Burkholderia pseudomallei is a rare case of septic arthritis knee and it should keep in mind for prompt diagnosis and treatment.
Dr. Mohit Singh,
Department of Orthopedics,
Lady Hardinge Medical College and SSK Hospital, New Delhi, India.
E-mail: mohitsuryawanshi007@gmail.com
Introduction: Melioidosis is an infection caused by the bacterium Burkholderia pseudomallei, which is more frequent in Southeast Asia and Australia but less prevalent in India. Melioidosis-related septic arthritis is extremely rare and should be considered a differential diagnosis in any patient presenting with septic arthritis in endemic locations.
Case Report: Here is a case report of a 42-year-old male from the Andaman and Nicobar Islands who presented with a history of fever along with knee swelling. He had a history of uncontrolled Diabetes Mellitus. Following an emergency arthrotomy, a synovial fluid culture revealed B. pseudomallei, and the patient gradually recovered after receiving ceftazidime via parenteral administration.
Conclusion: This case not only highlights the possibilities of Melioidotic septic arthritis but also validates the importance of prompt administration of appropriate antibiotics for faster recovery from the rare organism B. pseudomallei.
Keywords: Septic arthritis, Burkholderia pseudomallei, Melioidosis.
Septic arthritis is a common medical emergency often associated with substantial morbidity and mortality [1]. Septic arthritis has a case fatality rate of 5–15%, and it can lead to an irreversible loss of joint function in 25–50% of those who survive [2]. The most prevalent route is hematogenous spread, followed by direct inoculation caused by trauma or iatrogenically. Staphylococcus aureus and Streptococcus species are the most common Gram-positive bacteria found worldwide, although Gram-negative bacteria like Escherichia coli and Pseudomonas are also common among elderly patients simultaneous suffering from recurrent urinary tract infection.
Melioidosis is a fatal disease, most prevalent in South-East Asia, northern Australia, but less common in the Indian subcontinent [3]. It is caused by Gram-negative saprophyte Burkholderia pseudomallei. The common presentations include pneumonia (most common), skin infection, genitourinary infections, and septicemia with a distant focus [4]. It has high mortality rates ranging from 14% to 40% despite optimal therapy with high recurrence rates [3, 4]. Septic arthritis due to Melioidosis is very rare and should be a differential diagnosis in a patient presenting with septic arthritis in endemic areas. B. pseudomallei is intrinsically resistant to a wide range of antimicrobials, including gentamicin and most third-generation cephalosporins except ceftazidime. Effective parenteral antibiotics include ceftazidime and carbepenem [5, 6]. Diabetes Mellitus (DM) is the most important risk factor and is found in about 50% of Melioidosis patients [7]. Other known risk factors include exposure to soil or water, male gender, older age, excess alcohol consumption, chronic liver disease, chronic lung disease, chronic renal disease, and thalassemia [6].
Burkholderia is an uncommon cause of knee septic arthritis in the mainland of India. Although Andaman and Nicobar Islands are located in the Southern part of Asia, this rare organism (B. pseudomallei) has shown morphological and infectious similarities with other endemic countries of South-east Asia (Thailand and Singapore). Herein, we describe a case report of septic arthritis that has presented to a tertiary referral hospital in the Andaman and Nicobar Islands (Union Territory of India).
A 42-year-old male patient farmer by occupation from the Northernmost part of Andaman and Nicobar Island was admitted to the orthopedic ward with complaints of left knee swelling, pain, and high-grade fever of 1-week duration. The swelling started first followed by high-grade fever and pain. The swelling rapidly developed and progressed. The pain was mild, dull aching, insidious in onset without any radiation, aggravated by movements and relieved by rest and analgesics, and gradually worsened with time disabling him for day-to-day activities. The fever was high grade continuous in nature, with chills and rigors, without any diurnal variation or any upper respiratory tract infection, and relieved with antipyretic. There was no history of trauma, loss of appetite, night sweats, or contact with tuberculosis (TB).
