[box type=”bio”] What to Learn from this Article?[/box]
Biological hypotheses could account for an increased risk of acetabular loosening in acromegalic patient.
Case Report | Volume 7 | Issue 2 | JOCR March – April 2017 | Page 94-97| Simon Koulischer, Bilal Kapanci, Nicolas Bloemers, Tatiana Charles, Marc Jayankura. DOI: 10.13107/jocr.2250-0685.768
Authors: Simon Koulischer[1], Bilal Kapanci[2], Nicolas Bloemers[2], Tatiana Charles[2], Marc Jayankura[2]
[1] Department of Orthopaedic Surgery, ISPPC, Boulevard Zoé Drion 1, 6000 Charleroi, Belgium.
[2] Department of Orthopaedic and Traumatologic Surgery, Erasme Hospital, Route de Lennik 808, 1070 Brussels, Belgium.
Address of Correspondence
Dr. Simon Koulischer,
Service d’orthopédie de l’ISPPC, Boulevard Zoé Drion 1, 6000 Charleroi, Belgium.
E-mail: simon.koulischer@chu-charleroi.be
Abstract
Introduction: Acromegaly is a rare disorder characterized by excess secretion of growth hormone and its principle mediator, insulin-like growth factor-1. Although acromegaly is frequently associated with osteoarthritis, the outcome of arthroplasty in this population is not documented.
Case Report: We report here a case of aseptic loosening of an uncemented total hip arthroplasty acetabulum in an acromegalic patient that was revised with a cemented cup. It has been suggested that the incidence of this complication is increased in other pathology with a similarly high bone-turnover (e.g., Paget’s disease), but this complication has however not yet been reported in the setting of acromegaly.
Conclusion: Although coincidence cannot be ruled out, multiple metabolic hypotheses could account for an altered osseointegration process in the presence of acromegaly, which could lead to a higher risk of loosening.
Keywords: Acromegaly, aseptic loosening, growth hormone, total hip arthroplasty.
Introduction
It is estimated that around 2 million total hip arthroplasties (THAs) are performed worldwide annually, and projections of rising demand are reported at least for the United States [1]. However, some THAs fail during the period of service and require revision surgery, which is more expensive than the primary operation and brings less satisfactory outcomes along with increased risk for complications [2]. In this context, the Food and Drug Administration has encouraged the reporting of unusual or unreported mechanical device complications [3]. It is estimated that around 2 million total hip arthroplasties (THAs) are performed worldwide annually, and projections of rising demand are reported at least for the United States [1]. However, some THAs fail during the period of service and require revision surgery, which is more expensive than the primary operation and brings less satisfactory outcomes along with increased risk for complications [2]. In this context, the Food and Drug Administration has encouraged the reporting of unusual or unreported mechanical device complications [3]. Aseptic loosening, characterized by bone resorption at the bone-implant interface, is the most frequent cause of late failure and is reported to be accountable for up to 55% of THA revisions [4]. Acromegaly is a rare disorder characterized by excess secretion of growth hormone (GH) and its principle mediator, insulin-like growth factor-1 (IGF-1). Its annual incidence is 6 per million people. It is caused by GH-secreting pituitary tumors, or very rarely by extrapituitary disorders. Increased GH and IGF-1 levels lead to a form of diffuse osteoarthritis, which may dominate the clinical picture and require surgical advice [5]. However, there is no data on the outcome of arthroplasty in this population. We report here a case of aseptic loosening of an uncemented acetabulum after THA in an acromegalic patient and review the biological hypotheses that might account for a higher risk of aseptic loosening.
