Intradiscal ozone therapy for PIVD has its own set of complications, further studies are warranted to validate its safety profile.
Dr. Sarvdeep Singh Dhatt,
Department of Orthopaedics, Post Graduate Institute of Medical Education and Research, Chandigarh – 160 012, India.
E-mail: sdhatt@yahoo.com
Introduction: Ozone therapy is one of the evolving, yet far from conclusive, alternative minimally invasive treatment option in the management of herniated disc in the cervical and lumbar spine. It causes the decrease in the volume of herniated disc by dehydration.
Case Report: We hereby present the first reported case of Mycobacterium infection of the spine secondary to ozone therapy with the aim to caution the surgeons regarding the complications of intradiscal ozone therapy.
Conclusion: Lack of proper, adequate, and recommended precautions if not taken can inoculate the varied microorganisms into the intradiscal space leading to devastating and unforeseen complications.
Keywords: tuberculosis, ozone therapy, infection.
Ozone therapy is one of the evolving, yet far from conclusive, alternative minimally invasive treatment option in the management of herniated disc in the cervical and lumbar spine. It causes the decrease in the volume of herniated disc by dehydration. Although this therapy has been used for herniated discs, the safety profile regarding its use is still controversial. We hereby present the first reported case of Mycobacterium infection of the spine secondary to ozone therapy with the aim and intent to caution the surgeons regarding the complications of intra discal ozone therapy [1, 2].
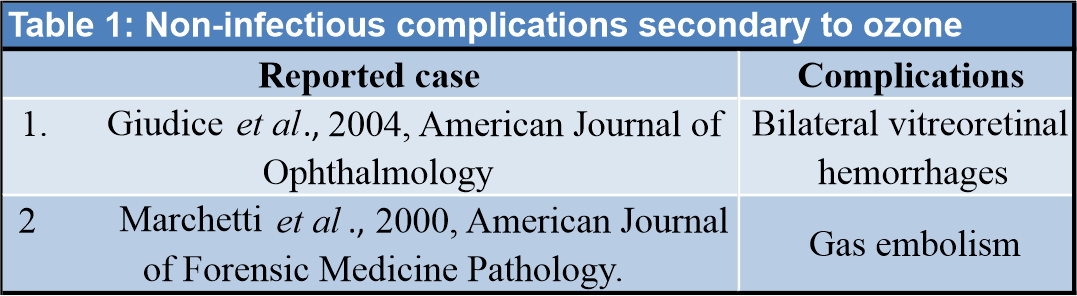
A 55-year-old female farmer by occupation presented to us with excruciating back pain radiating to her bilateral lower limbs along with the constitutional symptoms of anorexia, low-grade fever, and weight loss. The patient was investigated and found to have an elevated erythrocyte sedimentation rate, C-reactive protein, and leukocytosis. Magnetic resonance imaging (MRI) scan showed pre-paravertebral and anterior epidural collections extending from the L2/L3 to L4/L5 intervertebral disc causing spinal canal and bilateral foramina narrowing. Paravertebral collections extended up to the bilateral psoas muscles more so on the right side (Fig. 1). Fine-needle aspiration cytology stain was positive for acid-fast bacilli. Hence, the diagnosis of tuberculosis was made and anti-tuberculosis treatment (ATT) was started. A medical history revealed that the patient was managed at other hospital. She complained of pain in her lower back radiating to her left leg from the past 3 years. She was diagnosed with prolapsed intervertebral disc diseases at the level of L3/L4 and L4/L5 with the left radiculopathy (Fig. 2).
