[box type=”bio”] What to Learn from this Article?[/box]
Septic arthritis can presents as stiff shoulders in immunocompromised patients.
Case Report | Volume 6 | Issue 2 | JOCR April-June 2016 | Page 31-33 | Senthil Nathan Sambandam, Mukesh Atturu. DOI: 10.13107/jocr.2250-0685.418
Authors: Senthil Nathan Sambandam[1], Mukesh Atturu[1].
[1] Department of Orthopaedics, K.G hospital and P.G medical institute, Coimbatore. India.
Address of Correspondence
Dr. Mukesh Atturu,
Orthopaedics resident, K.G hospital and P.G medical institute, Arts college road, Coimbatore, Tamilnadu. India- 641018.
E-mail: kghors@gmail.com
Abstract
Introduction: Septic arthritis of the shoulder is uncommon in adults. It is a surgical emergency as joint destruction occurs rapidly and can lead to significant morbidity and mortality. Accurate diagnosis can be particularly challenging in patients with underlying liver disease. MRI is a useful adjunct in early detection of atypical causes of shoulder pain.
Case report: A 43-year-old male came to our outpatient department with complaints of pain and stiffness of his left shoulder. On examination, his shoulder movements were severely restricted. Further evaluation with MRI revealed septic arthritis of left gleno-humeral joint for which emergency arthroscopic debridement was done.
Conclusion: Septic arthritis of shoulder may not present with classical clinical features. Hence, a through clinical and radiological evaluation will help us prognosticate and treat accordingly thereby preventing complications like septic shock, osteomyelitis.
Key Words: Arthritis, Shoulder joint, stiffness.
Introduction
Patients with septic arthritis usually develop moderate to severe joint pain, warmth, tenderness, effusion, restricted active and passive motion, and sometimes redness. We report an unusual presentation of shoulder septic arthritis in a 43 years old man with no other clinical signs and symptoms of classical septic arthritis.
Case Report
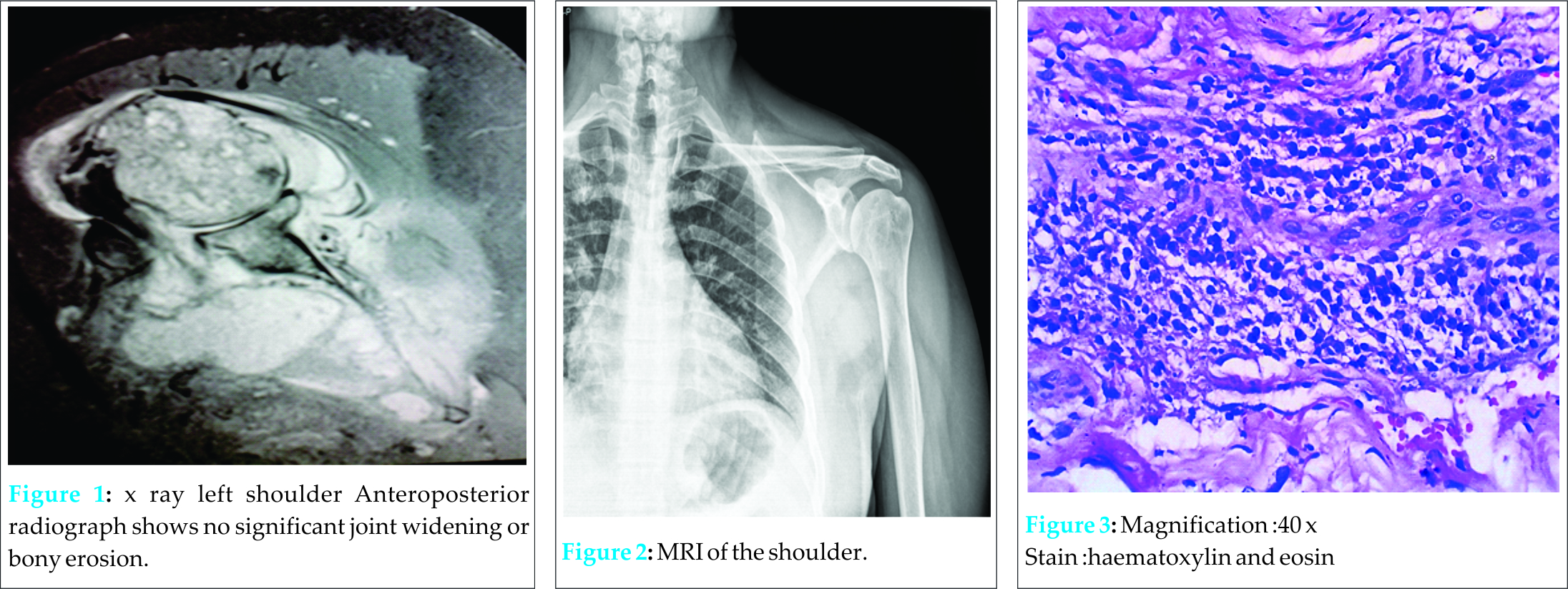
A 43-year-old man presented to the orthopaedic outpatient clinic with 2 months history of pain and limited range of motion in his left shoulder. His pain was insidious in onset, mild to moderate in intensity, aggravated by activities and associated with moderate rest and night pain. There was no history of direct or indirect trauma to the left shoulder. Patient was diagnosed as frozen shoulder at an outside facility and had been given intraarticular Depomedrol 40 mg injection for the same 40 days ago with no improvement in his symptoms. He had no fever, chills or rigors. He had no weight loss or loss of appetite. He is diabetic and has liver cirrhosis and is on treatment. On physical examination, the patient was afebrile, B.P was 110/70 mmHg, pulse rate-72beats/min. The skin colour and temperature of the left shoulder were normal, but the shoulder was tender to touch over the anterior joint line. Shoulder was very stiff and all shoulder movements were severely restricted. MRI was obtained [Fig 2] which showed extraosseous soft tissue enhancements around left shoulder with soft tissue abscess in inter muscular planes of supraspinatous, infraspinatous, subscapularis. glenoid joint effusion with distension of axillary recess.