Case Report
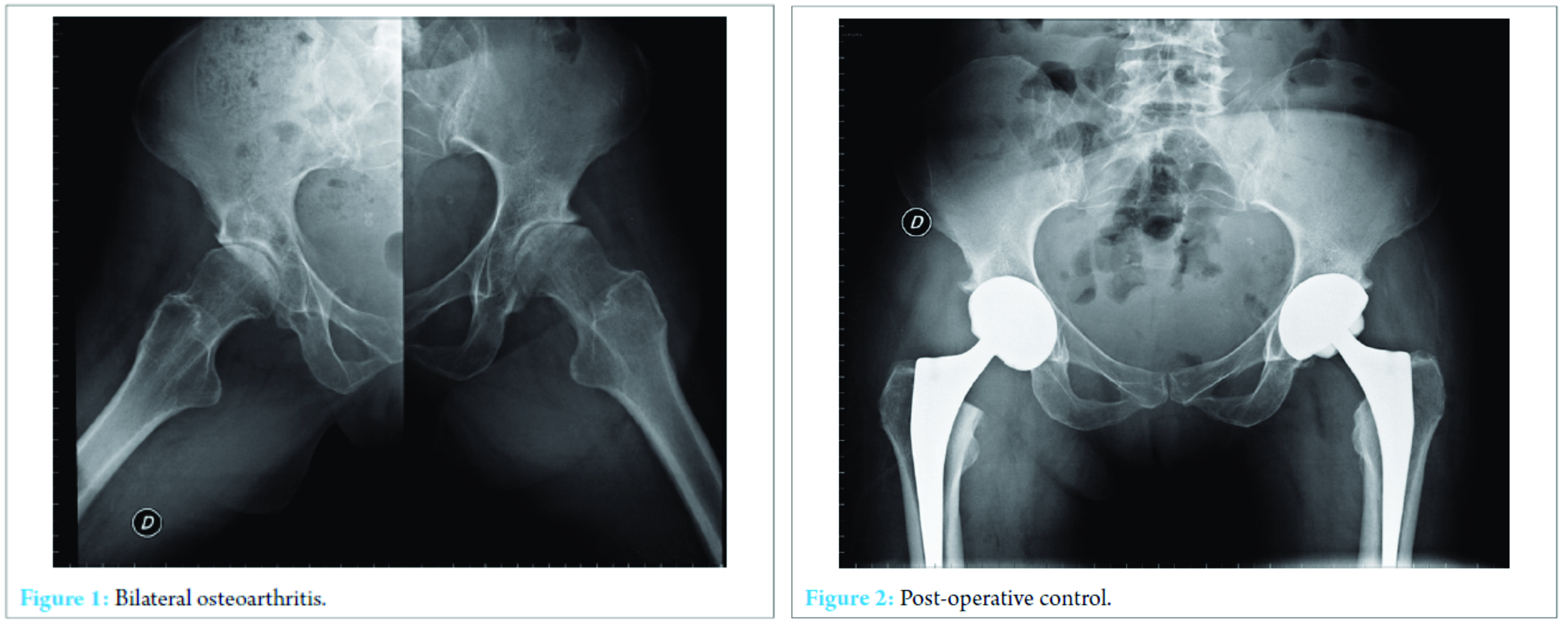
A 64-year-old Caucasian woman was referred to our hospital with a 3-year history of bilateral hip pain. 2 years prior, the patient had been diagnosed with a GH-producing pituitary adenoma and treated in 2008 by transsphenoidal surgery without radiation. Post-operative follow-up revealed a poor control of GH levels. At the time, she was treated with the administration of octreotide acetate (30 mg/month) (Sandostatin LAR, Novartis Pharma, Tokyo, Japan). On physical examination, the patient’s height and weight were 168.2 cm and 57 kg, respectively. Her blood pressure was 145/109 mmHg. Typical acromegalic features, including enlargement of the nose, lips, tongue, and extremities, were observed; however, no cushingoid features, such as central obesity, moon face, and buffalo hump, were present. Range of motion of both hips was limited in every direction. The startup test was painful, and a slight Trendelenburg gait was observed. Standard X-rays revealed a bilateral narrowing of the joint space, osteophytes, and slight sclerosis, corresponding to Kellgren and Lawrence Grade 2 hip osteoarthritis (Fig. 1). As the 6-month conservative treatment with non-steroidal anti-inflammatory acetaminophen and physiotherapy failed to improve symptoms, bilateral THA was proposed. The right hip was operated on in December 2008 and the left hip in January 2009. An uncemented, double-tapered, fully hydroxyapatite-coated stem (quadra H reg, Medacta, Castel San Pietro, Switzerland) with a modular neck and ceramic head with a 28-mm articulation was implanted through a direct anterior approach on a specialty orthopedic traction table. The acetabular component was an uncemented, porous cup with a ceramic insert (Versafit Cup CC, Medacta SA, Castel San Pietro, Switzerland).
