In orthopedics, 3D printing can be used to generate anatomic models to accurately and effectively tailor orthopedic implants to a given patient’s anatomy thereby minimizing surgical time and morbidity.
Dr. Catherine Mackey,
Department of Orthopaedic Surgery, Montefiore Health System, Bronx, New York, United States.
E-mail: catherinemackey221@gmail.com
Introduction: Paget’s disease is a metabolic bone disorder characterized by abnormal patterns in bone remodeling, resulting in variable degrees of chronic bone pain, deformation of the long bones and rarely, and pathologic fracture. These issues can pose difficult surgical challenges, particularly in the elderly frail population, where the benefits of orthopedic intervention must be balanced with minimizing inherent surgical risks. Such considerations often include reducing operative time and blood loss, allowing for early mobilization, stabilizing an impending fracture, and providing symptom relief.
Case Report: A 77-year-old female with a 10-year history of Paget’s disease presented to an outside orthopedic clinic with progressive right leg pain and worsening anterior bowing following minor trauma to the extremity. Ultimately, the patient was offered in situ prophylactic intramedullary (IM) nail fixation, intended to augment her bone’s native strength and prevent further microfractures and subsequent deformation. A three-dimensional (3D) printed patient specific model was developed to permit for pre-contouring of an off-the-shelf implant and subsequent sterilization and use at a future point in time. She underwent uneventful IM nailing of her tibia with the pre-contoured implant and proceeded to progress clinically postoperatively.
Conclusion: In this report, we present an innovative use of a 3D printed patient-specific tibia model to pre-contour an IM nail. This surgical approach was undertaken to treat an elderly patient with a symptomatic and progressive deformity of the tibia secondary to Paget’s disease of bone.
Keywords: Paget’s disease, 3D-printing, orthopedic implant.
Three-dimensional (3D) printing, also known as additive manufacturing or rapid prototyping, was first developed in the 1980’s and has been used throughout a variety of industries including medical and dental, aerospace, automotive, and even consumer goods [1, 2]. Within the medical field, one such application includes using 3D printing to assist with pre-operative planning where patient-specific models are often used as a visual aid for the surgical team. This has allowed for better understanding of anatomic and spatial considerations, which is particularly relevant in the setting of complex oncologic resections, where normal anatomy may be distorted and where surgical margin fidelity can prove essential [3, 4]. With the development of new printing technologies and materials, 3D printed models can now be used for pre-operative surgical simulations and directly in the OR as intra-operative guides [5-8]. In patients undergoing oncologic resections, 3D printed cutting jigs and drilling guides, can help ensure both adequate margins and preoperatively planned margins, which often correspond to custom-made implants [9]. 3D printing patient-specific anatomic models can improve surgical procedures in a variety of ways by allowing for increased accuracy, better reproducibility, and decreased surgical times [6, 10].
In this report, we describe a minimally invasive and patient-specific approach for a patient with Paget’s disease of the bone. Paget’s disease of bone is a metabolic bone disorder characterized by abnormal patterns in bone remodeling, whereby there exists an uncoupling of bone resorption and bone formation [11]. One of the known complications of Paget’s includes serial microfractures which cyclically heal and re-fracture, leading to progressive limb malalignment and deformity. Historically, these deformities have necessitated major surgical interventions, including osteotomies, and internal fixation. Parvizi et al. noted that careful selection of patients for corrective osteotomy is necessary given that the deformity is often very complex and multiplanar in nature [12]. Herein, 3D printing technology was leveraged to realize surgical goals while minimizing the risks inherent in more substantial surgical procedures.
A 77-year-old female with a 10-year history of Paget’s disease presented to an outside orthopedic clinic with progressive right leg pain and worsening anterior bowing following minor trauma to the extremity. Initial management was conservative, which including casting followed by functional bracing. Despite intervention, the patient reported increasing difficulty with ambulation and completing her activities of daily living, as well as noticing a worsening leg length discrepancy. She presented to our institution for further management options.
On exam, the patient had significant anterolateral bowing of the right leg relative to the left with tenderness about the anterior aspect of the middle third of the tibia. There were no overlying signs of trauma such as abrasion or ecchymosis, and the patient was neurologically intact throughout the extremity.
