[box type=”bio”] What to Learn from this Article?[/box]
Spinal anesthesia is not without any complication, it might result in complications such as neuropathic joint.
Case Report | Volume 6 | Issue 4 | JOCR September-October 2016 | Page 77-79 | S Swaroop Chandra, J K Giriraj Harshavardhan, Ganesan G Ram, P V Vijayaraghavan DOI: 10.13107/jocr.2250-0685.580
Authors: S Swaroop Chandra[1], J K Giriraj Harshavardhan[1], Ganesan G Ram[1], P V Vijayaraghavan[1]
[1]Department of Orthopaedics, Sri Ramachandra Medical University, Chennai, Tamil Nadu, India.
Address of Correspondence
Dr. S Swaroop Chandra,
Department of Orthopaedics, Sri Ramachandra Medical University, Chennai, Tamil Nadu, India.
E-mail: Swaroopchanda93@gmail.com
Abstract
Introduction: Neurological complications due to spinal anaesthesia are dyaesthesia, paraesthesia, caudaequina syndrome, neuropathic joint. However neurological complications are rare. We report a case of neuropathic joint of knee as a complication of syrinx following post spinal anaesthesia.
Case Report: A 33years old lady came with a complaints of pain and instability of her left knee and left foot drop. She had developed weakness of her left lower limb following her caeserian section surgery done under spinal anaesthesia. Clinically and radiologically she had features of neuropathic left knee joint which had occurred as a complication of syrinx following spinal anaesthesia.
Conclusion: The case is reported for its rarity and to highlight the possible neurological complications of spinal anaesthesia.
Keyword: Neuropathic Joint, Syrinx, Post Spinal Anaesthesia
Introduction:
Most common anaesthesia given in day to day practise is spinal due to its cost effectiveness, safety and efficacy, which provides both motor and sensory block with high success rate. Complications such as hypotension, headache and urinary retention are relatively common. However permanent neurological complications are very rare.
Neurological complications due to spinal anaesthesia are burning sensation over buttocks, dyaesthesia, paraesthesia, transverse myelitis, anterior spinal artery syndrome, caudaequina syndrome. We report a case of neuropathic left knee joint which developed because of formation of a syrinx following inadvertent dural penetration during spinal anaesthesia [2, 3].
Case Presentation:
A 33 years old female gravida 2 came with a complaint of weakness of left lower limb and swelling in left knee. Patient was apparently normal before and underwent lower segment caeserian section under spinal anaesthesia in November 2014. She is unaware of the level at which it was given. Immediately after introduction of spinal lumbar puncture needle she experienced severe shooting pain and tingling sensation over left lower limb. Post operatively patient was not having any bladder/bowel incontinence but she had weakness of her left lower limb which showed no recovery and was gradually progressive. Two months before presentation patient had a history of slip and fall over her left knee while walking following which she developed swelling over her left knee joint.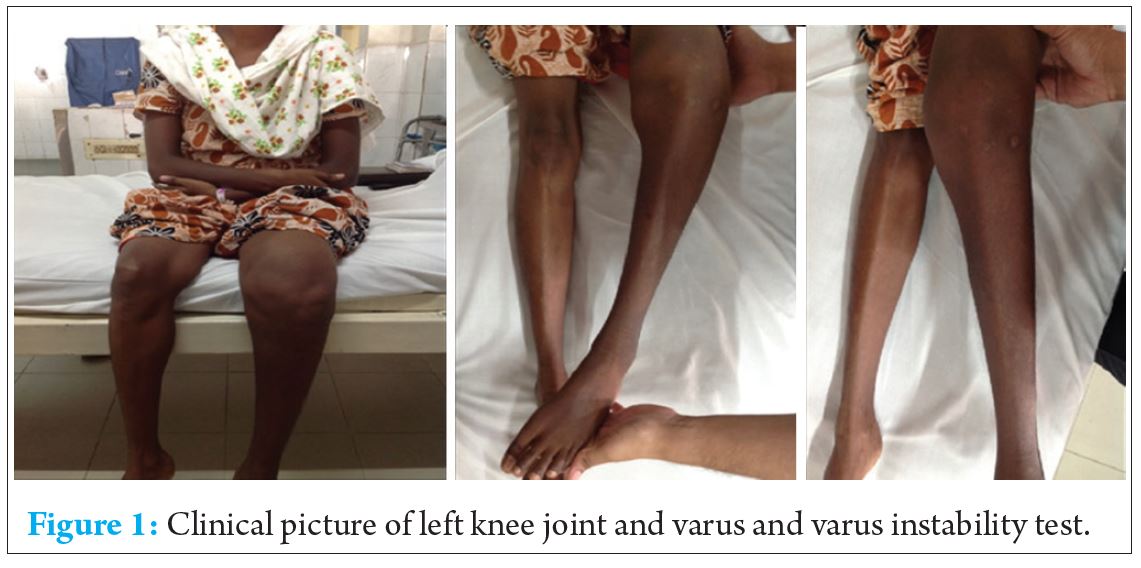
On examination, diffuse swelling was noted over left knee. Knee flexion was possible up to 90 degrees with some extensor lag. Gross abnormal mobility was present in both sagittal and coronal planes (Fig. 1). Anterior and posterior drawer tests were positive. Valgus and varus instability tests were also positive.
