Obturator internus bursitis is a possible cause of groin pain not responding to conservative line of management and MRI is the key to diagnosis.
Dr. Vaibhav Bagaria, Department of Orthopaedic Surgery, Sir H. N. Reliance Foundation Hospital, Mumbai, Maharashtra, India. E-mail: drbagaria@gmail.com
Introduction: Traumatic groin pain (GP) is frequently the result of acute trauma, often an indirect muscle injury. The most affected muscles in traumatic GP are the rectus abdominis, adductors, and iliopsoas. The obturator internus bursitis as a cause of GP is very rare.
Case Presentation:The present case describes a rare indirect injury of obturator internus bursitis in a 22-year-old male football player who reported GP that used to worsen with sprinting and change in directions. The pain was relieved with rest and sprinting at 80% capacity. The patient had been diagnosed clinically and on magnetic resonance imaging (MRI) as a case of obturator internus insertional tendinopathy with bursitis. His symptoms resolved after ultrasound-guided injection in the inflamed tendon sheath at its insertion point. After 2 years, the patient was followed up with a triumphant return to professional football with no recurrence and a good prognosis in a relatively short recovery time.
Conclusion: Clinical diagnosis of obturator injuries is often tricky. GP not responding to conservative management presents a unique challenge to the physician and the rehabilitation team. MRI must follow the radiological investigations and ultrasound if the reports were inconclusive of the diagnosis. In the present case study, the usual causes of such pain (osteitis pubis, and adductor muscle strains/tendinosis) were ruled out, and a specific unique condition was diagnosed with the help of the MRI.
Keywords: Bursitis, groin pain, magnetic resonance imaging, obturator internus.
Groin pain (GP) is a common and broad cause of disability both in professional and amateur’s athletes and is relatively an occurring phenomenon in sports that requires quick accelerations, changes in direction, and kicking [1]. In a soccer team, 21% of players experienced GP during each season [2]. GP as proposed by the “GP Italian Consensus Conference on Terminology, the Clinical Evaluation and Imaging Assessment in GP in Athletics” [3] can be defined as “Any clinical symptom reported by the patient, located at the inguinal-pubic adductor area, affecting sports activities, or interfering with activities of daily living and requiring medical attention.” GP is divided into three main categories. The first category is represented by the GP of traumatic origin, in which the onset of pain is due to any acute trauma, and this clinical diagnosis is supported by medical history, clinical examination, and imaging. The second category includes GP due to functional overload, characterized by insidious, and progressive onset, without an acute trauma or a situation to which the onset of pain symptoms can be attributed with certainty. The third category is represented by the long-standing GP or chronic GP, in which the cohort of symptoms reported by the patient continues for an extended period (over 12 weeks) and is recalcitrant to any conservative therapy. Traumatic GP is generally the consequence of an acute indirect muscle-tendon injury. In traumatic GP, the most affected muscle groups are rectus abdominis, adductors, and iliopsoas muscles [3]. GP contributes to loss of playtime in most footballers. The Doha agreement [1] broadly described the GP origin under
• Adductor-related, iliopsoas-related, inguinal-related, and pubic-related GP
• Hip related GP
• Others: unclassified.
The present case study of an obturator internus tendinosis is an unusual cause of GP in football players. To the best of our knowledge, there were only seven studies concerning a cause of GP in obturator internus [2] injuries in the literature review [4, 5, 6, 7, 8. 9, 10].
A 22-year-old professional football player had reported to outpatient department complaining of recurring left GP that had been going on for last few months. A detailed clinical examination by a senior specialist was performed. His findings noted that patient was athletically built with a normal alignment of the lower limbs when standing. The hip joint range of motion (ROM) was normal, labrum and strength of muscles were normal except that there was localized tenderness in the posteromedial aspect of the hip, where the tendon of the obturator internus passes in between the ischial spine and ischial tuberosity. The pain was referred to the anterior aspect of the thigh and groin. Passive adduction and internal rotation produced minimal pain and discomfort. Resisted left hip flexion and external rotation in 90°’ flexion on manual muscle tests were weak compared to the right side with pain felt deep in the left groin. Jumping and landing with a twist could create momentary sharp pain of tolerable nature that eases with repetition on the left side.