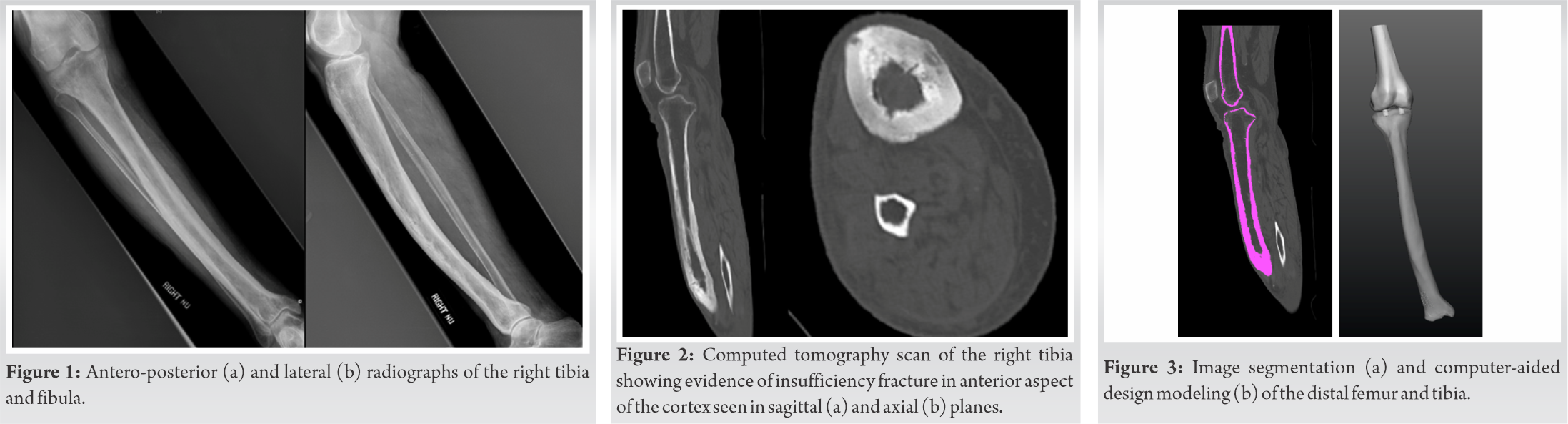
Plain radiographs demonstrated diffuse cortical thickening of the tibia with mild anterior bowing in the middle to distal third of the bone. Along with mild osteopenia, findings consistent with Pagetoid bone (Fig. 1). Computed tomography (CT) scan images demonstrated multiple transverse linear lucencies at the apex of the tibial convexity, consistent with insufficiency fractures of the Pagetoid bone (Fig. 2).
The medical and surgical options were carefully considered and given her failed conservative course thus far, recommendations were made to pursue surgical intervention. We considered conventional options including an osteotomy, followed by internal fixation, but the inherent risks of these approaches were excessive for this patient and her family, given her age, comorbidities, and limited tolerance for prolonged rehabilitation. Ultimately, the patient was offered in situ prophylactic intramedullary (IM) nail fixation, intended to augment her bone’s native strength and prevent further microfractures and subsequent deformation. Given her existing deformity, we recognized that an off-the-shelf IM nail would not navigate her IM canal. We considered designing and manufacturing a custom implant as well as intra-operative bending or contouring of an IM nail, both of which were sub-optimal. We also entertained an alternative approach, which consisted of using a 3D printed patient specific model to permit for pre-contouring of an off-the-shelf implant and subsequent sterilization and use at a future point in time.
Our institution supports a team of innovative physicians and researchers who use volumetric radiographic imaging to create and manufacture 3D printed models for use by the clinical and surgical staff. After an initial consultation, the 3D printing team used imaging data from the patient’s CT scan to create an accurate to-scale model of the patient’s affected tibia and distal femur. The imaging data were exported to a dedicated segmentation software package (Mimics 21.0, Materialize, Leuven, Belgium), where the desired anatomic components including the tibia and distal femur were separated from adjacent anatomy. The final segmented data of each of the anatomic components underwent further processing using a computer-aided design (CAD) software platform (3-matic, Materialize, Leuven, Belgium) and included adding structures to attach the two bones in the correct anatomical orientation and embedding unique labels for proper identification. Image segmentation and CAD modeling took approximately 2 h each and are shown in Fig. 3.