The power of left lower limb was reduced (refer table below)
Knee, ankle and plantar reflexes were absent.
Pain and temperature (crude sensations) was absent involving L4, L5 and S1 dermatomes. Vibration and joint position sensations were intact.
Routine blood investigations are done found to be with in normal limits except ESR (90).
X ray and computerized tomography of knee joint was done which show marked destructive changes, sclerosis, dislocation and sub chondral fractures of knee joint ( Refer Fig. 2 )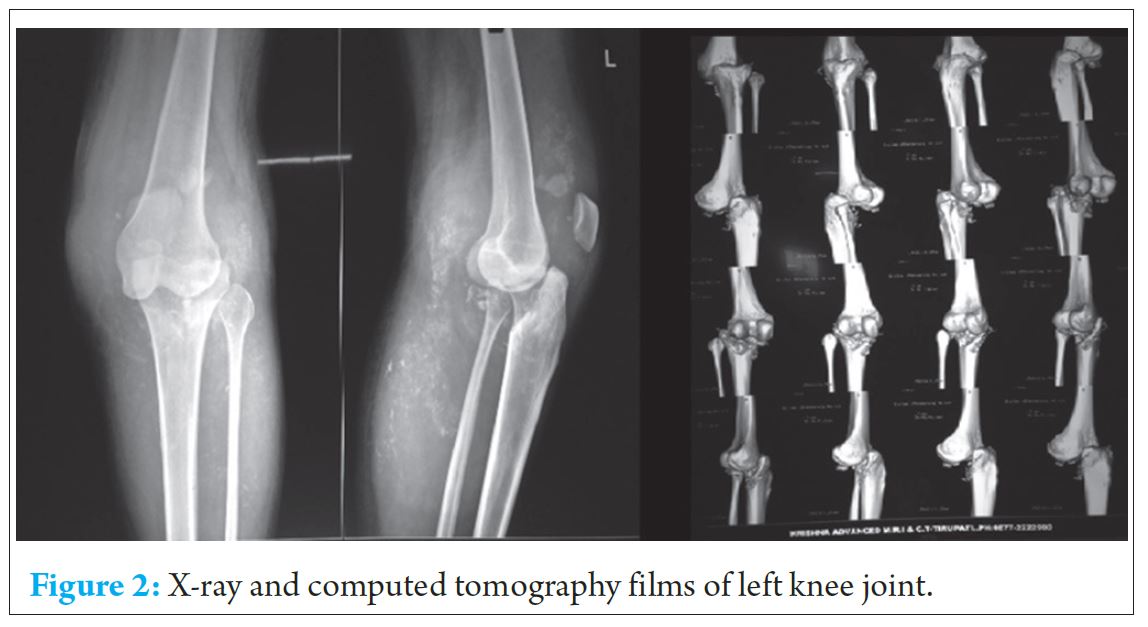
MRI of whole spine was done which show syrinx at D7, D9, D10 & D12 and L1 level. (Refer Fig.3)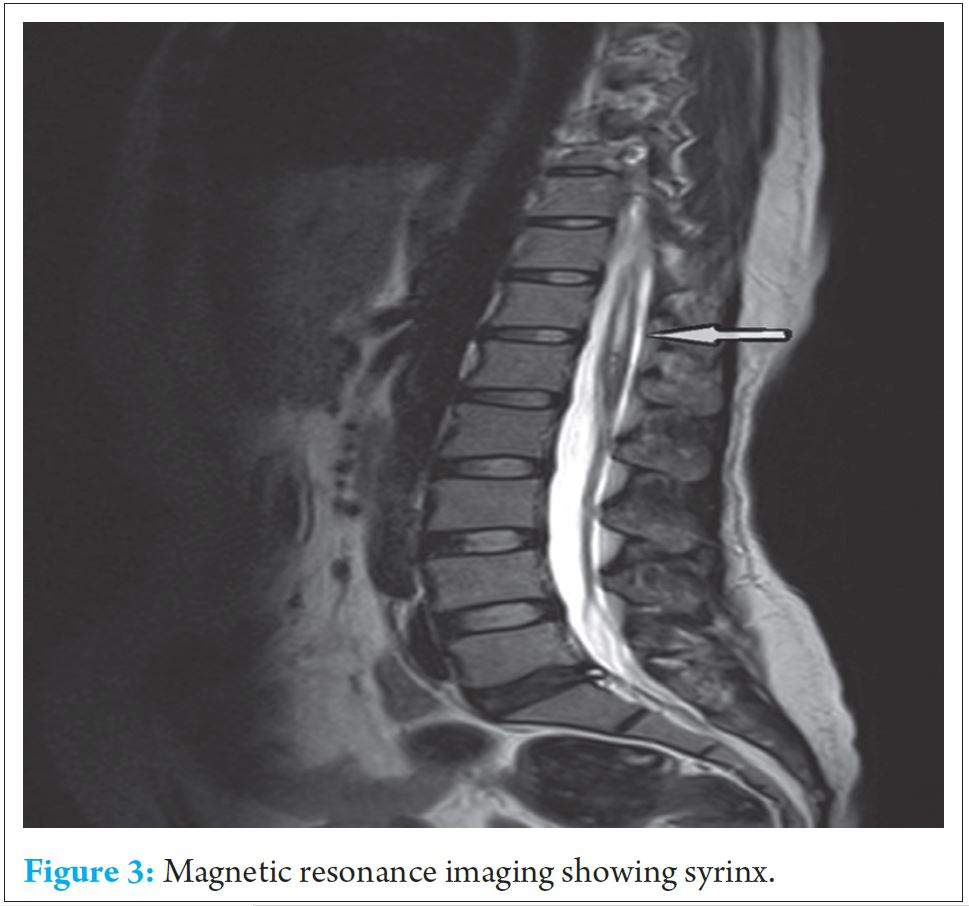
Patient was counselled regarding the possible options of treatment. Arthrodesis could be attempted but with high failure rates and loss of available knee movements. Knee replacement with a constrained/hinged custom mega prosthesis (in view of gross instability) could be done with high rates of early loosening and infection. Patient was not willing for any surgical procedure and hence she was advised and fitted with an orthoses.
Discussion:
Incidence of permanent neurological injury following spinal anaesthesia varies between 0-4.2/10000 patients. Pre-existing spinal pathology or disease increase the incidence of postoperative neurological complication following neuraxial blockade.
Reynolds reported a series of cases of conusmedullaris injury post spinal anaesthesia [1]. The possible reason for this were indicated as misplacement of needle at the lower end of spinal cord, mis- identification of Tuffier’s line (line drawn between highest points of iliac crest in adults which corresponds to L4 spinous process), arachnoid membrane attachment to the conus like a web. A traumatic needle insertion can cause severe disturbance in intra medullary micro circulation and the direct toxicity of anaesthetic agent over the injured cord resulted in syrinx.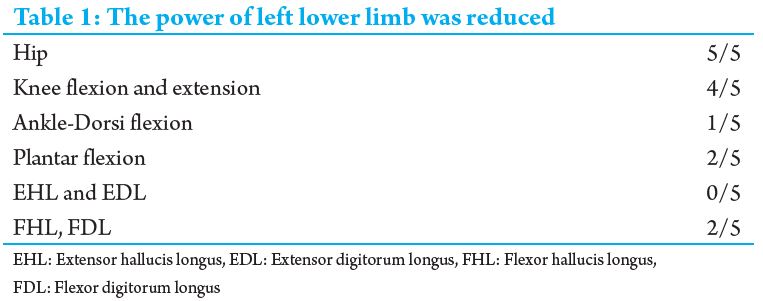
Neuropathic arthropathy develops in weight bearing joints and the most common cause is diabetes mellitus, other causes being leprosy, menigomyelocele,syringomyelia, spinal cord injury, and tabesdorsalis. The most common joints affected are the ankle and joints of the feet. Involvement of the knee joint is very uncommon and rarely reported till date [4].