Clinically, there was a local rise of temperature at the left knee and redness. There were no sinus tracts. The knee was swollen with the fullness of the suprapatellar pouch. The range of motions was painful and limited. The knee joint was held in slight flexion (comfort position) (Fig. 1).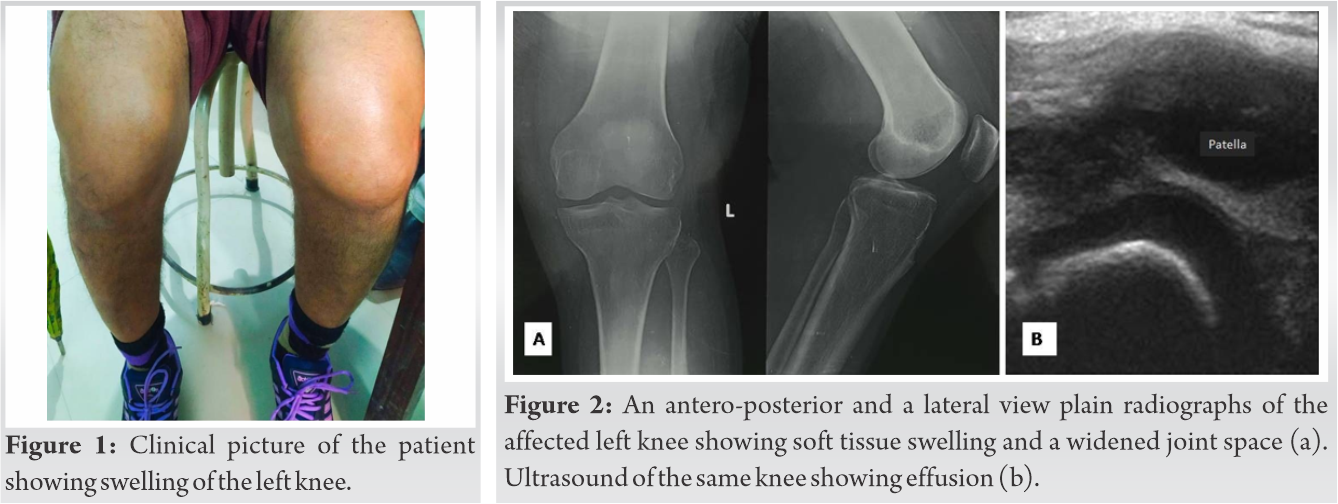
Laboratory findings showed his hemoglobin was 11.2 gm/dL, ESR was 62 mm/h, C-reactive protein level was 96 mg/L. His serology was negative for HIV. The patient had uncontrolled diabetes with a fasting sugar of 192 mg/dL, postprandial sugar of 288 mg/dl, and HbA1c of 10.5%. He was a known case of Type 2 DM and was not compliant with treatment. Plain radiograph of the left knee showed localized soft tissue swelling with obliteration of soft tissue plane without any severe joint space narrowing or bony destruction (Fig. 2a). Ultrasonogram of the left knee showed a subcutaneous localized collection with septate loculations and intraarticular effusion (Fig. 2b). Computed tomogram, magnetic resonance image scans were not sought as the clinical and radiological evidence pointed toward localized collection.
An aseptic technique was used with a local anesthesia infiltration. Aspiration of the knee joint revealed 20 mL of frank pus. The affected joint’s synovial fluid was sent for regular microscopy, culture, and sensitivity testing. Routine microscopy and cytology with gram staining revealed gram-negative bipolar rod-shaped bacilli and leukocyte count of 28,800/mL (with 95% polymorphs and 5% lymphocytes) (Fig. 3a, b).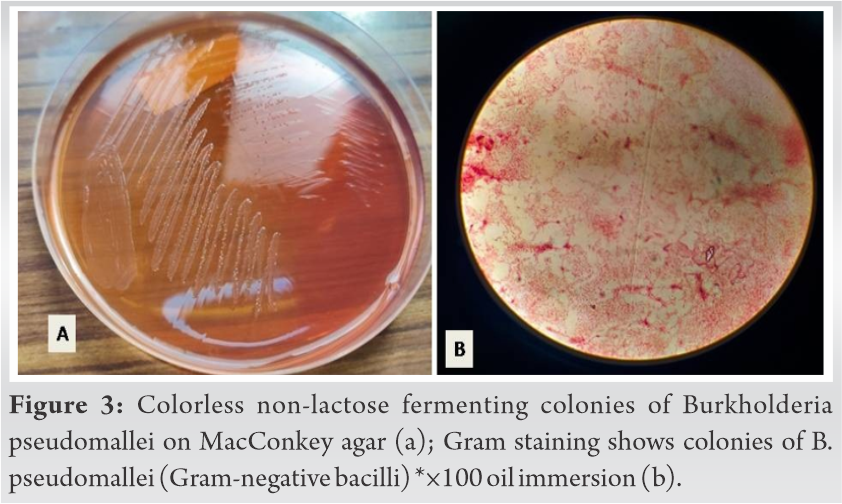
An emergency arthrotomy was done, the joint was washed thoroughly and samples were sent for culture and sensitivity. Blood samples were taken for blood cultures then intravenous linezolid and amikacin were started which provided gram-positive and gram-negative coverage while waiting for culture reports. But there were no signs of recovery, with frequent spikes of fever, chills, and rigors for 3 days. The culture report came out after 3 days. It showed growth of B. pseudomallei which was sensitive to intravenous Carbapenems and ceftazidime. Treatment was started according to the culture and sensitivity reports with intravenous ceftazidime (2 gm) 8 hourly, and the signs and symptoms of the patient started improving. At the end of the 10th day, his knee range of motion increased dramatically and the patient’s condition improved symptomatically. Intravenous antibiotic treatment was continued for 3 weeks at the hospital as his home was far away from the hospital with poor medical access. The patient was discharged on oral cotrimoxazole and doxycycline for 5 weeks.