A clinical diagnosis of dynamic ischiofemoral impingement was made with or without labral involvement, with potential differential diagnosis of profound hip stabilizers weakness. Due to the inability to reproduce symptoms in a controlled clinical setting and chronic alongside the recurring nature of his symptoms with sports-specific activity triggers, the patient was referred for radiological assessment. The X-ray revealed no evidence of impingement or rotational mal-alignment. In view of the chronic and recurring nature of pain, further investigation in form of magnetic resonance imaging (MRI) was done. MRI (Fig. 1) showed an intensity of the liquid signal localized in the gluteofemoral bursa and the obturator bursa with interruption of a few fibers of the obturator internus. Fluid flows along the obturator internus tendon without muscle atrophy. (Fig. 2) shows the location of the obturator internus of the bursa and the orientation of the fibers. based on the classification proposed by the Italian Consensus on the Conservative Treatment of Lower Limb Muscle Damage in Athletes. 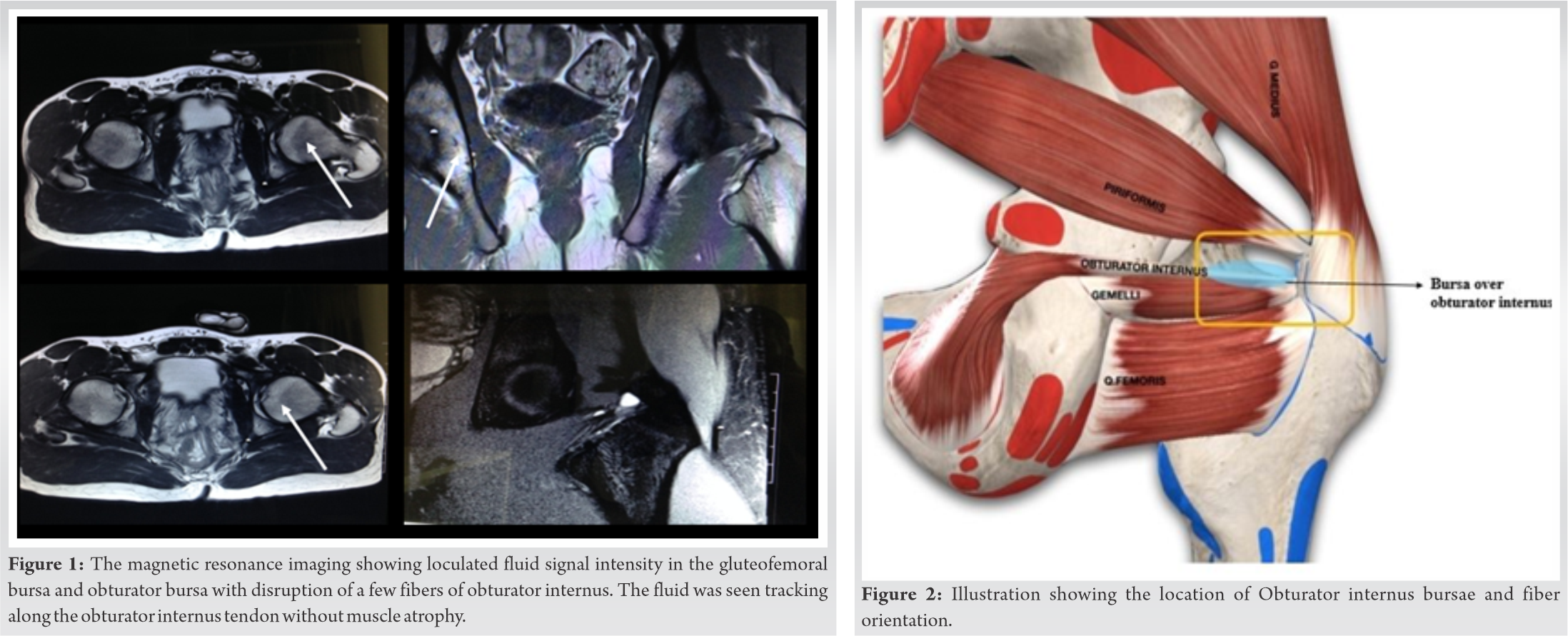
The patient was assigned to a rehabilitation program that included four phases – mentioned in section outcome and follow-up. After 6 weeks of structured rehabilitation program, the problem remains un resolved. The pain would subside with rest and by avoiding sprinting and sudden change of direction, massages, and stretching exercises. However, the symptoms would recur on training and playing and this continued despite many rehabilitation and physical therapy sessions. The most recent pain episode started after the player got trailed for a professional contract and was required to train for more than 4 h a day and play regularly. Based on MRI findings and in view of failure of conservative management, diagnostic and therapeutic ultrasound-guided injection into the posterior intra-trochanteric space was planned. After informed consent, ultrasound-guided injection of local anesthetic and methylprednisolone acetate 2 ml (80 mg: 40 mg/ml) in the sheath of the obturator internus tendon was given. The patient was advised to rest 3 days and assigned to a rehabilitation path that included four phases briefed.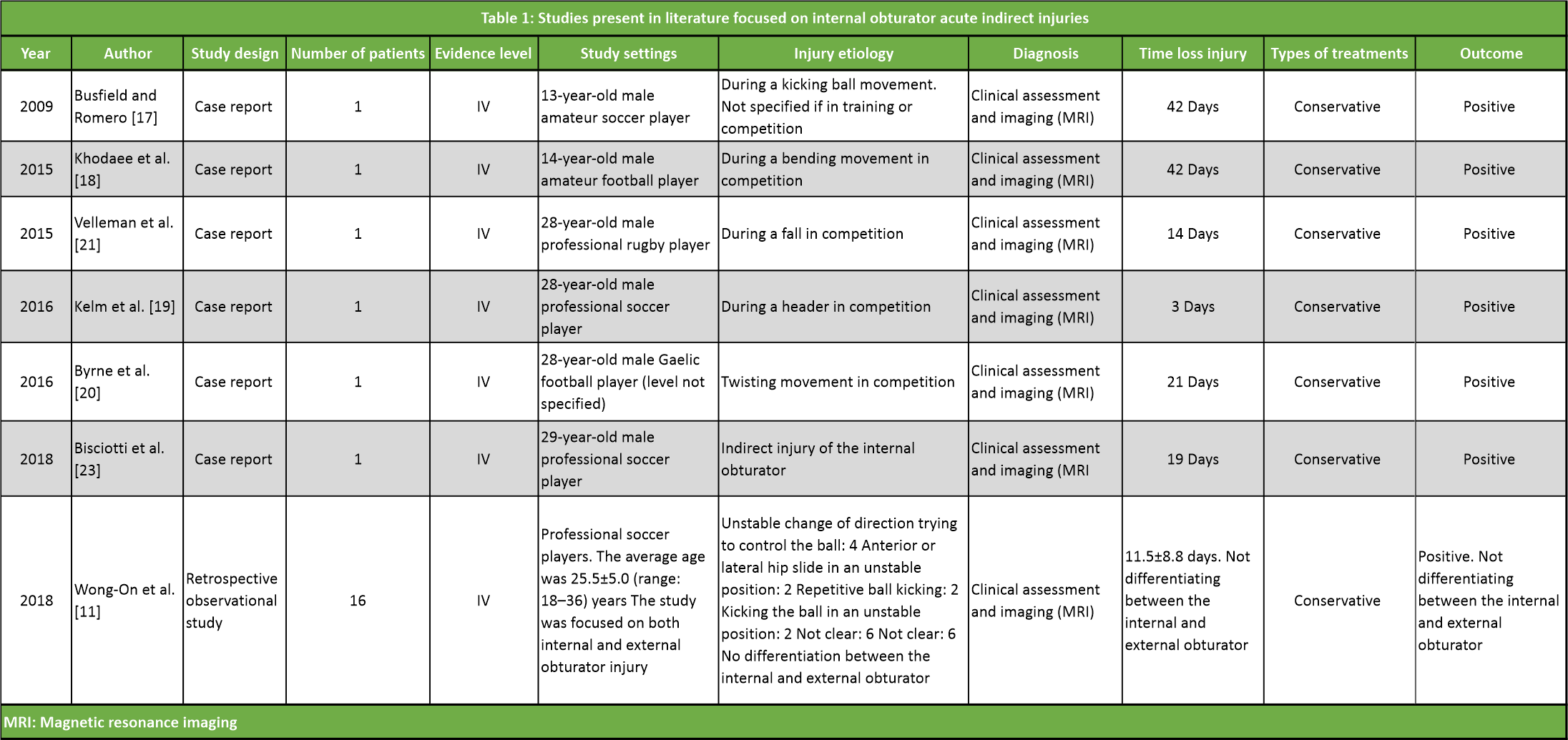
In the first phase, (after 5 days) the focus was on controlling pain and mobilizing. The patient became completely asymptomatic after 3 days of rest. Passive hip adduction and internal rotation against resistance were pain-free. The patient was then subjected to phased rehabilitation. A clinical assessment and imaging examination were used to determine the transition between Phases I and II (after 7 days). As clinical