Painless abnormal mobility due to destruction of afferent proprioceptive fibres, loss of sensation of joint, followed by severe degenerative changes, osteophyte formation, subchondral fractures suggests neuropathic joint.
Conclusion:
Syrinx can occur as a complication of spinal anaesthesia. Neurological deficit as a complication of syrinx can be disabling and can lead to the neuropathic joints even in larger joints as illustrated in this case report.
Clinical Message:
Patients who have severe radicular pain following spinal anaesthesia should be carefully followed up for the development of a syrinx and neurological deficit. Neuropathic knee can occur as a complication and is difficult to treat with poor outcome.
References:
1. M. J. Doherty, P. A. Millner et.al, Non-invasive ventilation in the treatment of ventilator failure following corrective spinal surgery, Anaesthesia, 2001, 56, pages 235±247.
2. AlparslanApan and ÖzgünCuvaşApan; Complications in Spinal Anaesthesia Ch.7; 139-159
3. Niraj Kumar, Surya Prakash Patidar et.al, Focal Myelomalacia and Syrinx Formation after Spinal Anaesthesia, JAPI • July 2010 • VOL. 58
4. Gopakumar TS, Rajanish R, et.al, Neuropathic Joint following Spinal anesthesia, J. Orthopaedics 2008, 5(3)e2.
5. Auroy Y,Narchi P,Messiah A, et al .Serious complications relate to regional anaesthesia Results of a prospective survey in France. Anaesthesiology 1997;87:479-486.
6. Aromaa U, Lahdensuu M, Cozantis DA. Severe complications associated with epidural and 6. Aromaa U, Lahdensuu M, Cozantis DA. Severe complications associated with epidural and spinal anaesthsias in Finland 1987- 1993. A study based on patient insurance claims. Acta Anaesthsiol Scand 1997;41:445-452
7. Rajakulendran Y, Rahman S, Venkat N. Long-term neurological complication following traumatic damage to the spinal cord with a 25 gauge Whitacre spinal needle. International Journal of Obstetric Anesthesia 1999; 8: 62±6.
8. Holloway J, Seed PT, O’Sullivan G, Reynolds F. Paraesthesiae and nerve damage following combined spinal epidural and spinal anaesthesia. International Journal of Obstetric Anesthesia 2000; 9: 151±5.
9. Waters JH, Watson TB, Ward MG. Conus medullaris injury following both tetracaine and lidocaine spinal anesthesia. Journal of Clinical Anesthesia 1996; 8: 656±8.
10. Lambert LA, Lambert DH, Strichartz GR. Irreversible conduction block in isolated nerve by high concentrations of local anesthetics. Anesthesiology 1994; 80: 1082±93.
11. Loo CC, Dahlgren G, Irestedt L. Neurological complications in obstetric regional anaesthesia. International Journal of Obstetric Anesthesia 2000; 9: 99±124.
12. Rigler ML, Drasner K, Krejchie TC, et al. Cauda equina syndrome after continuous spinal anesthesia. Anesthesia and Analgesia 1991; 72: 275±81.
13. Tedeschi E, Marano I, Savarese F, et al. Neurological deficit following spinal anaesthesia: MRI and CTevidence of spinal cord gas embolism. Neuroradiology 1999; 41: 275±8.
14. Katz N, Hurley R. Epidural anesthesia complicated by fluid collection within the spinal cord. Anesthesia and Analgesia 1993; 77: 1064±5.
15. Greaves JG. Serious spinal cord injury due to haematomyelia.
| How to Cite This Article: Chandra SS, Harshavardhan JKG, Ram GG, Vijayaraghavan PV. Neuropathic Knee Joint – A Complication of Syrinx Following Spinal Anesthesia: A Rare Case Report and Review of Literature. Journal of Orthopaedic Case Reports 2016 Sep-Oct;6(4): 77-79. Available from: https://www.jocr.co.in/wp/2016/10/10/2250-0685-580-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