The tibia and femur parts were saved in stereolithography file format and were imported into slicing software (Cura, Ultimaker, Utrecht, Netherlands) in preparation for printing. 3D printing was performed with polylactic acid (PLA) using material extrusion (Ultimaker S5, Ultimaker, Utrecht, Netherlands). A total of 236 grams of PLA were used to create the model, along with an additional 33 g of PLA for material support. After printing, the model was post-processed to remove the support material and cleaned. In total, the print time was 36 h and 24 min, with post-processing time taking roughly 1 h. The finished product was a life-size physical anatomic model of the right tibia and distal femur, which uniquely depicted the patient’s anatomy and offered additional visualization (Fig. 4).
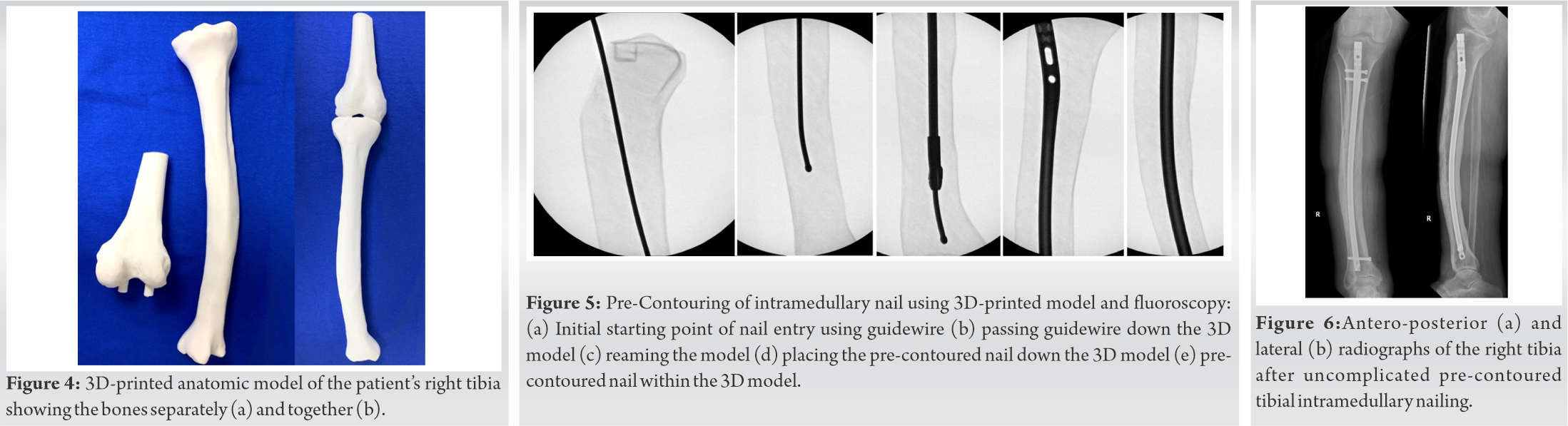
One week before the scheduled procedure, the nail was pre-contoured using routine surgical equipment within the operating room using the 3D model. This aspect of the procedure was non-sterile and a fluoroscopy unit was available. The standard steps for a tibial IM nail were performed on the 3D printed bone. The starting point was determined, an opening awl was used on the model, and a ball-tipped guidewire was placed down the shaft. The shaft was then reamed with flexible reamers. The nail was contoured using a table press in controlled and incremental steps based on gross comparison of the tibia and the implant in both the coronal and sagittal planes. Thereafter, it was sequentially introduced into the canal, advanced, removed, and further adjusted as needed. In this way, using macroscopic and fluoroscopic feedback, additional contour modifications were performed. The nail was subsequently passed down the shaft of the 3D model without issue (Fig. 5).
This nail was then sterilized and packaged. One week later, the patient was brought to the operating room where she underwent uneventful IM nailing of her tibia. The nail easily passed down the tibial shaft and the size, shape, and length all matched our pre-operative plan. The nail was locked proximally and distally. Fluoroscopy was again utilized to ensure adequate positioning (Fig. 6). The procedure was roughly 1 h and 45 min. The estimated blood loss was minimal. The patient’s perioperative pain was well controlled. She progressed well with physical therapy and was discharged on post-operative day 1.
