Use of tantalum metal cones can be considered for reconstruction of segmental distal femoral bone defects, in native and periprosthetic cases.
Dr. Alan W Reynolds,
Department of Orthopedic Surgery, Allegheny General Hospital, Pittsburgh, Pennsylvania, United States.
E-mail: alan.reynolds@ahn.org
Introduction: Segmental bone loss in the distal femur presents a challenge for reconstruction regardless of etiology. Use of tantalum trabecular metal cones with intramedullary fixation and autologous bone graft may be used as a salvage technique in difficult situations where other options have either been exhausted or are unavailable.
Case Report: Surgical planning and technique for this approach to reconstruction are described. A retrospective review of five cases with >1 year of follow-up was performed to provide radiographic and clinical outcomes. All five patients had satisfactory outcomes with clinical union and retention of implants at final follow-up (average >4 years).
Conclusions:Use of tantalum metal cones for reconstruction of distal femur nonunion with segmental bone defects can be a successful technique in a complex group of patients.
Keywords: Femur, bone defect, non-union, induced membrane, tantalum.
Segmental bone loss in the post-traumatic and nonunion setting is a challenging problem in long bones of the lower extremity. Initial management often requires adequate treatment and resolution of infection, open fractures, soft-tissue damage and coverage, neurovascular deficits, and concomitant injuries or implant failures. After stabilization of the patient and once the site of injury is acceptable for definitive skeletal reconstruction and fixation, critical bone loss presents a dilemma in and of itself. No consensus has been approached in terms of management of these bone defects [1, 2, 3, 4, 5, 6]. Many different approaches have been attempted but with limited or varying data to support their use. Perhaps the most popular would be the induced membrane technique, although this has shown relatively poor results in some reports, as well as others that have found outcomes to be more consistent [7, 8]. Other treatment options rely on the size of the defect, potential availability of iliac crest autograft, fibula autograft (both vascularized and nonvascularized), as well as allograft [9, 10, 11, 12]. In addition, distraction osteogenesis, acute shortening, and amputation are possible options [13, 14]. In addition to these approaches, many biologic adjuncts have been used including bone marrow aspirate, reamer-irrigator-aspirator (RIA) bone graft, demineralized bone matrix, bone morphogenic proteins, and platelet-rich plasma [3, 15]. All of these approaches and combinations of techniques attempt to achieve a reconstruction construct that is both structurally stable and biologically capable of healing. One method that has addressed this issue in the arthroplasty setting is the use of tantalum trabecular metal for metaphyseal bone loss [16, 17]. These biocompatible implants provide a porous osteoconductive scaffold and provide additional structural support. Tantalum cone augments have a modulus closer to the stiffness of bone when compared to other solid metal implants or cement possibly leading to an environment more conducive to bone formation. Initial studies in the arthroplasty setting have shown promising outcomes for this technique [18]. In theory, this approach combined with stable internal fixation may be effective for management of post-traumatic and nonunion segmental bone defects in some cases. We have had success with the off-label use of the tantalum trabecular metal augments at our institution. We would first recommend the usual well-known techniques of internal fixation and bone grafting of the bone defect. Our described technique would be optional when the bone loss is greater than 3.5 cm, autologous bone graft material is limited, or the patient will not tolerate shortening or bone transport. We have been more liberal to perform this technique in the elderly with or without knee arthroplasty. This technique has been helpful to allow early weight bearing and to avoid distal femoral replacement. This paper presents our technique as well as a case series of five patients and their outcomes.
For each patient, standard radiographs are obtained including anterior-posterior (AP) and lateral views of the femur. The radiographs were evaluated for nonunion, implant positioning, loosening or broken implants, peri-implant lucency, and size of bone defect. Computed tomography (CT) of the femur was occasionally obtained but not necessary. Defects that may be amenable to trabecular metal cone with bone grafting are those with bone defects that are not amenable to shortening but have a critical bone defect in the metadiaphyseal distal femur of 3.5 cm or greater. The pre-operative X-rays are templated to match the proximal and distal canal cortices at the defect site to a similar sized trabecular cone. We have found that either the femoral or tibial cones are satisfactory, but the tibial cones match the cortical relationships of the distal femur resulting in a more stable construct. In defects >3.5 cm, some shortening may be accepted, augments maybe stacked to gain length, or a custom shaped trabecular metal shape may be ordered in the preoperative period.