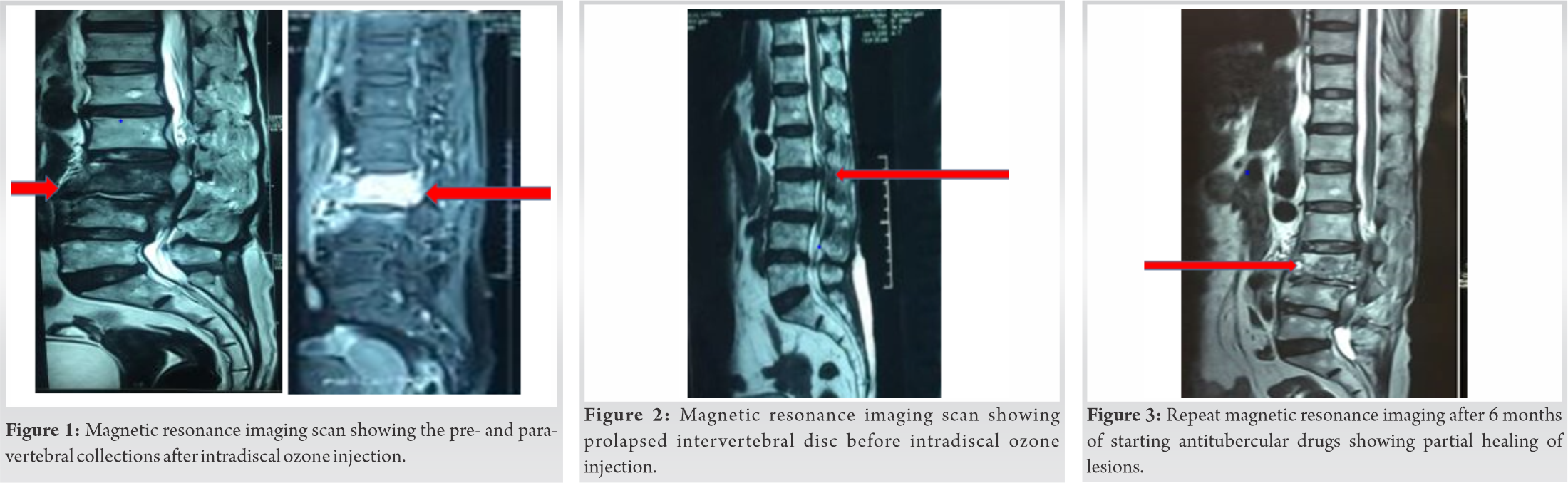
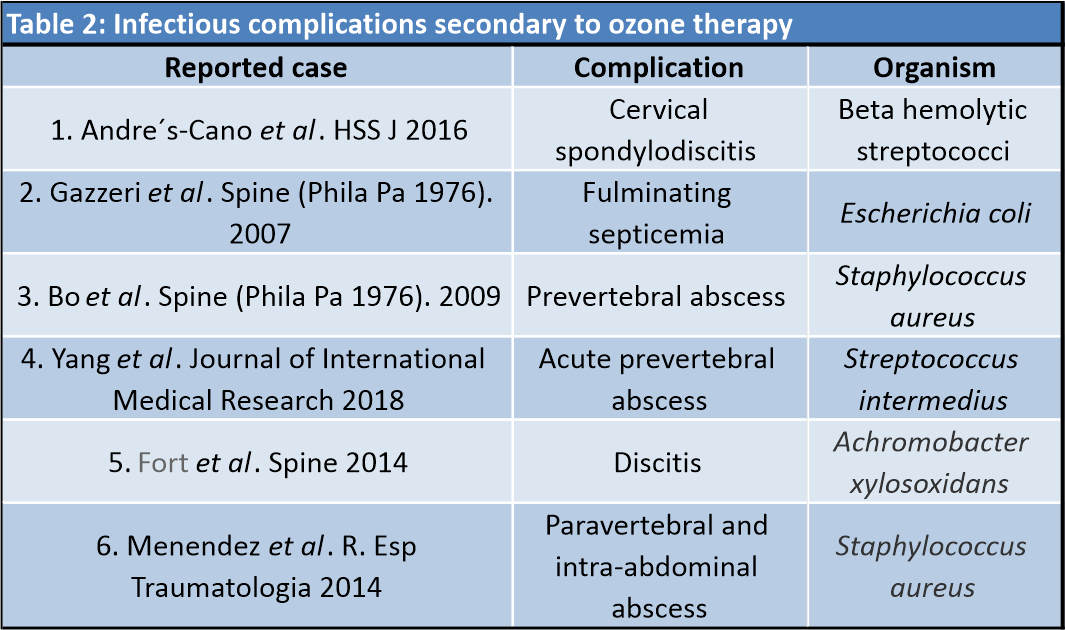
Initially, she was managed with nonsteroidal anti-inflammatory drugs and on other conservative modalities for 3 years. However, the patient did not respond satisfactorily to all these therapies. Hence, the patient underwent percutaneous instillation of 30% ozone (20 ml) along with 40 mg of Depo-Medrol a long-acting steroid into the L3/L4 and L4/L5 disc spaces. Immediate post-operative period was uneventful and the patient was discharged from the hospital on the same day. The patient was partially relieved of the symptoms but 10 days later after the operation, she complained of pain at the lower back along with left-sided radiculopathy. The patient was again put on medical therapy. As the symptoms did not resolve on the conservative treatment for 3 months and were progressive, the patient decided to take opinion at our tertiary center. The patient was put on ATT following a clinical-radiological examination and is responding well with marked improvement clinically. Repeat MRI after 6 months of starting ATT revealed partially healed lesion with decrease in active infection and reduction in the bilateral psoas abscess (Fig. 3). The patient is under close follow-up to monitor the response of antitubercular drugs both clinically and radiologically. The patient was put on ATT following a clinical-radiological examination and is responding well with marked improvement clinically. Repeat MRI after 6 months of starting ATT revealed partially healed lesion with decrease in active infection and reduction in the bilateral psoas abscess (Fig. 3). The patient is under close follow-up to monitor the response of antitubercular drugs both clinically and radiologically.
