Long Locking locking plate fixation is effective method of treatment for long oblique diaphyseal peri-implant fractures in femur following proximal femur nail.
Dr. Tushar C Patil, Junior Resident, Department of Orthopaedics, Grant Government Medical College, Mumbai, Maharashtra. India. E-mail: tushar6919@gmail.com
Introduction:The rising demographic trend towards elderly population and increased incidence of osteosynthesis of proximal femur fractures are associated with increased recurrent falls and rise in incidence of peri- implant fractures.
Case Report: Here, we present a difficult case of a peri- implant femur shaft fracture in a 55-year-old male, with stuck short proximal femur nail (PFN) removal followed by long distal femur plating with bone grafting showing good fracture union at 1 year with satisfactory functional outcome.
Conclusion:Peri- implant femur fractures are quite rare and more commonly occur in elderly. Among all treatment modalities for intertrochanteric femur fracture fixation, the literature shows short PFN having highest comparative risk for peri peri-implant fractures. Implant removal followed by locking plates for long spiral fractures provides a stable, anatomical, and reliable fixation. Bone grafting augments bony union, especially in cases of bone defects.
Keywords: Peri-implant, femur, fracture, proximal femur nail, distal femur locking plate.
The rising demographic trend toward elderly population and increased incidence of osteosynthesis of proximal femur fractures are associated with increased recurrent falls and rise in incidence of peri-implant fractures [1]. The incidence of peri-implant fractures in operated cases of intertrochanteric femur fractures is found to be highest in short proximal femoral nail (PFN), that is, PFN (18.74 fractures/1000 person years), followed by cementless hemiarthroplasty (11.72 fractures/1000 person years), followed by primary arthroplasty with cement (6.2 fractures/1000 person years), and was quite lower in dynamic hip screw or cannulated hip screw patients (4.50 fractures/1000 person years) [2]. Peri-implant fractures in operated case of short PFN are predisposed by osteoporosis, old age, long-term bisphosphonates intake, and trivial falls [3]. According to Koch’s model, the forces are distributed along femur length from highly tensile subtrochanteric region to becoming compressive at distal lateral metaphysis. Hence, operated cases of short PFN are predisposed to increased stress at distal locking sites. An alternative solution is avoiding distal screw placement [3]. If retention of previous implant is decided, then overlapping of the new implant is desired as it increases failure strength and decreases regional strain. As in gapped instrumentation, the distal tip of proximal and proximal tip of distal implant act as stress risers in intervening area, leading to failure of construct [4]. In stable constructs, the main goal is retention of implant if possible, with precontoured periarticular locking plates with polyaxial screws as preferred second implant especially in osteoporotic fractures [5].
