This case report demonstrated the efficacy of the Ilizarov frame in treatment of cases of long standing chronic patella alta in which primary repair is practically impossible due to significant scar tissue formation and quadriceps contracture.
Dr. Amr Abdelgawad, Department of Orthopedic Surgery, Maimonides Medical Center, 6010 Bay Parkway, Brooklyn, NY 11204. E-mail: amratef@doctor.com
Introduction: Chronic patella alta after chronic patellar tendon rupture or patella fracture non-union is a challenging condition to treat.
Case Report: In this report, we present the case of a 50-year-old male with inferior patellar pole fracture with non-union and chronic patella alta from a chain saw accident 12 years before presentation. An Ilizarov frame was used to reduce the patella to anatomic position before reconstructive surgery for knee extensor mechanism repair using an Achilles tendon allograft.
Conclusion: This case demonstrated the efficacy of the Ilizarov frame in the setting of chronic patella alta where primary repair would have been impossible due to significant scar tissue formation and quadriceps contracture.
Keywords: Ilizarov, external fixator frame, chronic patellar tendon rupture, patella alta, Achilles tendon allograft, knee extensor mechanism reconstruction, distraction histogenesis.
Patella alta is an uncommon condition that may be associated with chronic patellar tendon rupture or patella fracture non-union. Common etiologies include sporting events or work-related incidents [1, 2, 3, 4, 5]. Although less common, these injuries can also occur through direct trauma [2]. Most cases are treated promptly with reconstructive surgery using either auto or allografts [4].
Chronic patella alta, defined as >6 weeks between injury and fixation [1], is rarer and associated with greater functional impairment [3, 6]. There is no agreed-on treatment for chronic patella alta, with most of the data coming from case reports and small case series [3, 4, 7]. In this case report, we described the use of an Ilizarov external fixator to reduce an inferior patellar pole fracture with non-union and patella alta 12 years before definitive surgical treatment.
