Limb deformity and leg length discrepancy after infantile meningococcal infection, can be managed with distraction osteogenesis with the Ilizarov device.
Dr. Nikolaos Laliotis, Pediatric Orthopaedic Surgeon, M.Ch.Orth, f Assistant Professor in Pediatric Orthopaedics E-mail: nicklaliotis@gmail.com
Introduction:Residual orthopedic deformities after meningococcal infection in infancy, including severe angular deformities and leg length discrepancy (LLD), affect patient quality of life.
Case presentation:We report the case of an adolescent female with severe varus deformity and LLD of her right femur. We applied a preconstructed Ilizarov frame and initially corrected the varus deviation with different rates of rod elongation and appropriate hinges. We then completed the correction by performing usual lengthening procedures to address the LLD.
Conclusion:Treatment with distraction osteogenesis with the Ilizarov frame enabled the restoration of the anatomical axis and severe LLD of the legs.
Keywords:meningococcal infection, leg length discrepancy, varus deformity, Ilizarov frame, distraction osteogenesis.
Meningococcal infection is a severe disease that can occur during infancy. Children that survive the infection may develop severe orthopedic problems, mainly affecting the lower limbs. Vascular occlusive lesions affect the normal development of the metaphysis, growth plate, and epiphysis. Lesions of the growth plate result in growth arrest and leg length discrepancy (LLD) with angular deformities [1-5].
We report the case of an adolescent girl who was referred for the management of severe sequelae including LLD and varus deformity affecting her right femur. After radiological assessment, she was surgically treated for limb reconstruction with distraction osteogenesis using the Ilizarov device. This deformity correction completely changed the activities and attitudes of this young girl.
A 14-year-old adolescent girl was referred to our department for the evaluation of a deformity of her right leg. Her mother described her medical history. The girl was born normally and had been delivered full-term in a country in East Europe.
She was diagnosed with meningococcal infection 3 weeks of age. The diagnosis was confirmed based on the results of cerebrospinal fluid cultures. During the next 6 months, five surgical procedures were performed to drain osteomyelitis and septic arthritis affecting both the proximal and distal parts of the patient’s right femur.
Two additional surgical procedures for osteomyelitis of the distal femur were performed when the patient was 2 and 4 years of age.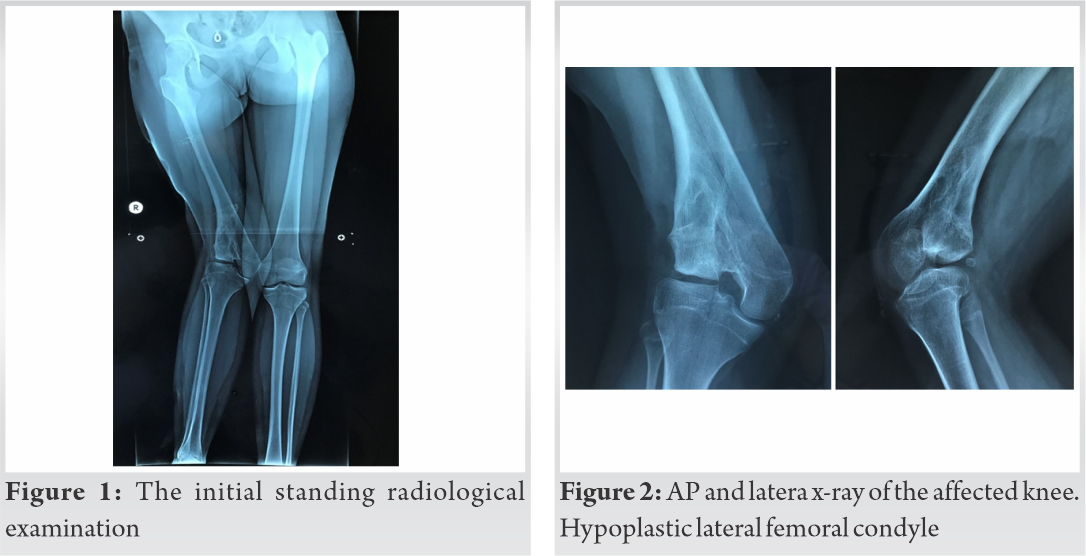
There was an obvious varus deformity in her leg as well as LLD. The length discrepancy was 7.5 cm, as measured by computed tomography (CT). The discrepancy almost completely affected the femora (35 cm left–28 cm right), while the tibia differed in length by <0.5 cm. The knee flexion was limited to 90°, while the knee had hyperextension to 10° with a slight recurvatum shape.