The patient was seen in clinic for follow-up 10 days after surgery. At that time, her surgical incisions were healing and her pain was improving. She was able to straight-leg raise as well as to flex and extend her knee. She was then seen 20 days after surgery at which time her incisions had fully healed and she was ambulating very well with no pain reported. At her last follow-up nearly, she was noted to be nearly pain-free with the ability to weight-bear without symptoms.
In this case, 3D printing the patient-specific anatomy facilitated pre-operative planning. By pre-contouring the IM implant pre-operatively, we were able to cut down on operative time considerably. With the nail pre-contoured, we also believe we were reducing the rate of adverse intraoperative events such as iatrogenic fracture. Finally, being able to use a nail specific to the patient’s anatomy, enabled us to avoid an open procedure, which reduced blood loss and allowed for immediate weight-bearing and a less painful recovery.
Paget’s disease is associated with an uncoupling of the normal osteolytic and osteoblastic balance within the skeletal system, such that there is increased bone resorption, followed by abnormal bone deposition and uncoordinated bone remodeling [11]. In addition to the musculoskeletal complications associated with this pathology, the disorder is associated with deafness and cranial nerve deficits, high output cardiac failure, and an elevated risk of osteosarcoma [12]. The etiology of the disorder remains debatable and has been postulated to have both genetic and viral causes. Although the incidence of Paget’s disease has been declining in recent years, the management of insufficiency fractures and deformity in elderly adults remains a persistent relevant challenge [12]. Medical management of Paget’s disease includes bisphosphonates, which decrease bone resorption by inhibiting osteoclasts. Calcitonin has also been cited as a possible treatment, but this medication is not as potent as bisphosphonates [11]. Although these medications reduce net bone resorption, they do not address mechanical concerns or/and deformities.
Surgical management of elderly patients with multiple comorbidities should minimize operative time, bleeding, risk of infection, post-operative pain, rehabilitation requirement, and time under anesthesia [12]. Although conventional osteotomy and internal fixation would address the deformity and restore a more normal mechanical alignment to the limb, from our experience, it carries with it the risk of excessive bleeding, non-union, hardware failure, wound issues, and a long course of rehabilitation. Compared to traditional open approaches IM nailing in situ can achieve all of the aforementioned aims while minimizing many of the risks. In addition, IM nailing in situ afford the opportunity to contour the implant preoperatively to match the anatomic constraints of a given bone, which can further reduce operative time, minimize intraoperative error, and decrease iatrogenic injury. In our experience, IM nailing minimizes blood loss and soft-tissue stripping, is associated with reduced post-operative pain, requires less narcotic pain medication and allows immediate weight bearing following surgery, helping patients regain mobility, and independence.
3D printed anatomic models have increasingly gained popularity within all realms of medicine. Specifically, in orthopedic surgery, 3D printed models have been deemed useful for many types of surgical procedures including total knee arthroplasty, hip replacement, shoulder replacement, and scoliosis surgeries. At our institution, the 3D printing team assists numerous medical and surgical specialists including orthopedic surgeons, radiation oncologists, cardiologists, urologists, plastic surgeons, and neurosurgeons. In addition to direct clinical and surgical applications, our team has also used 3D printed models as a means of patient education. Our experience has found an increased patient understanding of the surgical procedure at hand, when 3D models have been used are pre-operative appointments [13].
To date, many hospital-based 3D printing departments have relied solely on institutional and research funding to carry out their cutting-edge work. However, recent changes in insurance legislation has enabled 3D printing to be coded using Category III Current Procedural Terminology (CPT) codes, temporary tracking codes to detail the usage of 3D printed models, which were released by the American Medical Association on July 1, 2019, so that some insurance companies are now starting to provide compensation for these project [14]. In conjunction with the release of these codes, a 3D printing registry has been established by the Radiological Society of North America and the American College of Radiology to enable institutional quality improvement and to provide evidence for potential future reimbursement [15]. Information about the scope of clinical indications will help to determine appropriate indications and help to guide fully reimbursable Category I CPT codes in the future.