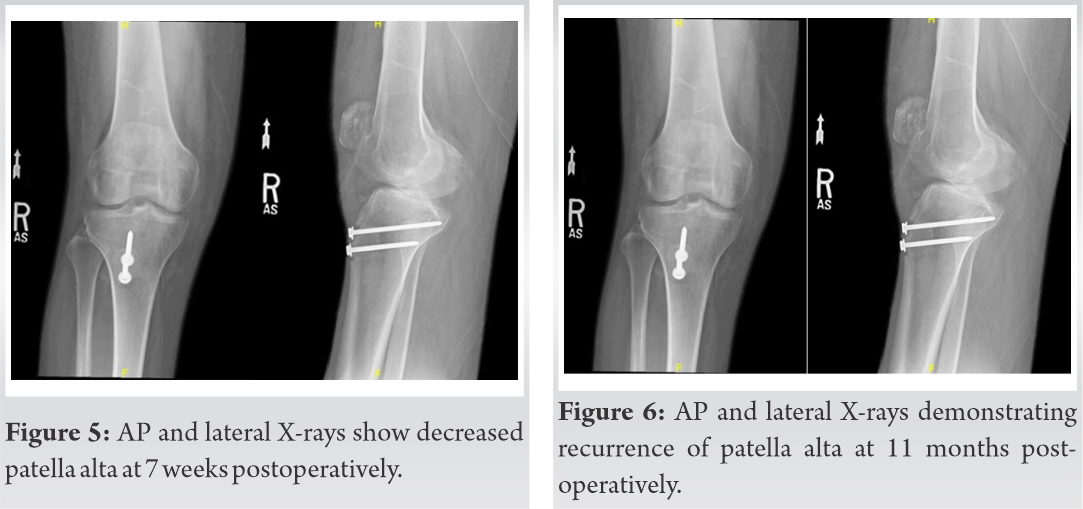
A 50-year-old incarcerated male presented with chronic patella alta sustained from a chainsaw injury 12 years before. On physical exam, he was found to have a well-healed scar over the right knee, a high riding patella, and an inability to extend the right leg. X-ray demonstrated a high riding patella (Fig. 1). The X-ray showed a small bony fragment of the lower pole of the patella, representing an inferior patella pole fracture non-union with marked patella alta and an IS ratio of 2.75. Due to the chronic nature of the injury, severe contracture of the quadriceps muscle, and severe high riding patella, the surgeons elected to use an Ilizarov frame (Fig. 2) for the gradual distraction of the patella to its anatomical location.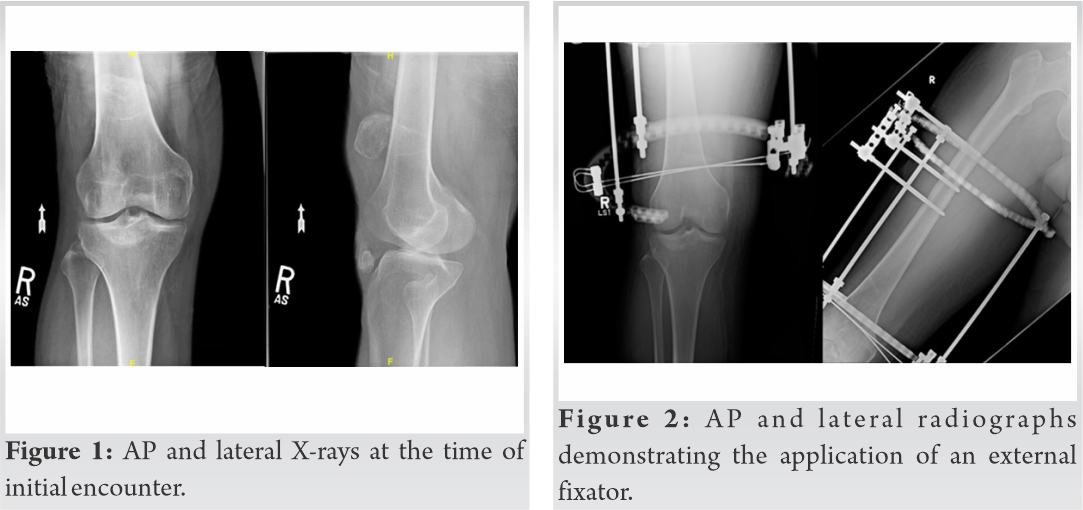 It took approximately 3 months, at a rate of 1 mm/day, to distract the patella to anatomic position (Fig. 3). The frame consisted of a 205 mm TSF (Smith and Nephew, Memphis, TN) full RING and 2/3 205 ring. The 2/3 ring was mounted orthogonal to the femur with two Ilizarov wires inserted into the patella using fluoroscopy to verify their position. The proximal full ring was mounted to the femur. Ilizarov threaded rods were used for gradual distraction. During the distraction phase, the patient developed a deep venous thrombosis (DVT) and pulmonary embolus (PE), requiring medical treatment before surgery.
It took approximately 3 months, at a rate of 1 mm/day, to distract the patella to anatomic position (Fig. 3). The frame consisted of a 205 mm TSF (Smith and Nephew, Memphis, TN) full RING and 2/3 205 ring. The 2/3 ring was mounted orthogonal to the femur with two Ilizarov wires inserted into the patella using fluoroscopy to verify their position. The proximal full ring was mounted to the femur. Ilizarov threaded rods were used for gradual distraction. During the distraction phase, the patient developed a deep venous thrombosis (DVT) and pulmonary embolus (PE), requiring medical treatment before surgery.