X-ray examination revealed a distorted and hypoplastic distal lateral femoral condyle and normal-appearing intercondylar notch and medial femoral condyle. The distal femoral growth plate appeared only in the medial part of the distal femur. The proximal tibial growth plate appeared normal and symmetrical. The growth plates showed radiological signs of closure. The patient’s foot shape and ankle joint movements were normal. She had no skin contractures apart from the incisions resulting from the surgical procedures. A bone scan showed negative uptake in the femur.
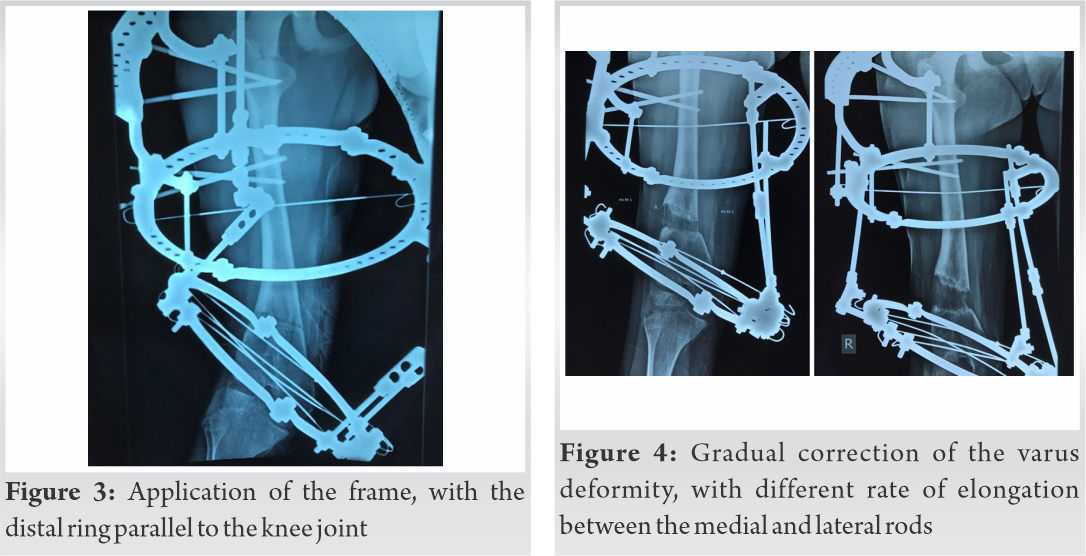
After completing the evaluation and counseling with her parents, we proceeded with a surgical intervention using a pre-constructed Ilizarov frame.