Ozone therapy has emerged an alternative treatment option in the management of herniated disc since the past three decades. [3, 4]. Due to lack of sufficient high-quality studies, its efficacy is still under scanner. Dehydration by oxidation of proteoglycans leading to decreased disc volume is the main proposed mechanism [4, 5]. As a result, the venous stasis is reduced and local microcirculation improves. The pain decreases due to decreased pressure on the nerve roots and the hypoxic damage is also ameliorated. It also has analgesic and anti-inflammatory effects. At present, there are only a few studies advocating the use and effectiveness of ozone therapy in herniated disc [1, 3, 4, 5, 6, 7]. There are a scarce case reports depicting the secondary complications after its use even on extensive literature search [2, 8, 9, 10, 11, 12, 13]. The various non-infectious complications (Table 1) reported are the bilateral vitreoretinal hemorrhages after the use of oxygen ozone therapy for lumbar disc herniations [10].
There is also one reported death due to gas embolism by ozone therapy given by auto-hemotransfusion [9]. Till date, there are only six individual reports of infectious (Table 2) complications published in literature [2, 8, 11, 12, 13, 14]. Gazzeri et al. reported a case of iliopsoas abscess secondary to Escherichia coli infection. Similarly, infection by Staphylococcus aureus leading to paravertebral abscess was reported by Bo et al. and Menendez et al. Recently, Yang et al. reported a case of acute prevertebral abscess extending from C2-T1 after intradiscal oxygen ozone chemonucleosis of cervical disc herniation. Streptococcus intermedius was the culprit organism in their case report. Another recent case report published by Fort et al. who revealed Achromobacter xylosoxidans vertebral infection secondary to ozone therapy of lumbar disc herniation.
To the best of our knowledge, this is the first ever reported case of Mycobacterium tuberculosis and the sixth report of spinal infections after intradiscal ozone therapy after exhaustive literature search. The most likely mechanism of infection in our case was the direct inoculation of the mycobacteria. Even when aseptic techniques are used the instruments and needles can become contaminated by diverse environmental pathogens. The contamination of the gas mixture is also plausible. From all these, we can conclude that intradiscal ozone therapy can be complicated by a wide and varied array of microbial infections. Aseptic technique is of paramount importance in such minimally invasive procedures. Patients should be warned about the potential complications and should be under close and regular follow ups. Hence, it is the need of the hour to investigate the benefits and critically analyze the complications of ozone therapy in herniated discs. Further studies are required to validate and recommend this as a viable alternative, relatively risk-free minimally invasive modality as one of the feasible treatment options in the present armamentarium of various non-invasive or either minimally invasive treatment options.
Concerns overlay and shadow the safety of ozone therapy in the treatment of Prolapsed intervertebral disc disease. Lack of proper, adequate, and recommended precautions if not taken can inoculate the varied microorganisms into the intradiscal space. Further studies are warranted to ensure the safety guidelines and treatment algorithm of this seemingly lucrative off the counter treatment modality.