The second stage of the reconstruction was performed after the patella reached its anatomic station. The patient underwent patellar tendon reconstruction with an Achilles tendon allograft connecting a bone tunnel in the tibial tubercle (Fig. 4) to three bony tunnels in the patella and reinforced by wrapping the patellar tendon around the quadriceps. Intraoperatively, the patient was found to have a significant amount of scar tissue around the patella and severely osteoporotic bone. Despite severe patella osteoporosis, the patient had no wires cut out or loosening during the distraction phase. Initially, suture anchors were used for the repair of the extensor mechanism; however, due to the patient’s severe osteoporosis they did not hold. Therefore, the authors switched to bone tunnel tendon repair for the proximal site. The patient was immobilized in a long-leg cast. He was discharged on post-operative day 6. The patient was allowed weight-bearing as tolerated for 6 weeks.
The cast was removed 7 weeks post-operative and physical therapy with gentle range-of-motion (ROM) training was begun (Fig. 5). At 11 months post-operative, the patient returned after hearing a “pop” and new extensor lag. On X-ray, the two tibial screws were intact, but there was increased patella alta compared to the previous films (Fig. 6). The re-rupture of the patella tendon was attributed to a lack of adherence to physical therapy and loss of knee range of motion. The patient was scheduled for revision surgery.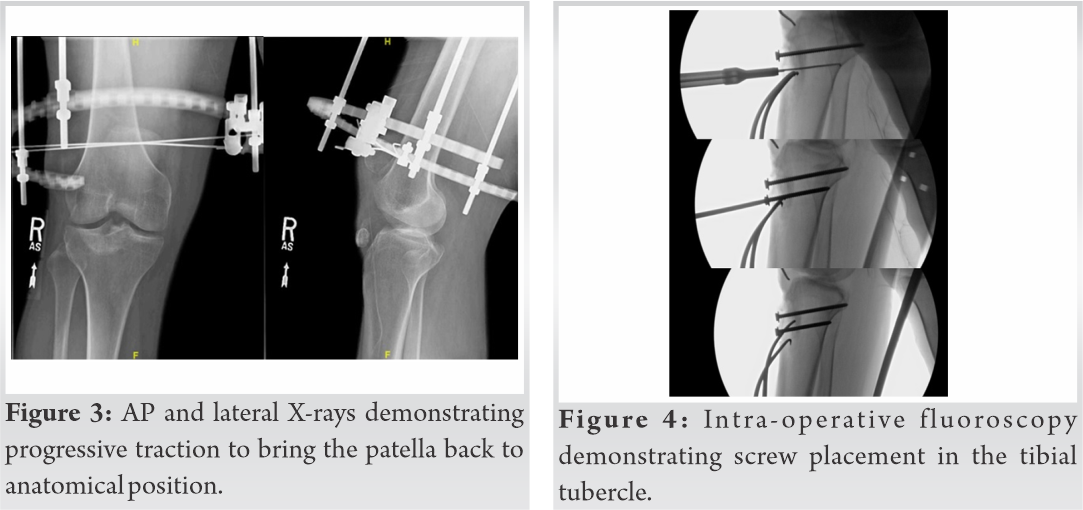
The patient underwent revision surgery with a new Achilles tendon allograft supplemented with an IT band autograft secured to bony tunnels in the patella with Krackow sutures. Intraoperatively, the patient was found to have graft failure with all hardware still in place. At 3 weeks post-operative, he had a ROM of 5–60°, the ability to hold a straight leg raise, and intact active knee extension. X-rays showed intact hardware and improved patella alta (Fig. 7). Over the next 2 months, the patient achieved 5/5 strength, ROM from 0 to 100°, and only a 10° extensor lag with physical therapy. At 5 months postoperatively, the patient had stopped attending physical therapy due to lack of improvement, his active ROM was 10–95°, passive ROM 0–110°. X-ray demonstrated a well-healed knee with all hardware in place. At 22 months post-operative, the patient reported an upward migration of the patella confirmed by X-ray showing the patella 2.5 cm proximal to the femoral condyles (Fig. 8).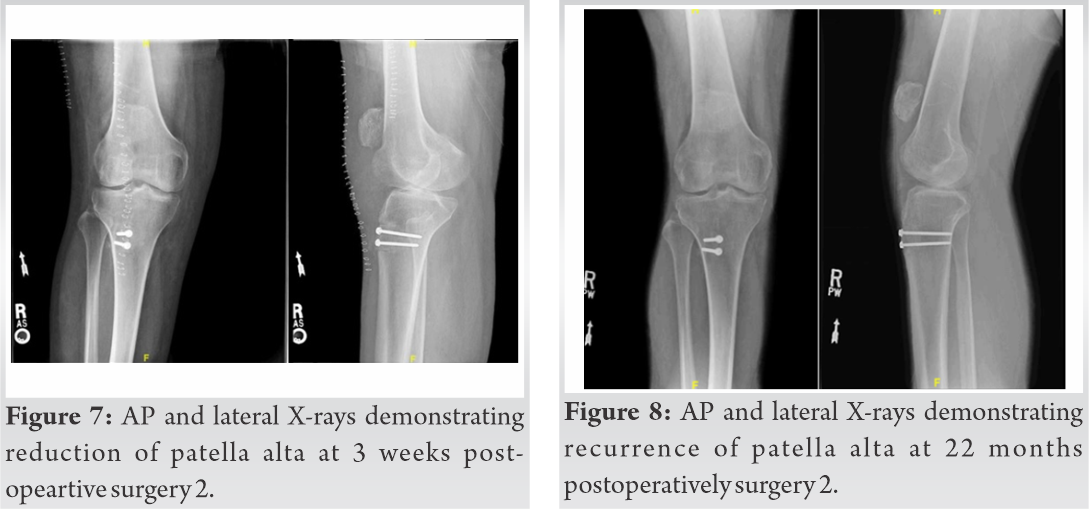 An MRI demonstrated a partial disruption of the patellar tendon at the inferior pole of the patella. He was encouraged to continue weight-bearing as tolerated and quadriceps strengthening exercises with physical therapy. At 32 months post-operative, the patient was functioning well without the use of assistive devices. He had an active ROM of 0–90° (Fig. 9). An X-ray showed changes compared to previous studies (IS ratio 2) (Fig. 10 and 11).