criteria, we adopted the absence of pain during maximal isometric contractions, the absence of pain during passive stretching and active stretching tests, and the fact that the hip joint had reached its full ROM. Non-impact hip and lower limb strengthening regimes focusing on low resistance and hip muscle group endurance exercises. Left side hip stability with static and dynamic exercises. The transition criteria between Phases II and III were still based on the clinical assessment and the imaging examination (after 14 days). The clinical criteria used were no pain during maximal concentric and submaximal eccentric contractions. The imaging criteria adopted were the disappearance of the lesion gap and compact granulation repair tissue within the lesion gap in MRI examination. Lower body strengthening and conditioning exercises with dynamic loading exercises and football specific skill drills were introduced. Resume kicking and shooting with 50–75% effort and ball-handling drills and moderate sprint speed changes of direction drills. At the end of the week, the patient achieved 90% strength and endurance for regular fitness. The transition criteria between Phases III and IV were based on the clinical assessment and the imaging examination (after 21 days). During the last phase, eccentric exercises with progressively increased intensity, run with cutting movements at progressive speed, and football individual technique exercises were introduced. At the same time, a progressive integration with the team was introduced in this phase. The patient resumed normal strength and endurance training as per his schedule with football training, including high sprint running with the change of direction and cutting and ball tackling skills with a local professional team. Before the professional could test out, the patient had been trained for more than 4 h a day for 3 weeks. The athlete was followed up for 2 years, and no recurrence was reported.
Evaluating the GP in an athlete can be challenging to the treating physician as the pain may not be well localized. The patients usually present with overlapping symptoms or over-use and the possibility of coexisting injuries cannot be ruled out. The complex anatomy of the pubic symphysis and rami further confounds the clinical judgments due to the proximity of the muscles and tendons in this region. This leads to delay in the diagnosis and can potentially have adverse consequences on the playing time resulting in premature career termination. GP resistance to conservative management presents a unique challenge to the treating physician and the rehabilitation team. MRI must follow the radiological investigations and ultrasound if the reports were