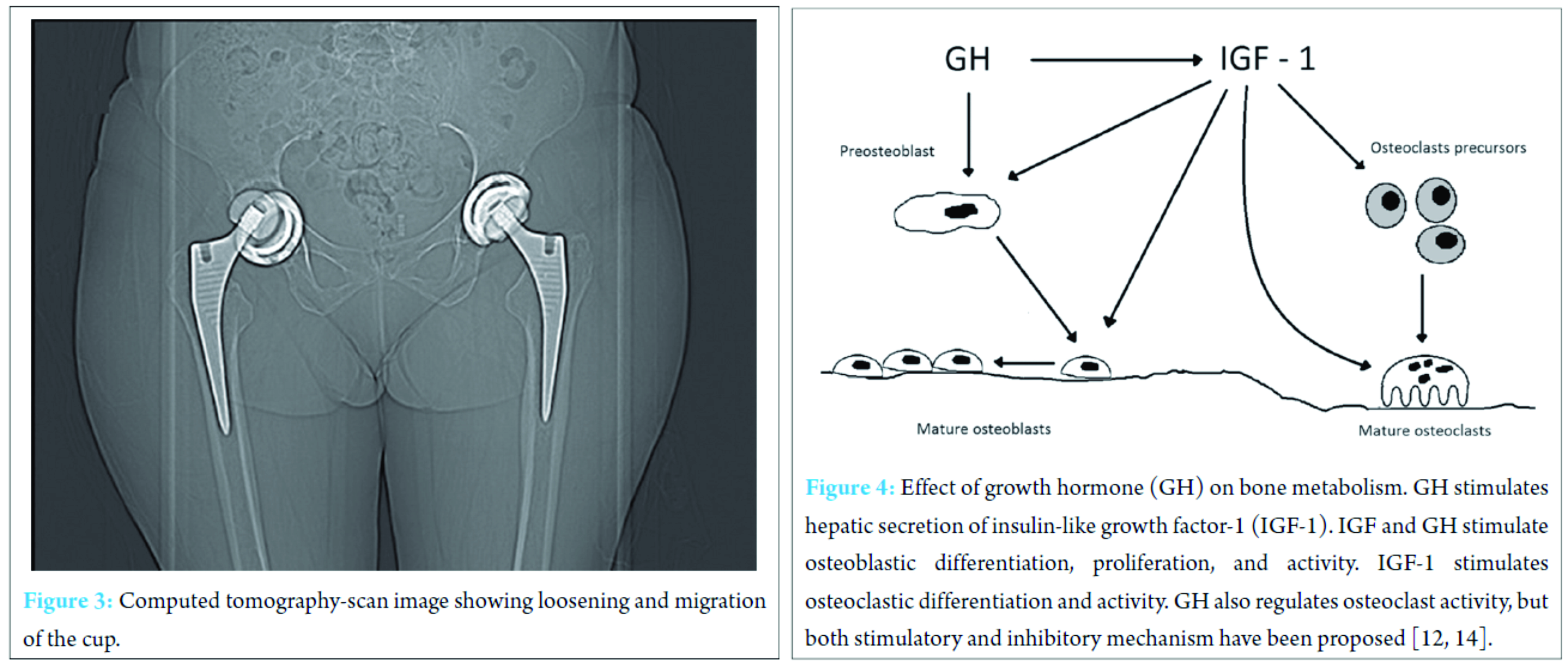
The post-operative conventional X-ray is shown in (Fig. 2). In April 2013, the patient presented with a recurrence of right-sided hip pain. Although zones of peri-implant lucency were found on standard X-ray on both stem and acetabulum, no change in the inclination of the cup was noted. A bone scintigraphy showed an unusual fixation on the acetabular component. 2 weeks later, the patient suddenly reported extreme pain and was unable to walk. A computed tomography-scan revealed the migration of the acetabular component (Fig. 3). Samples of articular liquid were sent for bacteriological examination and culture. No evidence of infection was found. A hip arthroplasty revision was performed in May 2013 through a direct anterior approach on a traction table. Since the stem did not show any signs of per-operative instability when clinically tested, only the acetabulum was replaced with a cemented component.2 years after the revision surgery, the patient is painless and has recovered a normal range of motion.