An MRI demonstrated a partial disruption of the patellar tendon at the inferior pole of the patella. He was encouraged to continue weight-bearing as tolerated and quadriceps strengthening exercises with physical therapy. At 32 months post-operative, the patient was functioning well without the use of assistive devices. He had an active ROM of 0–90° (Fig. 9). An X-ray showed changes compared to previous studies (IS ratio 2) (Fig. 10 and 11).

This was a case of chronic patella alta with over 12 years between the time of initial injury and reconstructive surgery. The patient presented with this challenging condition due to proximal migration of the patella, quadriceps atrophy, and severe contracture. Primary repair of the extensor mechanism was impossible due to the long history of high riding patella. Seeking guidance from the published literature was extremely difficult due to limited reports of similar conditions.
The published literature divided about: (1) How to bring the patella down to its anatomical location, (2) repair the extensor mechanism using allograft versus autograft, and (3) fixation method. Table 1 presents published literature of similar patellar conditions.
Reduction of the patella to its normal station can be achieved acutely or with gradual distraction. While acute relocation of the patella into its anatomical position can be achieved with V-Y lengthening of quadriceps tendons [8], this option was not ideal for our patient. The quadriceps tendon was severely contracted with marked proximal migration of the patella, and such procedures can further weaken the quadriceps muscles and lead to more knee extensor lag. Gradual relocation was another alternative. Rocha et al. used a two-stage technique. The first-stage included transpatellar skeletal traction with 3 kg of traction and a gradual increase of 0.5 kg/day. The patient was admitted and closely monitored with X-rays until the patella reached its anatomical location. Extensor mechanism reconstruction was performed using autograft (Semitendinosus and Gracilis) [9]. Gradual distraction of patella to its anatomical location using an Ilizarov external fixator was used in our case. The use of an Ilizarov frame was effective in the distraction of the patella to anatomic position preoperatively [10, 11, 12]. The Ilizarov distraction provided several advantages in our patient: (1) Minimally invasive, (2) allowing weight-bearing as tolerated during the treatment course, (3) avoidance of the need for prolonged hospital admission compared to transpatellar skeletal traction, (4) the ability to control distraction, rate, rhythm, and the final destination of the patella, and (5) distraction histogenesis provided more tissues to make the second stage easier.