Blood test revealed normal white cell count with normal differential count, CRP-13.4 mg/l (normal<5.0 mg/l). The erythrocyte sedimentation rate was raised, at 88 mm/hour (normal range,0-20 mm/hour ) Aspiration of shoulder joint was performed and fluid was sent for aerobic and anaerobic culture, AFB staining, Mycobacterium culture, and Mycobacterium genetic testing. Aerobic cultures identified methicillin –resistant Staphylococcus aureus. Arthroscopic lavage of the joint was done and articular fluid sent for repeat aerobic and anaerobic culture. Synovial biopsy was obtained and sent for histopathological examination. During the procedure, joint visualization was markedly limited because of severe inflammation and fibrinous changes of the joint. The articular cartilages of glenoid and humeral head were completely eroded down to the bone. Rotator cuff undersurface and anterior capsule were completely covered by fibrinous material. Joint was thoroughly debrided. Culture of joint aspirate came back positive for Klebsiella pneumoniae. Susceptibility of the isolate was determined with the disk diffusion method and it was susceptible only to colistin. Mycobacterium culture and genetic test came back as negative. Histopathological examination of the synovial tissue revealed (Fig. 3) fibrocollagenous and fibrovascular inflammed connective tissue containing proliferated blood vessels and perivascular mixed inflammatory cells and lymphoplasmacytoid cells. Based on preoperative and intraoperative culture report, a definitive diagnosis of polymicrobial septic arthritis of the shoulder was established and patient was treated with combination antimicrobial treatment.
Discussion
Septic arthritis of the shoulder is a rare complication. Most patients present acutely with severe pain, loss of function and systemic symptoms. Our Patient had muted inflammatory response probably due to immunocompromised state (cirrhosis and diabetes) which is not uncommon. Hence, classical features of infection were not there in this patient. Most often it is hematogenous seeding of shoulder joint, however it can also happen after intraarticular steroid injections. Septic arthritis of the shoulder is more common in immunocompromised patients and intravenous drug abusers [1]. In this case report, the patient had atypical clinical symptoms and is immunocompromised and his primary source of infection seems to be hematogenous. Our experience with this patient highlights the importance of maintaining high index of suspicion for septic arthritis in immunocompromised patients presenting with atypical shoulder pain associated with stiffness.