Melioidosis is a severe systemic illness caused by B. pseudomallei, a gram-negative, bipolar, aerobic motile rod-shaped bacterium. Commonly found in soil, groundwater, and ponds in endemic regions. It spreads to people by percutaneous inoculation when working in these locations without wearing protective gear or footwear, resulting in an illness with a high case fatality rate. Diabetes, TB, chronic renal illness, heavy alcohol intake, and steroid usage are some of the risk factors. It can manifest in a variety of ways, from asymptomatic infection to localized abscess development. This may cause fulminating illness involving many organs and even death. Culture sensitivity of blood, pus, or body fluids is the gold standard diagnostic test. Imaging studies are not always specific and might be mistaken for other bacterial infections. The clinical diagnosis of the condition is not so specific. Although musculoskeletal melioidosis is well-known, it is uncommon even in endemic areas [7].
In India, most melioidotic septic arthritis cases have so far been reported from the southern states such as Kerala and Tamil Nadu. Isolated cases have also been reported from eastern and northeastern parts of India. Melioidosis is prevalent but under-reported may be because of a low index of suspicion and lack of proper diagnostic facilities [8]. We are reporting first time from Portblair, Andaman and Nicobar Island. Perumal et al. [9] in their observation found 342 (9.2%) patients infected with B. pseudomallei bacteria and only 37 patients had musculoskeletal involvement. Jesudason et al. [8] reported three cases of melioidotic septic arthritis from south India with a proven synovial fluid culture which responded well to ceftazidime, cotrimoxazole, and imipenem, similar to antibiotic sensitivity found in our case. Pandey et al. [10] literature review showed 10% local relapse of symptoms even after 20 weeks of treatment, however, the relapse rate increased to 30% when the duration of the treatment was less than 8 weeks. Gopalakrishnan et al. [11] in their study found alcohol and DM as the two most common factors associated with melioidosis and excellent outcome of treatment with parenteral use of ceftazidime. Shetty et al. [12] noted that most patients with musculoskeletal melioidosis needed operative intervention and those with multifocal bone and joint involvement needed significantly longer hospital stay and more operations. As routine antibiotics are seldom beneficial, melioidosis should always be there in our mind as a rare differential diagnosis for septic arthritis not responding to normal antibiotics and in patients with associated risk factors such as DM as in this case.
We conclude that when a septic arthritis is not responding to regular antibiotics, challenging our clinical diagnosis and treatment modalities, we should consider the possibilities of rare organisms as a causative agent such as Burkholderia in endemic areas of the Indian subcontinent.
Melioidosis is not only so common in India but also early and correct diagnosis and institution of proper and prompt antimicrobial therapy are important to reduce morbidity and mortality and have a favorable outcome.
References
- 1.Mathews CJ, Weston VC, Jones A, Field M, Coakley G. Bacterial septic arthritis in adults. Lancet 2010;375:846-55. [Google Scholar]
- 2.Goldenberg DL. Septic arthritis. Lancet 1998;351:197-202. [Google Scholar]
- 3.Shirtliff ME, Mader JT. Acute septic arthritis. Clin Microbiol Rev 2002;15:527-44. [Google Scholar]
- 4.Thin RN, Brown M, Stewart JB, Garrett CJ. Melioidosis: A report of ten cases. Q J Med 1970;39:115-27. [Google Scholar]
- 5.Dance D. Treatment and prophylaxis of melioidosis. Int J Antimicrob Agents 2014;43:310-8. [Google Scholar]
- 6.Jain VK, Jain D, Kataria H, Shukla A, Arya RK, Mittal D. Melioidosis: A review of orthopedic manifestations, clinical features, diagnosis, and management. [Google Scholar]
- 7.Cheng AC, Currie BJ. Melioidosis: Epidemiology, pathophysiology, and management. Clin Microbiol Rev 2005;18:383-416. [Google Scholar]
- 8.Jesudason MV, Anbarasu A, John TJ. Septicaemicmelioidosis in a tertiary care hospital in south India. Indian J Med Res 2003;117:119-21. [Google Scholar]
- 9.Perumal R, Livingston A, Samuel S, Govindaraju SK. Melioidosis of the musculoskeletal system. Med Princ Pract 2020;29:121-7. [Google Scholar]
- 10.Pandey V, Rao SP, Rao S, Acharya KK, Chhabra SS. Burkholderia pseudomallei musculoskeletal infections (melioidosis) in India. Indian J Orthop 2010;44:216 [Google Scholar]
- 11.Gopalakrishnan R, Sureshkumar D, Thirunarayan MA, Ramasubramanian V. Melioidosis: An emerging infection in India. J Assoc Physicians India 2013;61:612-4. [Google Scholar]
- 12.Shetty RP, Mathew M, Smith J, Morse LP, Mehta JA, Currie BJ. Management of melioidosis osteomyelitis and septic arthritis. Bone Joint J 2015;97:277-82. [Google Scholar]