However, the use of an Ilizarov external fixator for patella distraction is not without limitations. Due to the size and weight of the hardware, mobilization can be limited in some patients, increasing the risk for DVT and/or PE, which happened to our patient [13]. Our patient’s unique social situation, being a prisoner, further limited his mobility and possibly contributed to the development of the PE in this case. While the patient’s pulmonary embolism was successfully treated with medical management, this does highlight the need for appropriate DVT prophylaxis during the distraction phase of these operations. We recommend this decision be based on individual patient characteristics, as most patients can mobilize appropriately and thus prevent thrombosis without the need for chemical prophylaxis.
Few published reports in the literature have discussed the application of an Ilizarov external fixator in patellar disorders, including patella alta, or patella Baja (infera), Table 1. Isiklar et al. reported that two patients with chronic rupture of the patellar tendon who were placed in an Ilizarov frame for 4–6 weeks to distract the patella at a rate of 1–2 mm/day [11]; however, their patients had significantly less time between initial injury and surgery than the case presented (8 months and 3.5 years vs. 12 years, respectively). Similarly, Harato et al. described the use of polyethylene tape for 12–24 h to achieve anatomic reduction of the patella in the setting of chronic patellar tendon ruptures without the added risk of complications from prolonged external fixation [7], though the length of time between injury and surgery was not mentioned. The increased time from initial injury seen in our patient contributed to the substantial amount of scar tissue and patella osteoporosis seen intraoperatively, which made one-stage distraction and primary repair impossible.
Gradual distraction using the Ilizarov frame is believed to metabolically activate tissue growth (histogenesis) by the law of tension stress [11]. This could allow the surrounding soft tissue to be more conducive to healing in the setting of chronic patellar tendon ruptures which are usually riddled with scar tissue.