We hereby present the first reported case of Mycobacterium infection of the spine secondary to ozone therapy with the aim and intent to caution the surgeons regarding the complications of intradiscal ozone therapy.
References
- 1.Muto M, Ambrosanio G, Guarnieri G, Capobianco E, Piccolo G, Annunziata G, et al. Low back pain and sciatica: Treatment with intradiscal-intraforaminal O(2)-O (3) injection. Our experience. Radiol Med 2008;113:695-706. [Google Scholar]
- 2.Andrés-Cano P, Vela T, Cano C, García G, Vera JC, Andrés-García JA. Cervical spondylodiscitis after oxygen-ozone therapy for treatment of a cervical disc herniation: A case report and review of the literature. HSS J 2016;12:278-83. [Google Scholar]
- 3.Paoloni M, Di Sante L, Cacchio A, Apuzzo D, Marotta S, Razzano M, et al. Intramuscular oxygen-ozone therapy in the treatment of acute back pain with lumbar disc herniation: A multicenter, randomized, double-blind, clinical trial of active and simulated lumbar paravertebral injection. Spine (Phila Pa 1976) 2009;34:1337-44. [Google Scholar]
- 4.Magalhaes FN, Dotta L, Sasse A, Teixera MJ, Fonoff ET. Ozone therapy as a treatment for lower back pain secondary to a herniated disc: A systematic review and meta-analysis of randomized controlled trials. Pain Physician 2012;15:115-29. [Google Scholar]
- 5.Andreula CF, Simonetti L, de Santis F, Agati R, Ricci R, Leonardi M. Minimally invasive oxygen-ozone therapy for lumbar disk herniation. Am J Neuroradiol 2003;24:996-1000. [Google Scholar]
- 6.Steppan J, Meaders T, Muto M, Murphy KJ. A metaanalysis of the effectiveness and safety of ozone treatments for herniated lumbar discs. J Vasc Interv Radiol 2010;21:534-48. [Google Scholar]
- 7.Staal JB, de Bie R, de Vet HC, Hildebrandt J, Nelemans P. Injection therapy for subacute and chronic low back pain: An updated Cochrane review. Spine (Phila Pa 1976) 2009;34:49-59. [Google Scholar]
- 8.Gazzeri R, Galarza M, Neroni M, Esposito S, Alfieri A. Fulminating septicemia secondary to oxygen-ozone therapy for lumbar disc herniation: Case report. Spine (Phila Pa 1976) 2007;32:121-3. [Google Scholar]
- 9.Marchetti D, La Monaca G. An unexpected death during oxygen-ozone therapy. Am J Forensic Med Pathol 2000;21:144-7. [Google Scholar]
- 10.Lo Giudice G, Valdi F, Gismondi M, Prosdocimo G, de Belvis V. Acute bilateral vitreo-retinal hemorrhages following oxygen-ozone therapy for lumbar disk herniation. Am J Ophthalmol 2004;138:175-7. [Google Scholar]
- 11.Bo W, Longyi C, Jian T, Guangfu H, Hailong F, Weidong L, et al. A pyogenic discitis at c3-c4 with associated ventral epidural abscess involving c1-c4 after intradiscal oxygen-ozone chemonucleolysis: A case report. Spine (Phila Pa 1976) 2009;34:298-304. [Google Scholar]
- 12.Yang CS, Zhang LJ, Sun ZH, Yang L, Shi FD. Acute prevertebral abscess secondary to intradiscal oxygen-ozone chemonucleolysis for treatment of a cervical disc herniation. J Int Med Res 2018;46:2461-5. [Google Scholar]
- 13.Fort NM, Aichmair A, Miller AO, Girardi FP. L5-S1 Achromobacter xylosoxidans infection secondary to oxygen-ozone therapy for the treatment of lumbosacral disc herniation: A case report and review of the literature. Spine (Phila Pa 1976) 2014;39:413-6. [Google Scholar]
- 14.Menéndez P, García A, Peláez R. Absceso paravertebral e intraabdominal secundario a ozonoterapia por lumbalgia [Paravertebral and intra-abdominal abscess due to oxygen-ozone therapy for lower back pain]. Rev Esp Cir Ortop Traumatol 2014;58:125-7. [Google Scholar]