The patients also had the following labs obtained if evaluated for nonunion or infection: complete blood count, erythrocyte sedimentation rate, and C-reactive protein. Active infection is a contraindication to this technique. If the patient demonstrated an infection or there is a concern for infection, the procedure was staged. The implantation of the cone and revision fixation was performed when the infection was ruled out or adequately treated. All patients were consented for the off-label use of tantalum trabecular metal augments (Zimmer Biomet, Warsaw, IN, USA) and bone-grafting from either RIA or autologous iliac crest bone grafting.
The prior incisions are used including the straight midline incision with a medial parapatellar arthrotomy or lateral approach. The nonunion site or site of segmental bone defect is exposed and debrided mechanically until healthy bleeding bone is present. Bone biopsies and cultures are also obtained. At this time, any prior implants that may interfere are removed (e.g. intramedullary nail, cables, or plates) making sure to size the amount of bone defect present. A debridement of the defect with the tourniquet down allows for evaluation of viable and nonviable regions of bone. The medullary canals of the nonunion site are opened to establish adequate vascularity, often using a reamer. Any reasonable bone that was debrided may be used to supplement the autograft. A motorized burr may also be used for debridement but great care is taken to avoid thermal injury of the bone.
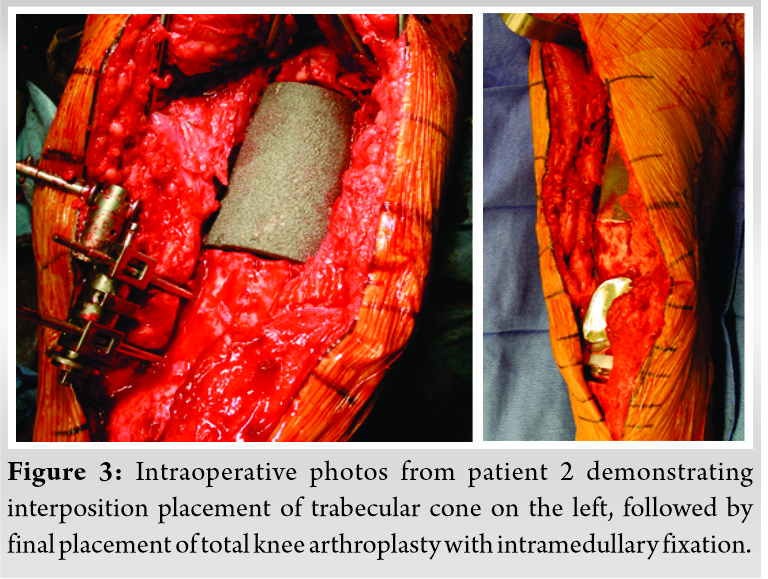
Bone graft may be harvested from multiple donor sites during the procedure. A RIA may also be used to obtain autologous bone graft from the ipsilateral femur or tibia with the tourniquet deflated. The contralateral femur may also be an option but is routinely avoided. After femoral reaming, a lamina spreader is used to open the defect site for sizing. The longitudinal length of the defect is then matched to the length trail cone. The medial to lateral width of the bone, metaphysis or diaphysis, was matched to the appropriately sized dimensions of the trabecular metal cone. The actual cone is placed after a small amount of the bone graft is used as a slurry at the interface between the bone and cone. A supplemental spanning 3.5 locking plate can be also used to temporarily stabilization the cone. The limb is checked for appropriate length, alignment, and rotation. The construct is confirmed on an AP/lateral intraoperative X-ray. A retrograde intramedullary nail is then carefully positioned through the trabecular metal cone to avoid displacement. A retrograde nail may not be possible if there is a femoral component without an open box in which case a lateral plate may be used. A blocking screw can also be considered if the trabecular metal cone or fracture is malpositioned. The construct is then assessed for stability and compressed either with a plate, impaction of the distal cross locked nail, compression device, or compression through an AO distractor. The proximal cross-locks of the nail are finally placed. The remaining bone graft is packed around the cone. Standard wound closure was completed and subcutaneous drains may be of use if there is an abundant adipose layer.