One of the main predictors of successful reconstruction is the time between the initial injury and definitive fixation [3, 5, 7, 11]. In the case above, the 12 years between the initial injury and surgical fixation likely led to this patient’s extensive scar tissue formation and severe osteoporosis. Another important factor in recovery is adherence to a rehabilitation protocol focused on ROM exercises and quadriceps strengthening [6, 7]. Our patient’s status as a prisoner limited his ability to complete appropriate follow-up and physical therapy. In addition to the lack of therapy, we believe that the likely lack of movement contributed to the graft becoming stiff and weakening thus contributing to this patient’s subsequent graft failure. Some of the correction obtained initially was lost during the course of the treatment after the Ilizarov frame was removed; making the treatment by the external fixator is “partial success” rather than full correction of the deformity. It is a possibility that a longer time in the Ilizarov fixator was needed to avoid this partial recurrence. At present, there are no clear guidelines for the length of time a patient should be in the frame for this rare pathology [10, 11, 13].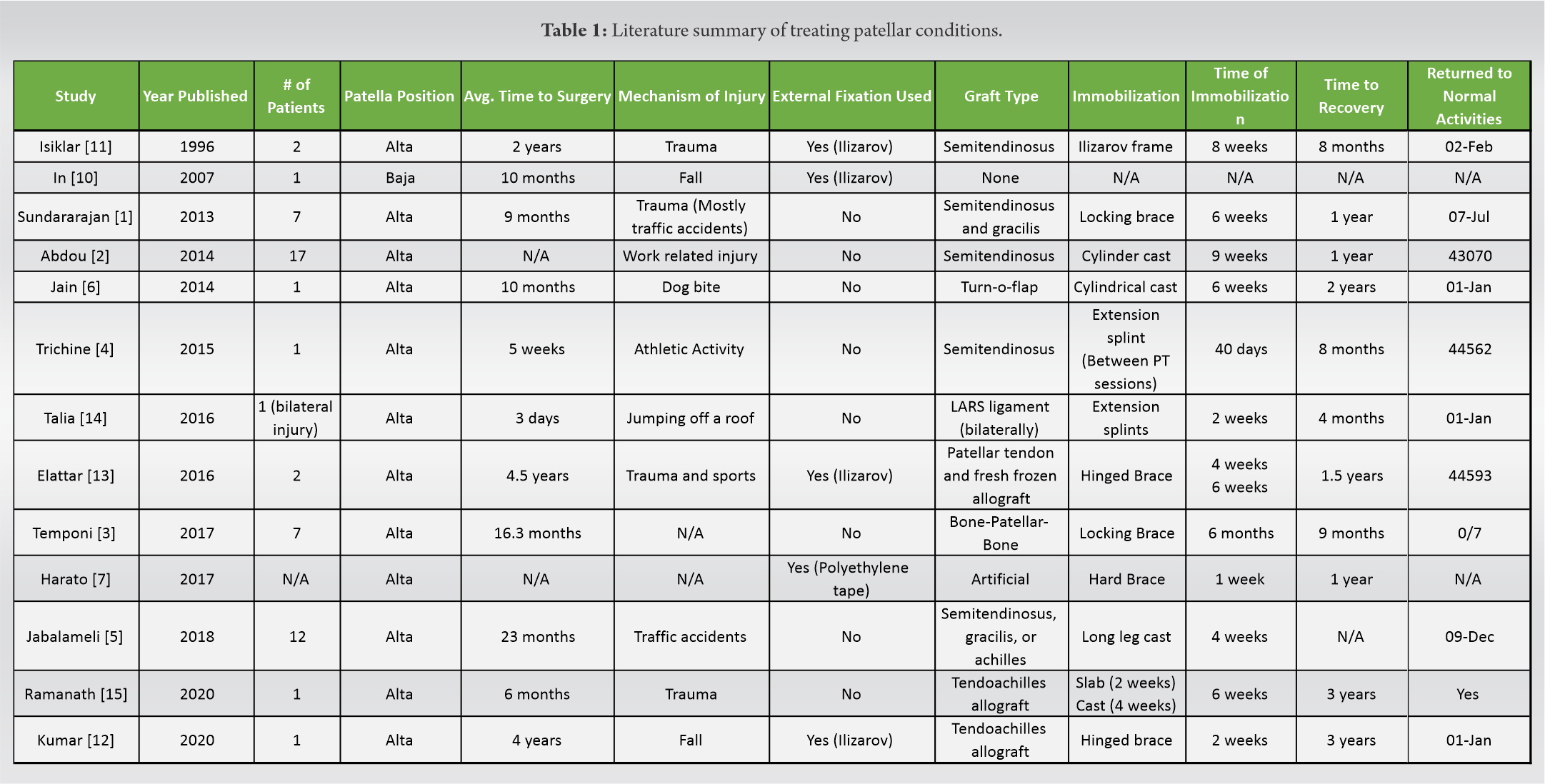
Chronic patella alta and patellar tendon rupture are a rare injury with no agreed-on treatment. This case demonstrated that an Ilizarov frame can be used to reduce the patella to anatomic position before reconstructive surgery. The Ilizarov fixator allows stretching of the extensive scar tissues without having to cut through the quadriceps muscle. The extended period of patella alta makes any reconstruction method subjected to high failure rate or inability to reach full correction. Complication of immobilization (DVT and PE) is a risk with this treatment technique. The duration of the frame application is still a debatable issue, with possibly some advantages to leave the frame for longer periods in the cases with long history of patella alta.
Patients with very long history of severe patella alta are a real challenging cases. Ilizarov gradual lengthening can correct the deformity without having to do any soft-tissue release. Partial correction (rather than full correction) may occur especially with very long period of pathology and in cases with patients are not very compliant.