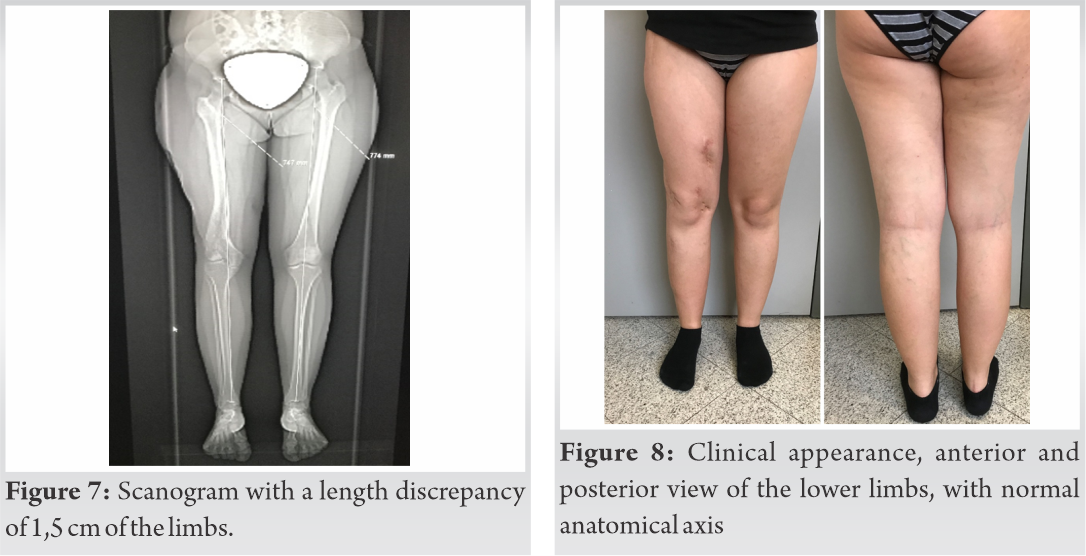
We used two central and one distal ring connected with universal hinges. The plane of the ring application was proximally perpendicular to the axis of the femur. The distal ring was parallel to the knee joint and had a 10° recurvatum. We performed the osteotomy and started the lengthening procedure on the 5th day. Initially, distraction was performed two and four times daily for the lateral and medial rods, respectively. We achieved correction of the mechanical axis in 4 weeks and then completed the lengthening procedure with similar rates of distraction for both the medial and lateral rods four times daily.
We completed the regeneration process with almost equalization of the leg discrepancy and restoration of the mechanical axis of the femur. During the lengthening procedure, the girl noted the change in the shape of her leg and was satisfied and cooperative. She was weight-bearing using crutches. Her knee flexion remained limited despite efforts to increase it, even though we did not include the tibia in the device. Radiological evaluation was performed every 10 days to assess the progress of the lengthening procedure and avoid possible knee subluxation. The bone regeneration was uncomplicated and normal ossification of the new bone appeared as expected.
After consolidation of the new bone, we removed the Ilizarov device and protected the limb with a knee brace.
The Ilizarov device was used for 5.5 months. We lengthened the right femur by 6 cm, which was 20% of the initial length. The consolidation period lasted for 2 months. The healing index was 0.9 months/cm.
The patient achieved a knee flexion of 0–100° with exercises and physiotherapy. Her behavior also changed, as she started participating in normal activities and dancing. The 10-year follow-up showed restoration of the normal femoral cortices and normal anatomical axis. There were no radiological signs of abnormalities in the knee joint space. Moreover, the patient showed no clinical signs, with normal knee movements, including squatting.
Meningococcal infection is a cause of morbidity during infancy. This severe infection causes disseminated intravascular coagulation that affects the growth plates. A physeal bar may be formed that connects the metaphysis to the epiphysis. This forms a tethering effect, leading to LLD and angular deviation of the bone [6].
Interestingly, the growth plates of the lower limb are mostly affected, while the upper limbs are rarely affected.
Metaphyseal osteomyelitis and septic arthritis in the knee or hip joint may coexist during infancy. These conditions require an emergency operation for immediate drainage as well as thorough treatment. In meningococcal infection, the process of vascular occlusion leads to further growth plate damage [7, 8].
The initial disappearance and later reappearance of the distal epiphyseal ossification center due to hyper-revascularization after the infection has been described. The reossified epiphysis may appear bifid and irregular, leading to deformity. Early excision of the physeal bar may prevent deformity and LLD, as reported in two of four children with Staphylococcus infection [6].
The clinical signs included LLD and angular deformities at the knee or ankle joint in a cohort of 10 patients with meningococcal septicemia. There are multiple growth plates, most of which affect the proximal and distal tibial growth plates. The authors used either Ilizarov or Taylor spatial frames for the correction of the LLD and angular deformities and combined the procedures with appropriate epiphysiodesis to prevent deformity recurrence [9]. A previous report on 24 children affected by meningococcal septicemia recommended epiphysiodesis while correcting deformities around the knee joint to reduce the high rate of deformity recurrence [10]. Another report described lesions of the distal tibial epiphysis following meningococcal septicemia in 14 children, although the distal fibular physis was not affected in 13 of these patients [11].