The patients are made touch-down weight bearing with a knee-immobilizer or hinged-knee brace locked in extension for 2 weeks to allow incision healing. Antibiotics are continued for 24 h postoperatively. The drains are removed by the 2nd postoperative day. All patients were mobilized on postoperative day 1 by the physical therapist. They were kept touch-down weight bearing for 6 weeks, and gradually progressed to full weight bearing by 12 weeks. Home range of motion exercises was encouraged after staple removal and formal outpatient physical therapy was deferred until at least 4 weeks postoperatively. All patients received low molecular weight heparin for deep vein thrombosis chemoprophylaxis. Nonsteroidal anti-inflammatory was avoided to minimize risk to bone healing.
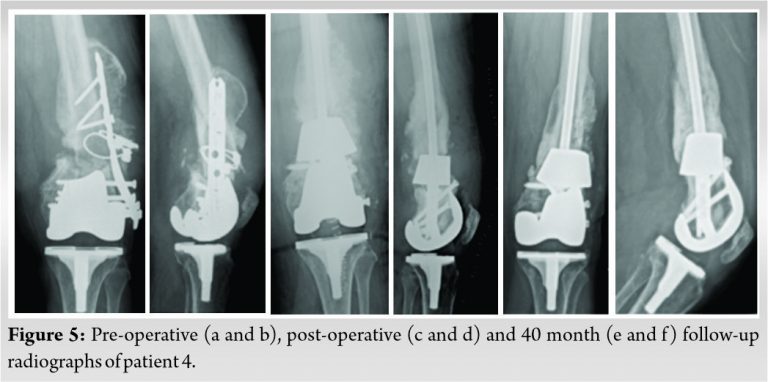
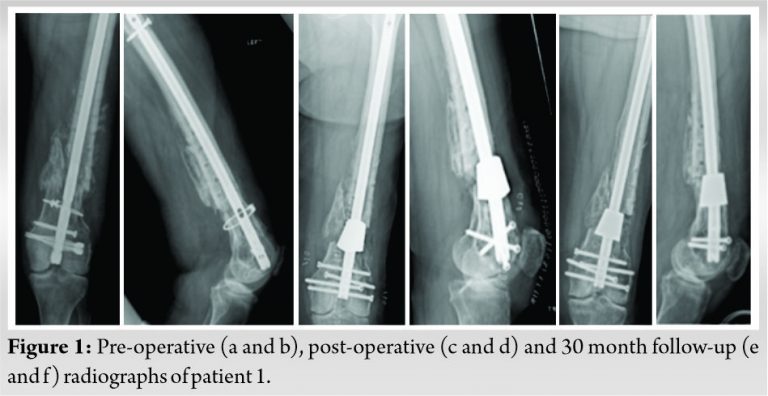
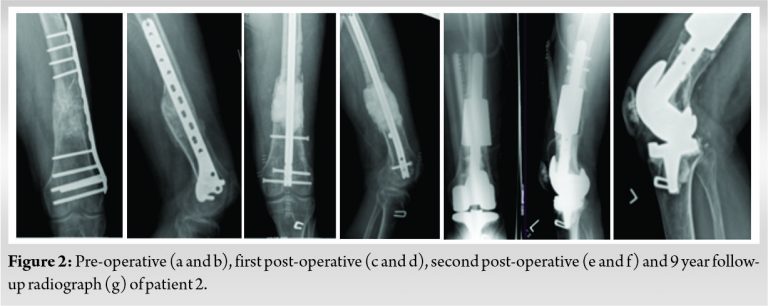
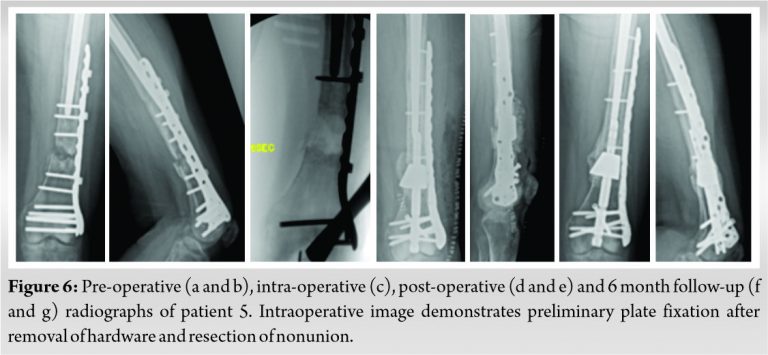
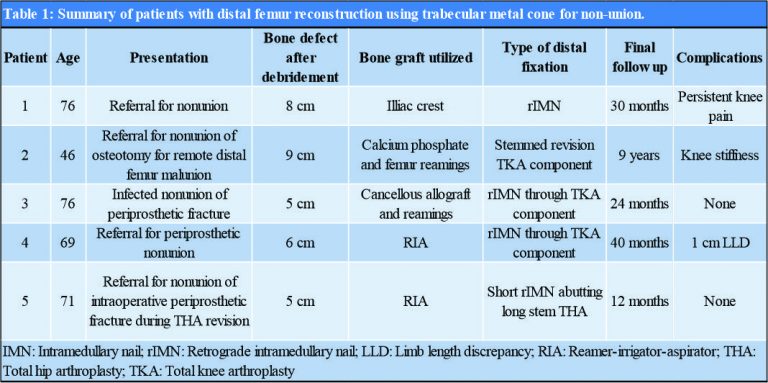
A small case series is presented in this report. Details of these patients and procedures are shown in (Table 1). All five cases were performed as salvage procedures for distal femur metadiaphyseal nonunions. In three cases, these were proximal to a total knee arthroplasty, while one case was distal to a long stem revision total hip arthroplasty component and one case with a previous intrameduallary nail. In all cases, prior hardware used initially to treat the fracture was removed. All patients were non-smokers and none were diabetic. Four of the patients presented initially to an outpatient clinic for care of nonunion after initial treatment at outside facility. All patients had minimum 1 year follow-up and had achieved union and remained ambulatory at that time with no revision surgery. All but one of the patients has been followed for over 2 years. Pre-operative and post-operative radiographs for each patient are shown in (Fig. 1, 2, 3, 4, 5, 6). Intraoperative images from patient 2 are shown in (Fig. 3). One of these cases was performed for infected nonunion (Patient 3). In this case, the patient initially underwent irrigation and debridement with removal of hardware and placement of antibiotic cement in the bone defect. They completed 6 weeks of IV antibiotics and after 4 months, revision with trabecular metal cone and final fixation was performed after verifying no ongoing signs of infection, including normalized inflammatory markers.