Discussion
We conducted a literature search of Medline (PubMed) using a combination of the following keywords: “THA,” “GH,” “somatostatin,” “acromegaly,” and “loosening.” Our literature search did not reveal any report of aseptic loosening in a patient with acromegaly nor in a patient treated with a somatostatin analog. More surprisingly, we could not find any data on the general outcome of THA in this particular population.Although this was the only case of aseptic loosening in our series of 600 patients, it is possible that the observed complication is independent of the excessive GH-levels. The left hip of our patient, which was also replaced, did not present any signs of loosening. The most commonly proposed theory for aseptic loosening is that the development of excess wear particles produces a proinflammatory state, which leads to increased osteoclast differentiation and macrophage production, and ultimately causes local osteolysis and aseptic loosening around the prosthesis. Other frequent causes of uncemented acetabulum loosening include insufficient press-fit fixation or a lack of primary osseointegration. In our patient, we used ceramic-on-ceramic (C-o-C) coupling. The average annual wear rate of a C-o-C prosthesis has been reported to be as low as 0.016 mm in vivo, which is 10-4000 times less than that of the metal-on-polyethylene combination [6, 7].
Further, a low rate of aseptic loosening with C-o-C bearing has been reported [8]. A lack of press fit may be a possible cause of the loosening observed in our patient, but we would expect this type of loosening to occur earlier in the post-operative course. We hypothesize that the osseointegration process of the hydroxyapatite coated cup could be altered by the metabolic consequences of either excess GH levels or the treatment with a somatostatin analog. IGF-1 and GH are essential for differentiation and repair of cartilage and bone. Excess GH leads however to a form of osteoarthritis. A mechanism has been proposed to explain this process based on in vitro studies assessing the effects of GH and IGF-1 on cartilage and connective tissue [9]. Excess GH and IGF-1 cause proliferation of articular chondrocytes and increased matrix production. GH also affects connective tissue, promoting the growth of periarticular structures which results in ligamentous laxity and joint instability. Synovial hypertrophy also occurs. These processes eventually lead to wear and fissuring of the cartilage. Abnormalities in repair mechanisms further result in overproliferation of regenerating fibrocartilage. The metabolic effects of GH on adult bone are schematically represented in (Fig. 4). The resulting effect of GH on bone metabolism is an increased bone turnover, with the stimulation of both osteoclast and osteoblast. To date, it is not precisely known how a pathologically higher bone turnover could interfere with the osseointegration process of the implants. Nonetheless, at least two other THA loosenings have been reported in patients with Paget’s disease, an affection that is also characterized by an increased bone turnover [10, 11]. Somatostatin and somatostatin analogs indirectly inhibit the osteoblast activity. This feature might have also played a role in the deficient osseointegration.Other features of acromegaly can account for the poorer THA
Results
The acetabular architecture could be altered [12]; periarticular laxity could be majored [13], which could induce higher biomechanical stress on the implants; finally, increased collagen production and incorporation into the bone matrix [14] could lead to fibrous interposition at the bone-implant interface. It is not known whether cemented implants could help lower the rate of loosening in such cases. Further studies should focus on the impact of increased bone turnover on the osseointegration process of mechanical implants. The inclusion of comorbidity in nationwide arthroplasty registers could help to better define the outcome of such rare affections.