The growth plate in our patient was not active and we corrected the angular deformity in both the frontal and sagittal planes using the Ilizarov frame.
A study of 170 patients who survived meningococcal septic shock, reported that late orthopedic sequelae were associated with a high incidence of skin scarring after purpura. Ten patients (8%) underwent amputation. Seven patients had LLD with lesions affecting the growth plates of the femur and tibia. These patients received appropriate orthopedic interventions with osteotomies and epiphysiodesis for the management of the LLD and angular deformities [12].
Orthopedic sequelae after meningococcal septicemia were reported in 13 patients followed over 17 years to skeletal maturity. The typical orthopedic sequela of angular deformities and LLD were reported. Multiple growth plates were involved, generally presenting as focal lesions. Seven physes underwent bar resection, four of which were successful. Complete or premature arrest resulted in LLD, while central or asymmetrical bars had angular deformities and LLD. The leg-lengthening procedures included the Orthofix rail apparatus (three femurs and three tibiae) and the Taylor spatial frame (two tibiae) [4].
We believe that the Ilizarov circular frame provides more options for the simultaneous correction of deformities in both the frontal and sagittal planes. We used different rates of rod elongation, which enabled the simultaneous correction of LLD and varus deviation. After correcting the angular deformity, we continued with the same rate of elongation to correct the LLD. The Taylor spatial frame can provide similar corrections with even more accurate rates. One study reported the correction of a 14-cm LLD, occurring as a late complication of childhood meningococcal sepsis, using an implantable system in two operative steps [13].
A report from New Zealand observed a higher occurrence rate of meningococcal septicemia in lower socioeconomic areas and also described early and late procedures for skin necrosis, gangrene, and contractures in 21 children. Nine of these children underwent amputations. However, only one child developed late sequelae including bilateral genu valgus and LLD, which were treated with osteotomy and use of the Ilizarov frame [14].
Orthopedic consequences were observed in 10 of 130 patients with meningococcal septicemia. Growth plate involvement most often affected the lower limbs (81%), mainly the lower tibia. The authors reported that infections requiring early amputation were more likely to develop growth plate abnormalities. Six patients (4.6%) developed LLDs [5].
In contrast, a study of 48 patients with a follow-up of 11,7 ± 5.1 years reported more frequent growth disturbances in children without amputation. Bone infections from S. aureus were a common complication in children who had undergone knee amputation [1]. This is similar to our patient, who had experienced two Staphylococcus infections after the initial meningococcal infection. While growth plate disturbances reportedly affect the periphery of the proximal tibia plate, their effects on the distal femoral plate is have not been described. Both the central and lateral parts of the distal femoral plate were affected in our patient.
We reconstructed the axis of the limb and restored the LLD in our patient. Despite the radiological inclination of the knee joint, the range of knee movements was almost complete, and the patient continued to enjoy her life at a long follow-up of 10 years after completing the limb restoration.
Severe LLD and angular deviation result from an initial meningococcal infection, with further osteomyelitis infections. The Ilizarov procedure enabled us to restore both the mechanical axis and correct the LLD in our patient.
The late orthopedic sequelae after meningococcal infection include severe deformities and LLDs. We used distraction osteogenesis with the Ilizarov frame to achieve staged correction of the deformity and complete restoration of the LLD. The patient returned to normal physical activities.