Treatment of post-traumatic and nonunion segmental bone loss presents a challenging problem in patients who are at high risk for complications. The case series reported here represents successful application of a technique used at our institution for these cases. Fortunately, in these cases good outcomes and fracture healing have been obtained. Inevitably, as the technique continues to be used there will likely be failures as well. It is worth pointing out that patient selection likely played a role in the successful outcomes in this series. All patients undergoing these significant reconstructions were non-smokers with no significant medical co-morbidities. Considering the complexity of these procedure and the problems that they are addressing, we find it relatively acceptable to have the minor complications that are listed in (Table 1), including on ongoing knee pain requiring cortisone injections and a 1 cm limb length discrepancy.
The described technique does haves several theoretical and practical advantages which are worthy of discussion. In terms of the material of the trabecular metal cone that is used, this offers an osteoconductive surface while also providing structural support with a modulus that is closer to bone than that of cement or solid metal implants. In addition, the hollow nature of it allows for the use of intramedullary fixation. From a technical standpoint, one significant advantage over the induced membrane technique is that it can be completed in 1 surgery, alleviating both patient morbidity, risk of complications, as well as costs. In addition to this, the structural nature of the implant (including the combination of intramedullary fixation), allow for a breadth of bone autograft options that can fit patient and surgeon preference since a structural autograft (or allograft) is not required. As previously mentioned, this technique is limited to a narrow subset of patients; however, it does provide a practical solution to a difficult clinical problem. We anticipate that similar techniques will become more prevalent in the future, especially if more tailored implants are made available, including custom implants for similar applications.
Use of tantalum metal cones for reconstruction of distal femur fractures and nonunions with segmental bone defects has been a successfully used technique at our institution. Further use and study of it is worthy of consideration in patients with complex distal femoral bone loss.
Reconstruction of distal femur fractures and nonunions is a challenge especially in the presence of bone loss, previous infection, and previously placed implants. Use of tantalum metal cones for segmental bone defects in these cases provides a reliable, structural building block that has yielded excellent clinical results in our experience.