In the setting of suspected septic arthritis, diagnosis should be confirmed as soon as possible and treatment initiated without much delay. Our initial pre-investigation diagnosis was atypical shoulder pain and stiffness of non specific etiology in an immunocompromised patient and infection was part of the differential diagnosis not the only diagnosis. Esenwein et al in his report highlighted the importance of early intervention to prevent chondral damage, osteomyelitis and also to prevent systemic spread [2]. Various authors have highlighted the importance of early diagnosis and management of septic arthritis failing which could lead to osteomyelitis and septic shock [3,4]. In our patient, the diagnosis was delayed due to atypical presentation and over reliance on clinical findings at an outside center. Intraoperatively, he was noted to have severe chondral erosion. However, our patient fortunately did not have systemic spread amidst compromised immune status. We strongly recommend early imaging studies in immunocompromised patients presenting with shoulder pain and practitioners should avoid loosely diagnosing as shoulder pain with associated stiffness as frozen shoulders. Klinger et al. did a retrospective study on 21 patients who underwent surgical treatment for septic arthritis of the shoulder joint between 2000 and 2007, and he concluded that patients with symptoms for less than 2 weeks did well with arthroscopic approach and early infection can be managed arthroscopically [5]. Our patient underwent arthroscopic washout followed by parenteral antibiotics with good outcome. Our reports show that arthroscopic washout can give good result even after 2 weeks of clinical symptoms if there is no evidence of osteomyelitis. Septic arthritis of the shoulder is very often due to hematogenous spread and diagnosis is often clinical. Laboratory investigations and imaging studies like MRI and USG may be useful in establishing the diagnosis but confirmation is usually by joint aspiration [6]. Patients who are immunocompromised and have insidious onset of moderate to severe pain and which fails to respond to trial of conservative treatment should be subjected to either ultrasound or MRI instead of X-ray because very often in these group of patients it is primarily a soft tissue pathology like impingement, RC tear, calcific tendinitis or rarely infections and malignancies. We recommend that moderate pain of more than 4 weeks duration with severe stiffness in immunocompromised patient (liver cirrhosis, renal failure, steroid treatment) should be further evaluated with MRI or ultrasound in the setting of normal X-ray and should not be loosely diagnosed as Frozen Shoulder. Staphylococcus aureus was the most commonly reported organism [7, 8]. Our patient’s intraoperative specimen grew Klebsiella pneumonia. Septic arthritis in cirrhotic patients has been reported by various other authors. Goldenberg in his report emphasized the role of local as well as systemic factors that predispose patients with cirrhosis to gram-negative bacterial joint infections [9]. Malnick also reported a case of spontaneous septic arthritis in a cirhottic patient that was due to E.coli [10]. Our study as well as other studies by Goldenberg and Malnick highlight the importance of including broad spectrum antibiotics with gram negative cover whilst waiting for final culture sensitivity.
Conclusion
Septic arthritis of shoulder may not present with classic clinical features. A through clinical and radiological evaluation should be executed and treatment initiated promptly to prevent complications like septic shock and osteomyelitis. Arthroscopic washout is an acceptable treatment option in early cases without osteomyelitis.
Clinical Message
This case presented a diagnostic challenge because of its atypical presentation. The case highlights the importance of establishing anatomical and pathological diagnosis using MRI in patients with shoulder pain instead of loosely diagnosing them as impingement or frozen shoulder. The case also challenges the practice of routine shoulder Depomedrol steroid injection, in the setting of secondary frozen shoulder, atleast in immunocompromised individuals. Primary idiopathic frozen shoulder is a rare condition and secondary frozen shoulder cases are often due to underlying shoulder pathology.
References
1. Gordon EJ, Hutchful GA: Pyoarthrosis simulating ruptured rotator cuff syndrome. South Med J 1982;75(6):759-762.
2.Esenwein SA, Ambacher T, Kollig E, Kutscha-Lissberg F, Hopf F, MuhrG.Unfallchirurg 2002;105(10):932-8. German. PMID:12376899.
3. Mehta P, Schnall SB, Zalavras CG. Septic arthritis of the shoulder, elbow and wrist. ClinOrthopRelat Res 2006;451:42-5.
4.Jeon I, Choi C, Seo J, Seo K, Ko S, Park J. Arthroscopic management of septic arthritis of the shoulder joint. J Bone Joint Surg Am 2006;88:1802-6.
5. Klinger HM, Baums MH, Freche S, Nusselt T, Spahn G, SteckelH. ActaOrthop Belg. 2010;76(5):598-603.PMID:2113821.
6.Gelberman RH, Menon J, Austerlitz MS, Weisman MH. Pyogenic arthritis of the shoulder in adults. J Bone Joint Surg Am 1980;62:550-3.5.
7.Leslie BM, Harris JM 3 rd , Driscoll D. Septic arthritis of the shoulder in adults. J Bone Joint Surg Am 1989;71:1516-22.
8. Lossos IS, Yossepowitch O, Kandel L, Yardeni D, Arber N. Septic arthritis of the glenohumeral joint: A report of 11 cases and review of the literature. Medicine 1998;77:177-87.
9.Goldenberg DL, Brandt KD, Cathcart ES, Cohen AS. Acute arthritis caused by gram-negative bacilli: a clinical characterization. Medicine. 1974;53:197–208.
10.Malnick SD, Attali M, Israeli E, Gratz R, Geltner D. Spontaneous bacterial arthritis in a cirrhotic patient. J ClinGastroenterol. 1998;27:364–366.
| How to Cite This Article: Sambandam SN, Atturu M. A Case of Septic Arthritis of Shoulder Presenting as Stiffness of the Shoulder. Journal of Orthopaedic Case Reports 2016 April-June;6(2): 31-33. Available from: https://www.jocr.co.in/wp/2016/04/01/2250-0685-418-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com