Conclusion
The outcome of hip arthroplasty in the acromegalic population is poorly documented. We report a case of aseptic loosening of an uncemented cup in an acromegalic patient. The alteration of GH-levels can alter osseointegration process through various biological mechanisms.
Clinical Message
Given the low prevalence of acromegaly, large prospective cohorts of THA in the setting of acromegaly are to date non-existent. Clinicians should nonetheless be aware that various features of acromegalic arthropathy could theoretically account for an increased risk of complications. We further encourage clinicians to report their arthroplasty results in this population.
References
1. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89(4):780-785.
2. Vanhegan IS, Malik AK, Jayakumar P, Ul Islam S, Haddad FS. A financial analysis of revision hip arthroplasty: The economic burden in relation to the national tariff. J Bone Joint Surg Br 2012;94(5):619-623.
3. Food and Drug Administration, Center for Devices and Radiological Health. Strengthening Our National System for Medical Device Postmarket Surveillance September; 2012. Available from: http://www.fda.gov/downloads/AboutFDA/CentersOffices/ OfficeofMedicalProductsandTobacco/CDRH/CDRHReports/UCM301924.pdf. [Last accessed on 2015 Oct 14].
4. Sadoghi P, Liebensteiner M, Agreiter M, Leithner A, Böhler N, Labek G. Revision surgery after total joint arthroplasty: A complication-based analysis using worldwide arthroplasty registers. J Arthroplasty 2013;28(8):1329-1332.
5. Melmed S. Medical progress: Acromegaly. N Engl J Med 2006;355:2558-2573.
6. Jiang Y, Jia T, Wooley PH, Yang SY. Current research in the pathogenesis of aseptic implant loosening associated with particulate wear debris. Acta Orthop Belg 2013;79(1):1-9.
7. Petsatodis GE, Papadopoulos PP, Papavasiliou KA, Hatzokos IG, Agathangelidis FG, Christodoulou AG. Primary cementless total hip arthroplasty with an alumina ceramic-on-ceramic bearing: Results after a minimum of twenty years of follow-up. J Bone Joint Surg Am 2010;92(3):639-644.
8. Bouras T, Repantis T, Fennema P, Korovessis P. Low aseptic loosening and revision rate in Zweymüller-Plus total hip arthroplasty with ceramic-on-ceramic bearings. Eur J Orthop Surg Traumatol 2014;24(8):1439-1445.
9. Lieberman SA, Björkengren AG, Hoffman AR. Rheumatologic and skeletal changes in acromegaly. Endocrinol Metab Clin North Am 1992;21(3):615-631.
10. Sartoris DJ, Safai C. Case report 334: Loosening of the femoral component of a total hip prosthesis with the potential pitfall of false-negative scintigraphy in a patient with Paget disease. Skeletal
Radiol 1985;14(3):236-239.
11. Gburek Z, Rybicki A. An attempt to treat loosening of the total hip endoprosthesis in Paget disease with Aredia. Chir Narzadow Ruchu Ortop Pol 1998;63(6):601-605.
12. Ueland T. Bone metabolism in relation to alterations in systemic growth hormone. Growth Horm IGF Res 2004;14(6):404-417.
13. Johanson NA, Vigorita VJ, Goldman AB, Salvati EA. Acromegalic arthropathy of the hip. Clin Orthop Relat Res 1983;173:130-139.
14. Ohlsson C, Bengtsson BA, Isaksson OG, Andreassen TT, Slootweg MC. Growth hormone and bone 1998;19(1):55-79.
 |
| Dr. Simon Koulischer |
| How to Cite This Article: Koulischer S, Kapanci B, Bloemers N, Charles T, Jayankura M. Aseptic Loosening after Total Hip Arthroplasty in an Acromegalic Patient: A Case Report. Journal of Orthopaedic Case Reports 2017 Mar-Apr;7(2):94-97 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com