaphysis (Fig. 1). Doppler sonography revealed a monophasic flow in the anterior tibial, posterior tibial, and dorsalis pedis arteries. The flow was normal above the level of the injury.
He was shifted to the operating room within 45 min of presentation. Under general anesthesia, in supine position, the fracture was reduced in a closed manner with traction and extension followed by flexion at the fracture site. Care was taken not to hyperextend or hyperflex the limb at any time during the maneuver. The reduction was held with two thick smooth K-wires in a crossed configuration (Fig. 2). The patient’s peripheral pulses had returned by the time the fixation was completed and hence the circulation was restored. Pin prick bleeding and capillary refill time returned back to normal. This was confirmed with a portable Doppler which showed biphasic flow in the peripheral arteries. Patient’s knee was immobilized in an above knee plaster cast. The post-operative period was uneventful except that the patient developed some blisters in the proximal leg on the 3rd postoperative day; however, there were no signs of any neurovascular compromise. The blisters were punctured, painted with Povidone-iodine and dressed in a dry manner. The skin healed well in a few days and the patient was discharged. The cast was removed at 3 weeks following which knee range of motion was started and the K-wires were removed at 6 weeks. Weight bearing was allowed at 3 months and gradually progressed as tolerable. Radiological healing was seen at 4 months (Fig. 3). At the last follow-up of 1 year, the patient had a good knee range of motion (ROM), no limb length discrepancy or deformity and was able to squat and sit cross legged without any difficulty.
Major vessel injuries are rare in children and occur in 0.6% trauma cases, out of which, injuries of popliteal artery comprise only 5% [10, 11]. Physeal injuries of proximal tibia are also uncommon and constitute only 1% of all physeal injuries [10]. The combination of these is an extremely rare injury pattern. Among all the physeal injuries of proximal tibia, about 7–10% can have compromised vascularity [6, 12]. Hyperextension (with or without valgus strain) resulting in posterior displacement of the shaft is the commonest mechanism in proximal tibial physeal injuries [3, 4]. Our patient had a similar mechanism with direct blow on the proximal tibia causing the shaft to translate posteriorly, separating at the physis which is the weak link between the metaphysis and epiphysis. Most of the reported series show that type II (SH) physeal injuries are the most common pattern resulting from hyperextension [7, 8, 9]; however, the case reported here had a pure type I physeal injury probably resulting from the direct impact on anterior aspect rather than a force acting from posterior to anterior direction causing hyperextension. (Table 1) summarizes some major case series on proximal tibial physeal injuries and outlines those presenting with vascular compromise [13, 14, 15, 16, 17]. Undisplaced physeal injuries can be treated in a plaster cast. Closed reduction and fixation with cross pins can be done for SH I and II injuries with displacement. An unacceptable reduction with >2 mm residual displacement or an irreducible fracture warrant an open reduction and release of interposed ligaments, pes tendons, or periosteum. Displaced SH III and IV injuries should be managed with open reduction and internal fixation with screws and pins in epiphysis and metaphysis while avoiding crossing the physis [18]. In an associated vascular injury, reassessment should always be done after an attempted reduction with a vascular surgeon on stand-by. A computed tomography (CT) angiogram is the best investigation to assess the vascular insult/restoration; however, a Doppler sonogram may do the job if there is no time to spare. If the vascularity is not restored following reduction, the popliteal artery should be explored [1, 4, 5]. In our case, our vascular surgeon colleague was asked to be on stand-by in case, the vascularity was not restored after reduction. Compartment syndrome may be an associated problem at the time of presentation. It may be due to the fracture itself [14] or a vascular insult evolving into compartment syndrome. An urgent fasciotomy is needed with or without vascular exploration depending on the pre-operative Doppler and CT angiography. Physeal injuries of proximal tibia can result in growth disturbances in up to 25% of cases. Frequent full length radiographs should be obtained in follow-up till skeletal maturity so as to recognize evolving growth disturbance or deformity. Ligamentous injuries should also be assessed following stabilization [19]. Common peroneal nerve (CPN) palsy is a common occurrence with these injuries and a careful neurological examination should always be done to detect it. Our patient did not have any associated compartment syndrome or CPN palsy. He went on to have a good recovery with no growth disturbance/deformity and excellent function at the last follow-up. Our case highlights two important aspects, first, a pure type I physeal injury of proximal tibia with vascular compromise is a rare entity and second that excellent results can be achieved with timely intervention.