A 55-year-old male patient brought to our OPD with alleged history of slip and fall at home with trauma to the left thigh 1 day back. There was no other associated injury. The patient got operated for the left short PFN 6 years back and for the right long femur nail with encerclage in 3 years back as seen on X-rays in (Fig. 1).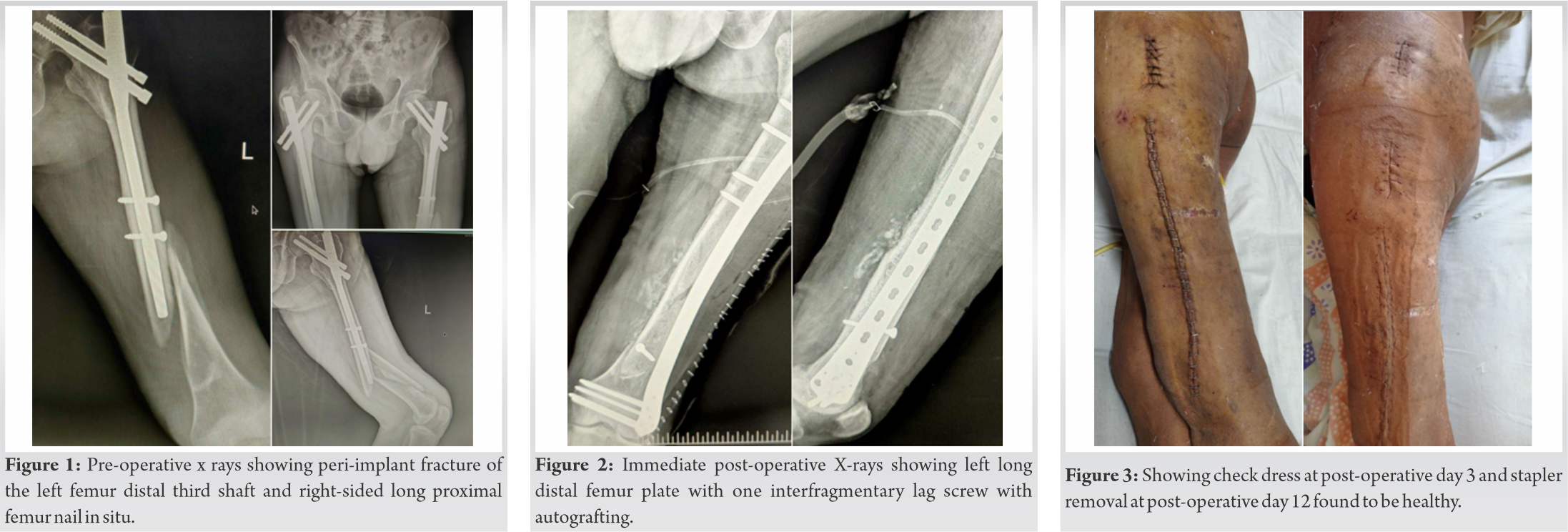
He was a known case of seizure disorder, on medications. Local examination revealed local pain and tenderness over mid-thigh with swelling and contusion. The range of motion was restricted at both hip and knee without any distal neurovascular deficit. Plain radiographs revealed peri-implant fracture of the left femur distal third shaft, as seen in (Fig. 1). The patient was then planned for implant removal followed by long distal femur periarticular plating. The patient was taken on operating table in supine position under all aseptic precautions and under epidural plus spinal anesthesia. Scrubbing, painting, and draping done. Incision taken over previous surgical scar for distal locking site of short PFN. Distal locking screw removed followed similarly for proximal locking screws. Incision taken over entry site and entry site cleared of soft tissue, nail tip identified. Nail removal set attached and nail safely removed without any complications.
Incision for distal locking site extended distally till lateral knee joint. Subcutaneous fat cleared and tensor fascia lata incised, and vastus lateralis divided.
Fracture reduced with traction and reduction holded with reduction clamps. A precontoured 13 hole 5 mm left distal femur locking plate selected and fixed on femur with preliminary k-wires. Reduction checked and confirmed under fluoroscopy. 4.5 mm lag screw was placed first for compression of anterior wedge fragment. Distal metaphyseal 5 mm locking cancellous is placed occupying 75% of locking holes. Followed by 4.5 mm locking screws proximally. Corticocancellous allogenic bone graft harvested from ipsilateral iliac crest is placed in the palpable defects medially. Above knee slab was given in immediate post-operative period which replaced by long rigid knee brace after suture removal for 3 weeks. Immediate post-operative X-rays are shown in (Fig. 2). The patient was mobilized with toe touch weight-bearing walk using walker. Passive assisted knee range on motion exercises was started after 3 weeks followed by active knee range of motion started at 6 weeks and quadriceps strengthening exercises after 12 weeks postoperatively. Check dress done post-operative day 3 and 7 was found to be healthy. Suture removal done on post-operative day 12, as seen in (Fig. 3). X-rays at 1 year post-operative shows good bony union, as seen in (Fig. 4). The patient was able to walk full weight-bearing without any walking aids at 6 months follow-up with good range of motion at hip and knee, as seen in (Fig. 5). There was good union and remodeling at 1 year follow-up.
Pre-operative oxford knee score was 14. Post-operative oxford knee score at 1 year follow-up is 36.