In this report, we present an innovative application of 3D printing technology to enable pre-operative planning and implant preparation in the case of an elderly patient unable to tolerate a more extensive surgery.
By creating an anatomic, 3D-printed replica of the patient’s affected bone, we were able to accurately and effectively tailor the IM nail preoperatively to match the patient’s irregular anatomy, thereby reducing surgical time and minimizing surgical morbidity.
References
- 1.Crump SS. Apparatus and Method for Creating Three-Dimensional Objects. United States Patent US No. 5121329A; 1989. Available from: https://www.patents.google.com/patent/us5121329. (Accessed November 2020) [Google Scholar]
- 2.Hull C. Apparatus for Production of Three-Dimensional Objects by Stereolithography. United States Patent US No. 4, 575, 330A; 1986. Available from: https://www.patents.google.com/patent/us4575330a/en. (Accessed November 2020) [Google Scholar]
- 3.Wake N, Chandarana H, Huang WC, Taneja SS, Rosenkrantz AB. Application of anatomically accurate, patient-specific 3D printed models from MRI data in urological oncology. Clin Radiol 2016;71:610-4. [Google Scholar]
- 4.Wake N, Rude T, Kang SK, Stifelman MD, Borin JF, Sodickson DK, et al. 3D printed renal cancer models derived from MRI data: Application in pre-surgical planning. Abdom Radiol (NY) 2017;42:1501-9. [Google Scholar]
- 5.Levine JP, Bae JS, Soares M, Brecht LE, Saadeh PB, Ceradini DJ, et al. Jaw in a day: Total maxillofacial reconstruction using digital technology. Plast Reconstr Surg 2013;131:1386-91. [Google Scholar]
- 6.Punyaratabandhu T, Liacouras PC, Pairojboriboon S. Using 3D models in orthopedic oncology: Presenting personalized advantages in surgical planning and intraoperative outcomes. 3D Print Med 2018;4:12. [Google Scholar]
- 7.Yoo SJ, Spray T, Austin EH 3rd, Yun TJ, van Arsdell GS. Hands-on surgical training of congenital heart surgery using 3-dimensional print models. J Thorac Cardiovasc Surg 2017;153:1530-40. [Google Scholar]
- 8.Hussein N, Lim A, Honjo O, Haller C, Coles JG, van Arsdell G, et al. Development and validation of a procedure-specific assessment tool for hands-on surgical training in congenital heart surgery. J Thorac Cardiovasc Surg 2020;160:229-40.e1. [Google Scholar]
- 9.Amir Sternheim YG, Kolander Y, Dadia S. 3D Printing in Orthopedic Oncology. Amsterdam: Elsevier; 2019. [Google Scholar]
- 10.Ballard DH, Mills P, Duszak R Jr., Weisman JA, Rybicki FJ, Woodard PK. Medical 3D printing cost-savings in orthopedic and maxillofacial surgery: Cost analysis of operating room time saved with 3D printed anatomic models and surgical guides. Acad Radiol 2020;27:1103-13. [Google Scholar]
- 11.Ralston SH, Langston AL, Reid IR. Pathogenesis and management of Paget’s disease of bone. Lancet 2008;372:155-63. [Google Scholar]
- 12.Parvizi J, Klein GR, Sim FH. Surgical management of Paget’s disease of bone. J Bone Miner Res 2006;21 Suppl 2:P75-82. [Google Scholar]
- 13.Wake N, Rosenkrantz AB, Huang R, Park KU, Wysock JS, Taneja SS, et al. Patient-specific 3D printed and augmented reality kidney and prostate cancer models: Impact on patient education. 3D Print Med 2019;5:4. [Google Scholar]
- 14.CMS. Medical Learning Network, July 2019 Update of the Hospital Outpatient Prospective Payment System (OPPS); 2020. Available from: https://www.cms.gov/files/document/mm11605.pdf. [Last accessed on 2020 Jun 01]. 15. ACR. 3D Printing (3DP) Registry; 2020. Available from: https://www.acr.org/practice-management-quality-informatics/registries/3d-printing-registry. [Last accessed on 2020 Oct 17]. [Google Scholar]