Vascular injuries occurring in SH 1 proximal tibial physeal fractures are often overlooked or missed due to the relatively benign appearance of slip with no sharp fragments to injure major vessels. Close monitoring of neurovascular status and a low threshold for fixation, for example, with K-wires, are important to prevent limb threatening ischemia in these relatively simple appearing injuries.
A pure type I physeal injury of proximal tibia with vascular compromise is a rare entity but excellent results can be achieved with timely intervention provided that the vascular injury is not missed.
References
- 1.Peterson HA, Madhok R, Benson JT, Ilstrup DM, Melton LJ 3rd. Physeal fractures: Part 1. Epidemiology in Olmsted County, Minnesota, 1979-1988. J Pediatr Orthop 1994;14:423-30. [Google Scholar]
- 2.Mubarak SJ, Kim JR, Edmonds EW, Pring ME, Bastrom TP. Classification of proximal tibial fractures in children. J Child Orthop 2009;3:191-7. [Google Scholar]
- 3.Vyas S, Ebramzadeh E, Behrend C, Silva M, Zionts LE. Flexion-type fractures of the proximal tibial physis: A report of five cases and review of the literature. J Pediatr Orthop B 2010;19:492-6. [Google Scholar]
- 4.Zionts LE. Fractures around the knee in children. J Am Acad Orthop Surg 2002;10:345-55. [Google Scholar]
- 5.Wozasek GE, Moser KD, Haller H, Capousek M. Trauma involving the proximal tibial epiphysis. Arch Orthop Trauma Surg 1991;110:301-6. [Google Scholar]
- 6.Beaty JH, Kasser JR. Rockwood and Wilkins’ Fractures in Children. 5th ed. Philadelphia, PA: Lippincott; 2001. p. 1011-9. [Google Scholar]
- 7.Burkhart SS, Peterson HA. Fractures of the proximal tibial epiphysis. J Bone Joint Surg Am 1979;61:996-1002. [Google Scholar]
- 8.Poulsen TD, Skak SV, Toftgaard T. Epiphyseal fractures of the proximal tibia. Injury 1989;20:111-3. [Google Scholar]
- 9.Gautier E, Ziran BH, Egger B, Slongo T, Jakob RP. Growth disturbances after injuries of the proximal tibial epiphysis. Arch Orthop Trauma Surg 1998;118:37-41. [Google Scholar]
- 10.Barmparas G, Inaba K, Talving P, David JS, Lam L, Plurad D, et al. Pediatric vs adult vascular trauma: A national trauma databank review. J Pediatr Surg 2010;45:1404-12. [Google Scholar]
- 11.Reed MK, Lowry PA, Myers SI. Successful repair of pediatric popliteal artery trauma. Am J Surg 1990;160:287-90. [Google Scholar]
- 12.McGuigan JA, O’Reilly MJ, Nixon JR. Popliteal arterial thrombosis resulting from disruption of the upper tibial epiphysis. Injury 1984;16:49-50. [Google Scholar]
- 13.Shelton WR, Canale ST. Fractures of the tibia through the proximal tibial epiphyseal cartilage. J Bone Joint Surg Am 1979;61:167-73. [Google Scholar]
- 14.Clement ND, Goswami A. Salter-Harris II injury of the proximal tibial epiphysis with both vascular compromise and compartment syndrome: A case report. J Orthop Surg Res 2009;4:23. [Google Scholar]
- 15.Guled U, Gopinathan NR, Goni VG, Rhh A, John R, Behera P. Proximal tibial and fibular physeal fracture causing popliteal artery injury and peroneal nerve injury: A case report and review of literature. Chin J Traumatol 2015;18:238-40. [Google Scholar]
- 16.Alshammari D, Alhefzi A, Bund L, Schneider L, Gicquel P. Popliteal artery dissection presented 12 hours after admission for a salter III fracture of proximal tibia. Acta Orthop Belg 2016;82:918-22. [Google Scholar]
- 17.Shinomiya R, Sunagawa T, Nakashima Y, Nakabayashi A, Makitsubo M, Adachi N. Slow progressive popliteal artery insufficiency after neglected proximal tibial physeal fracture: A case report. J Pediatr Orthop B 2018;27:35-9. [Google Scholar]
- 18.Mayer S, Albright JC, Stoneback JW. Pediatric knee dislocations and physeal fractures about the knee. J Am Acad Orthop Surg 2015;23:571-80. [Google Scholar]
- 19.Vrettakos AN, Evaggelidis DC, Kyrkos MJ, Tsatsos AV, Nenopoulos A, Beslikas T. Lower limb deformity following proximal tibia physeal injury: Long term follow-up. J Orthop Traumatol 2012;13:7-11. [Google Scholar]