inconclusive of the diagnosis. In this particular case, the usual causes of such pain (osteitis pubis, adductor muscle strains/tendinosis, and ETC) were ruled out, and a specific unique condition was diagnosed with the help of an MRI. A short external rotator of the hip rotates the femur externally and is required to maintain the stability of the femoral head within the acetabulum throughout the ROM of the hip joint. It is functionally similar to the rotator cuff of the shoulder joint [3]. These muscles had a complex origin and sat deep in the pelvis, making them difficult to isolate during a clinical examination. The obturator internus anatomically is a triangular part of the externally rotating muscles of the hip. The obturator foramen arises from the inner surface of the obturator membrane and the surrounding bony margins. Its muscle bands converge backwards, then pass the ischial foramen to become extra-pelvic, and give rise to an advancing tendon. Finally, the obturator internus enters the medial surface of the greater trochanter anteriorly and above the trochanteric fossa. At its distal insertion, the obturator internus fuses with the tendon of the twin muscles (triceps coxae), forming a common tendon [11]. This anatomical association with the twin tendon may explain the inferior lesions presented by the obturator internus compared to the obturator externus muscle [4]. The additional internal obturator rotates the thigh, removing it when the hip and leg were flexed, stabilizing the hip joint. It was innervated by the obturator nerve (L5 and S2), and its vascularization depends on the obturator artery. The maximum force of the obturator internus depended on the degree of flexion of the hip joint and was most significant at the start of the swing phase during the running stride [12]. In addition to the obturator internus, the other muscles that act as the external rotators of the hip are the piriformis, obturator externa, twins, and the quadrate of the femur. These muscles were collectively called “short lateral or external rotators.” [13] This muscle group has an essential stabilizing action in the hip joint, stabilizing the femoral head in the acetabulum during hip movements [11]. Despite the critical work done by this muscle group, little was found in the literature. The obturator internus originated from the rami surrounding the obturator foramen and the quadrilateral plate and left the pelvis through the lesser sciatic foramen and the notch before inserting on the greater trochanter of the femur [12]. It was separated from the grooved surface of the ischium by the obturator bursa. The MRI features of this bursa were reported identical by Hwang et al. 2008 [14] (Fig. 2).