References
- 1.Canavese F, Krajbich JI, LaFleur BJ. Orthopaedic sequelae of childhood meningococcemia: management considerations and outcome. J Bone Joint Surg Am. 2010 Sep 15;92(12):2196-203. doi: 10.2106/JBJS.I.01468.PMID: 20844162 [Google Scholar]
- 2.Elrod J, Mannhard D, Mohr C, Lienert C, Hagemann-Gysling K, Schiestl C, Mazzone L . Plastic and Orthopaedic Interventions and Long-Term Sequelae in Children with Meningococcal Septicemia-40 Years of Experience at the University Children's Hospital Zurich. Eur J Pediatr Surg. 2019 Oct;29(5):462-469. doi: 10.1055/s-0038-1673705. Epub 2018 Oct 29.PMID: 30372767 [Google Scholar]
- 3.Monsell F.The skeletal consequences of meningococcal septicaemia. Arch Dis Child. 2012 Jun;97(6):539-44. doi: 10.1136/archdischild-2011-301295. Epub 2012 Feb 3.PMID: 22307988 [Google Scholar]
- 4.du Plessis J-P, Dix-Peek S, Hastings CJ, Loots SB, Hoffman EB. Orthopaedic implications of physeal arrest following meningococcal septicaemia. SA orthop. j. [online]. 2010, vol.9, n.2, pp.67-75. ISSN 2309-8309. [Google Scholar]
- 5.Edwards TA, Bowen L, Bintcliffe F, Aird J, Monsell F The Orthopaedic Consequences of Childhood Meningococcal Septicaemia J Meningitis 2016, Vol 1(2) DOI: 10.4172/2572-2050.1000109 [Google Scholar]
- 6.Peterson HA, Shaughnessy WJ, Stans AA. Physeal bar equivalent. J Pediatr Orthop B. 2017 Nov;26(6):507-514. doi: 10.1097/BPB.0000000000000384. PMID: 27748675 [Google Scholar]
- 7.Montgomery NI, Epps HR. Pediatric Septic Arthritis. Orthop Clin North Am. 2017 Apr;48(2):209-216. doi: 10.1016/j.ocl.2016.12.008.PMID: 28336043 Review. [Google Scholar]
- 8.Quick RD, Williams J, Fernandez M, Gottschalk H et al Improved Diagnosis and Treatment of Bone and Joint Infections Using an Evidence-based Treatment Guideline. J Pediatr Orthop. 2018 Jul;38(6):e354-e359. doi: 10.1097/BPO.0000000000001187.PMID: 29727410 [Google Scholar]
- 9.Park DH, Bradish CF. The management of the orthopaedic sequelae of meningococcal septicaemia: patients treated to skeletal maturity. J Bone Joint Surg Br. 2011 Jul;93(7):984-9. doi: 10.1302/0301-620X.93B7.26128.PMID: 21705576 [Google Scholar]
- 10.Belthur MV, Bradish CF, Gibbons PJ. Late orthopaedic sequelae following meningococcal septicaemia. A multicentre study. J Bone Joint Surg Br. 2005 Feb;87(2):236-40. doi: 10.1302/0301-620x.87b2.14827.PMID: 15736750 [Google Scholar]
- 11.Monsell FP, McBride AR, Barnes JR, Kirubanandan R. Angular deformity of the ankle with sparing of the distal fibula following meningococcal septicaemia: a case series involving 14 ankles in ten children. J Bone Joint Surg Br. 2011 Aug;93(8):1131-3. doi: 10.1302/0301-620X.93B8.26277.PMID: 21768642 [Google Scholar]
- 12.Buysse CM, Oranje AP, Zuidema E, Hazelzet JA, Hop WC, Diepstraten AF, Joosten KF. Long-term skin scarring and orthopaedic sequelae in survivors of meningococcal septic shock. Arch Dis Child. 2009 May;94(5):381-6. doi: 10.1136/adc.2007.131862. Epub 2009 Jan 15.PMID: 19147623 [Google Scholar]
- 13.The correction of a 140 mm lower limb difference as a late complication of a childhood meningococcal sepsis with a fully implantable system. Helfen T, Delhey P, Mutschler W, Thaller PH.J Pediatr Orthop B. 2013 Sep;22(5):498-500. doi: 10.1097/BPB.0b013e3283623b4b.PMID: 23715178 [Google Scholar]
- 14.Wheeler JS, Anderson BJ, De Chalain TM. Surgical interventions in children with meningococcal purpura fulminans--a review of 117 procedures in 21 children. J Pediatr Surg. 2003 Apr;38(4):597-603. doi:10.1053/jpsu.2003.50130.PMID: 12677574 [Google Scholar]