Short femoral nails are cost-effective modality of treating intertrochanteric femur fractures with shorter operating time and little blood loss. However, they are also historically associated with greater risk of peri-implant fractures [6]. Age of the patient, bone quality, soft-tissue status, fracture morphology, and functional demands of patient are taken into account before deciding modality of surgical management [7]. Peri-implant fractures around the tip of nail as well as diaphyseal fracture risk and anterior cortical penetration are well known risk factors of short PFN [8]. The wedging in the anterior cortex could be result of tip causing additional displacement of anterior cortex. Union and stability at diaphyseal fracture site is threatened by strong deforming muscle forces [4]. The anticonvulsive therapy in seizure disorder is known to cause osteopenia; hence, weaker bones in previously operated patient results in more comminution in peri-implant fractures following trivial falls. Chan et al. define non prosthetic peri-implant fracture as a fracture in a bone with an existing non-prosthetic implant such as an intramedullary or extramedullary plate or screws. They have classified these peri-implant fractures according to type of implant (plate or nail), position of fracture relative to implant (1- at the tip, 2-distant to implant), and healing status of previous fracture (A – healed, B – not healed, and C – failing). Our patient had N1A fracture [9]. First generation Gamma nail showed peri-implant fracture rates of 17%. Newer improved designs show decreased fracture rates of 0.3–1% for dynamic hip screw and slightly more of 0.7–3.5% in cephalomedullary nails [9]. In management of peri-implant fractures, if implant is removed then areas of potential weakness and bone defects must be bridged if necessary. Areas of high stress risers must be avoided. There are higher complication rates in settings of revision surgeries through previous surgery scar mark and extensive soft-tissue dissection and periosteal stripping. Disuse osteopenia and loss of bone stock further complicate the situation [9]. Peri-implant femur fractures are most commonly spiral shaped with fracture line directed toward distal tip of previous implant. Hence, specifically for distal diaphyseal and metaphyseal fractures after short PFN, long exchange nailing should be avoided as such fractures, which would be insufficiently stabilized. The working length in distal femur may not be sufficient for rigid fixation with intramedullary nailing and subsequent delayed union or nonunion might be outcome when intramedullary nailing option is chosen. Long locking plates are considered to provide relatively stable fixation for achieving union by secondary healing in metaphyseo-diaphyseal region of distal femur. Periarticular locking plates give better results than dynamic condylar screw or supracondylar nail, which has been shown in biomechanical studies of peri-implant distal femur fractures [1, 4]. Conservative non-operative management leads to increased complication rates and mortality by 2–3 times [4]. Stiffness and loss of functions along with bony deformation may result in non-operative treatment. Autologous bone grafting remains the gold standard for treating fracture defects and non-unions. Its combination of biological and mechanical properties such as osteogenecity, osteoconductivity, and osteoinductivity ensures better bony union. It leads to filling of fracture defects and accelerates bone healing [10].
Peri-implant femur fractures are quite rare and more commonly occur in elderly. Among all treatment modalities for intertrochanteric femur fracture fixation, the literature shows short PFN having highest comparative risk for peri-implant fractures. Implant removal followed by locking plates for long spiral fractures provides a stable, anatomical, and reliable fixation. Bone grafting augments bony union, especially in cases of bone defects.
Peri-implant long comminuted fracture in distal third of femur shaft following stuck PFN can be very well treated with secondary healing offered with relative stability by long locking plate fixation after attempting PFN removal.
References
- 1.Müller F, Galler M, Zellner M, Bäuml C, Marzouk A, Füchtmeier B. Peri-implant femoral fractures: The risk is more than three times higher within PFN compared with DHS. Injury 2016;47:2189-94. [Google Scholar]
- 2.Robinson CM, Adams CI, Craig M, Doward W, Clarke MC, Auld J. Implant-related fractures of the femur following hip fracture surgery. JBJS 2002;84:1116-22. [Google Scholar]
- 3.Yamamoto N, Dan’ura T, Noda T, Ozaki T. Non-traumatic atypical peri-implant femoral fracture at the distal screw after short femoral nail fixation for a pertrochanteric fracture. Acta Med Okayama 2020;74:151-7. [Google Scholar]
- 4.Mounasamy V, Tran K, Baer G, Brown TE. Novel fixation of a peri-implant femur fracture in the elderly. Injury Extra 2007;38:231-4. [Google Scholar]
- 5.Ruchholtz S, El-Zayat B, Kreslo D, Bücking B, Lewan U, Krüger A, et al. Less invasive polyaxial locking plate fixation in periprosthetic and peri-implant fractures of the femura prospective study of 41 patients. Injury 2013;44:239-48. [Google Scholar]
- 6.Goodnough LH, Salazar BP, Furness J, Feng JE, DeBaun MR, Campbell ST, et al. How are peri-implant fractures below short versus long cephalomedullary nails different? Eur J Orthop Surg Traumatol 2021;31:421-7. [Google Scholar]
- 7.Kawoosa AA, Dhar SA, Butt MF, Dar GN, Mir MR. The role of composite technique in managing peri implant re-fractures in a case with supracondylar fracture of the femur: A case report. Cases J 2009;2:1-4. [Google Scholar]
- 8.Breceda A, Sands A, Zderic I, Schopper C, Schader J, Gehweiler D, et al. Biomechanical analysis of peri-implant fractures in short versus long cephalomedullary implants following pertrochanteric fracture consolidation. Injury 2021;52:60-5. [Google Scholar]
- 9.Chan LW, Gardner AW, Wong MK, Chua K, Kwek EB. Singapore orthopaedic research collaborative (SORCE). Non-prosthetic peri-implant fractures: Classification, management and outcomes. Arch Orthop Trauma Surg 2018;138:791-802. [Google Scholar]
- 10.Pape HC, Evans A, Kobbe P. Autologous bone graft: Properties and techniques. J Orthop Trauma 2010;24:36-40. [Google Scholar]