Hodges et al., in 2014, reported that the obturator internus was electromyographically active during hip extension, external rotation, and abduction [15]. Lateral hip rotators were essential for hip control: The shorter mean fiber length, small fiber pennation angles, small physiological cross-sectional areas, and high proportion of slow-twitch fibers make them essential for hip joint stabilization [16]. The obturator internus supports the hip joint only when the torques were applied in a specific direction. It maintains the external rotation moment arms throughout hip flexion, which decreased with an increased inflexion. There were few reported case studies of these muscle injuries and this cause is considered to be extremely rare in the sporting population [4]. Wong et al. reported two different injury mechanisms; first, the unstable position of the pelvis associated with an increase in load on the affected hip that may lead to an injury of the obturator muscles in the weight-bearing hip. (e.g., kicking the football in an unstable position). Moreover, second, the repetitive loading of the extremity while kicking the ball can injure either be the kicking extremity or the pivoting one [17]. During a sudden change of direction, the injury can occur in an unstable position to either obturator internus or obturator externus. The severity of the injury depends on the degree of the flexion or extension of the hip. Clinical diagnosis of obturator injuries was often tricky. Due to recall bias, additional investigations in the form of an MRI may help reach an accurate diagnosis. Insidious onset, manageable symptoms that affect specific activities and the ability to train and play with trick modifications, and the location of the symptoms reported by the athlete present a diagnostic challenge due to different pathologies around the hip, especially the adductor-related GP. Chronicity of symptoms adds to the diagnostic challenge. Due to the lack of effort to determine the exact cause of recurrent symptoms, the clinician was often misled by the rare nature of these injuries. In this case, the ultrasound-guided injection was used for diagnostic and therapeutic intervention as the symptoms never cleared up despite three years of focused conservative approaches. Smith et al. found that ultrasound-guided injections to the obturator internus muscle and bursa are feasible and can effectively target the structure without injuring other structures in the region. Ultrasound by a skilled expert helps understand the nature of the injury, which establishes working assessment dynamically with athletes involved in sports that require sudden acceleration and deceleration [11]. The previous literature mainly describes chronic syndromes such as piriformis syndrome or ischialfemoral impingent [18], and only a few studies were based on acute lesions. In particular, only six studies have investigated acute indirect injury, of which five are case reports and one was a retrospective observational study [11]. A summary of the studies is presented in (Table 1). All case reports focus on acute indirect obturator internus injuries as follows: The first case report [5] describes indirect obturator internus injury in one patient. A 13-year-old amateur football player finished second to a young American footballer, a professional footballer finished third, a 28-year-old Gaelic football player placed fourth, and a 28-year-old male professional rugby player placed fifth [6, 7, 8, 9]. The retrospective observational study reports injury data recorded during four seasons in the Spanish professional football league (La Liga). During the period considered, lesions of the obturator externus were recorded [13], while lesions of the obturator internus were only reported in [4]. The main mechanisms that determine the traumatic lesion of the obturator internals were essentially three in number. The first was a pelvic position with a sudden change in the distribution of body weight [4, 19]; the second was a sudden change in direction in a condition of pelvic instability [4, 19]; and, finally, the third, which represents the etiopathogenetic situation described in this study, was represented by a sudden internal rotation of the hip with the hip and knee flexed to approximately 90° [20]. The fact that internal obturator recurrences had not been described in the literature [4] confirms the hypothesis that they depend on a well-defined mechanical situation, such as those described above, and were independent of intrinsic factors predisposing such as excessive retraction or stiffness of the inner flap. The case presented in this study shows, in line with other studies, that obturator internus lesions had a good prognosis and a relatively short recovery time [4, 8].
Obturator internus bursitis is a rare cause of the GP originating from external rotator muscle groups of the hip, which has shown to suffer a very low incidence of injury. Despite their low incidence, they should be considered in the event of a traumatic picture of the GP. The etiopathogenesis of the obturator internus bursitis lesion was linked to well-defined mechanical situations and seemed independent of intrinsic factors. In all cases reported so far, obturator internal bursitis lesions had a good prognosis and relatively short healing times. The present case report highlighted the importance of detailed history, imaging, clinical diagnostics, and therapeutic decision-making to provide appropriate treatment with a quick return to play. The rarity of the pathology required a meticulous clinical examination might cause the delay in diagnosis and result in either worsening the pathology or cost a preterm exit from the professional career. In this case, the patient was followed up after 2 years with a triumphant return to professional football with no recurrence.