References
- 1.Sundararajan SR, Srikanth KP, Rajasekaran S. Neglected patellar tendon ruptures: A simple modified reconstruction using hamstrings tendon graft. Int Orthop 2013;37:2159-64. [Google Scholar]
- 2.Abdou YE. Reconstruction of a chronic patellar tendon rupture with semitendinosus autograft. Arch Orthop Trauma Surg 2014;134:1717-21. [Google Scholar]
- 3.Temponi EF, Camelo N, Tuteja S, Thaunat M, Daggett M, Fayard JM, et al. Reconstruction of chronic patellar tendon rupture with contralateral bone-tendon-bone autograft. Knee Surg Sports Traumatol Arthrosc 2017;25:2468-73. [Google Scholar]
- 4.Ibrahim TF, Tarek B, Assia B, Mahdjoub B. Reconstruction of neglected ruptured patellar tendon using ipsilateral semitendinosus tendon and a turndown quadriceps tendon. Jacobs J Sports Med 2015;2:1-6. [Google Scholar]
- 5.Jabalameli M, Bagherifard A, Hadi H, Mohseni MM, Yoosefzadeh A, Ghaffari S. Surgical treatment of chronic patellar tendon rupture: A case series study. Trauma Monthly 2018;23:59259. [Google Scholar]
- 6.Jain S, Jain AK, Dhammi IK, Modi P. Neglected patellar tendon rupture treated by trans-osseous encirclage wire and turn-o-flap: Case report. J Orthop Case Rep 2014;4:5-8. [Google Scholar]
- 7.Harato K, Kobayashi S, Udagawa K, Iwama Y, Masumoto K, Enomoto H, et al. Surgical technique to bring down the patellar height and to reconstruct the tendon for chronic patellar tendon rupture. Arthrosc Tech 2017;6:e1897-901. [Google Scholar]
- 8.Lewis PB, Rue JP, Bach BR, Jr. Chronic patellar tendon rupture: Surgical reconstruction technique using 2 Achilles tendon allografts. J Knee Surg 2008;21:130-5. [Google Scholar]
- 9.Rocha de Faria JL, de Barros Carvalho M, Marques AC, et al. Surgical treatment for chronic rupture of the patellar tendon performed in 2 stages. Arthrosc Tech 2020;9:e159-66. [Google Scholar]
- 10.In Y, Kim SJ, Kwon YJ. Patellar tendon lengthening for patella infera using the Ilizarov technique. J Bone Joint Surg Br 2007;89:398-400. [Google Scholar]
- 11.Isiklar ZU, Varner KE, Lindsey RW, Bocell JR, Lintner DM. Late reconstruction of patellar ligament ruptures using Ilizarov external fixation. Clin Orthop Relat Res 1996;322:174-8. [Google Scholar]
- 12.Kumar A, Rutherford-Davies J, Thorpe P, Newson A. Combined quadriceps lengthening (using an external ring fixator) and patellar tendon reconstruction (using a tendoachilles allograft) in a case of chronic patellar tendon rupture: A case report. Knee 2020;27:598-606. [Google Scholar]
- 13.Elattar O, Coleman SH, Warren RF, Rozbruch SR. Neglected patellar tendon rupture with massive proximal patellar migration treated with patellar transport and staged allograft reconstruction: A report of 2 cases. Orthop J Sports Med 2016;4:???. [Google Scholar]
- 14.Talia AJ, Tran P. Bilateral patellar tendon reconstruction using LARS ligaments: Case report and review of the literature. BMC Musculoskelet Disord 2016;17:302. [Google Scholar]
- 15.Ramanath SK, Shah RH, Patil S, Umesh S. Reconstruction of neglected patellar tendon rupture using tendoachilles’ allograft with transosseous tunnels: A case report. J Orthop Case Rep 2020;10:27-9. [Google Scholar]