References
- 1.Mitchell SE, Keating JF, Robinson CM. The treatment of open femoral fractures with bone loss. J Bone Joint Surg Br 2010;92:1678-84. [Google Scholar]
- 2.Mauffrey C, Barlow BT, Smith W. Management of segmental bone defects. J Am Acad Orthop Surg 2015;23:143-53. [Google Scholar]
- 3.Nauth A, Schemitsch E, Norris B, Nollin Z, Watson JT. Critical-size bone defects: Is there a consensus for diagnosis and treatment? J Orthop Trauma 2018;32:S7. [Google Scholar]
- 4.Ma CH, Chiu YC, Tu YK, Yen CY, Wu CH. Three-stage treatment protocol for recalcitrant distal femoral nonunion. Arch Orthop Trauma Surg 2017;137:489-98. [Google Scholar]
- 5.Sivakumar R, Mohideen MG, Chidambaram M, Vinoth T, Singhi PK, Somashekar V. Management of large bone defects in diaphyseal fractures by induced membrane formation by Masquelet’s technique. J Orthop Case Rep 2016;6:59-62. [Google Scholar]
- 6.Ayouba G, Lemonne F, Kombate NK, Bakriga B, Edem JY, Max UA. Interest of nailing associated with the Masquelet technique in reconstruction of bone defect. J Orthop 2020;20:228-31. [Google Scholar]
- 7.El-Alfy B, Abulsaad M, Abdelnaby WL. The use of free nonvascularized fibular graft in the induced membrane technique to manage post-traumatic bone defects. Eur J Orthop Surg Traumatol Orthop Traumatol 2018;28:1191-7. [Google Scholar]
- 8.Giotikas D, Tarazi N, Spalding L, Nabergoj M, Krkovic M. Results of the induced membrane technique in the management of traumatic bone loss in the lower limb: A cohort study. J Orthop Trauma 2019;33:131-6. [Google Scholar]
- 9.D’Agostino P, Stassen P, Delloye C. Post-traumatic bone loss of the femur treated with segmental bone allograft and bone morphogenetic protein: A case report. Acta Orthop Belg 2007;73:396-9. [Google Scholar]
- 10.Wei FC, El-Gammal TA, Lin CH, Ueng WN. Free fibula osteoseptocutaneous graft for reconstruction of segmental femoral shaft defects. J Trauma 1997;43:784-92. [Google Scholar]
- 11.Jean JL, Wang SJ, Au MK. Treatment of a large segmental bone defect with allograft and autogenous bone marrow graft. J Formos Med Assoc Taiwan Yi Zhi 1997;96:553-7. [Google Scholar]
- 12.Ridha H, Bernard J, Gateley D, Vesely MJ. Reconstruction of large traumatic segmental defects of the femur using segmental allograft with vascularized fibula inlay. J Reconstr Microsurg 2011;27:383-90. [Google Scholar]
- 13.Barinaga G, Beason AM, Gardner MP. Novel surgical approach to segmental bone transport using a magnetic intramedullary limb lengthening system. J Am Acad Orthop Surg 2018;26:e477-82. [Google Scholar]
- 14.Wozasek GE. Limb salvage in a partially amputated distal femur with extensive segmental bone loss using the nailing after lengthening technique: A case report. Strateg Trauma Limb Reconstr 2015;10:59-63. [Google Scholar]
- 15.Stafford PR, Norris BL. Reamer-irrigator-aspirator bone graft and bi Masquelet technique for segmental bone defect nonunions: A review of 25 cases. Injury 2010;41 Suppl 2:S72-7. [Google Scholar]
- 16.de Mozella AP, Olivero RR, Alexandre H, Cobra AB. Use of a trabecular metal cone made of tantalum, to treat bone defects during revision knee arthroplasty. Rev Bras Ortop 2014;49:245-51. [Google Scholar]
- 17.Meneghini RM, Lewallen DG, Hanssen AD. Use of porous tantalum metaphyseal cones for severe tibial bone loss during revision total knee replacement. Surgical technique. J Bone Joint Surg Am 2009;91 Suppl 2 Pt 1:131-8. [Google Scholar]
- 18.You JS, Wright AR, Hasegawa I, Kobayashi B, Kawahara M, Wang J, et al. Addressing large tibial osseous defects in primary total knee arthroplasty using porous tantalum cones. Knee 2019;26:228-39. [Google Scholar]