GP resistance to conservative management presents a unique challenge to the treating physician and the rehabilitation team. Obturator bursitis is a rare cause of resistant GP, and the MRI is the key to diagnosis. Recalcitrant GP secondary to this condition warrants an ultrasound-guided steroid injection and a structured post-intervention rehabilitation Protocol.
References
- 1.Weir A, Brukner P, Delahunt E, Ekstrand J, Griffin D, Khan KM, et al. Doha agreement meeting on terminology and definitions in groin pain in athletes. Br J Sports Med 2015;49:768-74. [Google Scholar]
- 2.Hureibi KA, McLatchie GR. Groin pain in athletes. Scott Med J 2010;55:8-11. [Google Scholar]
- 3.O’Brien SD, Bui-Mansfield LT. MRI of quadratus femoris muscle tear: Another cause of hip pain. AJR Am J Roentgenol 2007;189:1185-9. [Google Scholar]
- 4.Wong-On M, Turmo-Garuz A, Arriaza R, de Suso JM, Til-Perez L, Yanguas-Leite X, et al. Injuries of the obturator muscles in professional soccer players. Knee Surg Sports Traumatol Arthrosc 2018;26:1936-42. [Google Scholar]
- 5.Busfield BT, Romero DM. Obturator internus strain in the hip of an adolescent athlete. Am J Orthop 2009;38:588-9. [Google Scholar]
- 6.Khodaee M, Jones D, Spittler J. Obturator internus and obturator externus strain in a high school quarterback. Asian J Sports Med 2015;6:e23481. [Google Scholar]
- 7.Kelm J, Ludwig O, Schneider G, Hopp S. Injury of the obturator internus muscle-a rare differential diagnosis in a soccer player (in Geran). Sportverletz Sportschaden 2016;30:50-3. [Google Scholar]
- 8.Byrne C, Alkhayat A, O’Neill P, Eustace S, Kavanagh E. Obturator internus muscle strains. Radiol Case Rep 2016;12:130-2. [Google Scholar]
- 9.Velleman MD, Jansen Van Rensburg A, Janse Van Rensburg DC, Strauss O. Acute obturator internus muscle strain in a rugby player: A case report. J Sports Med Phys Fitness 2015;55:1544-6. [Google Scholar]
- 10.Bisciotti GN, Corsini A, Cena E, Bisciotti AN, Bisciotti AL, Belli A, et al. Acute groin pain syndrome due to internal obturator muscle injury in a professional football player. Joints 2019;7:205-8. [Google Scholar]
- 11.Smith J, Wisniewski SJ, Wempe MK, Landry BW, Sellon JL. Sonographically guided obturator internus injections: Techniques and validation. J Ultrasound Med 2012;31:1597-608. [Google Scholar]
- 12.Solomon LB, Lee YC, Callary SA, Beck M, Howie DW. Anatomy of the piriformis, obturator internus and obturator externus: Implications for the posterior surgical approach to the hip. J Bone Joint Surg Br 2010;92:1317-24. [Google Scholar]
- 13.Gudena R, Alzahrani A, Railton P, Powell J, Ganz R. The anatomy and function of the obturator externus. Hip Int 2015;25:424-7. [Google Scholar]
- 14.Hwang JY, Lee SW, Kim JO. MR imaging features of obturator internus bursa of the hip. Korean J Radiol 2008;9:375-8. [Google Scholar]
- 15.Hodges PW, McLean L, Hodder J. Insight into the function of the obturator internus muscle in humans: Observations with development and validation of an electromyography recording technique. J Electromyogr Kinesiol 2014;24:489-96. [Google Scholar]
- 16.Roche JJ, Jones CD, Khan RJ, Yates PJ. The surgical anatomy of the piriformis tendon, with particular reference to total hip replacement: A cadaver study. Bone Joint J 2013;95:764-9. [Google Scholar]
- 17.Wong S, Ning A, Lee C, Feeley BT. Return to sport after muscle injury. Curr Rev Musculoskelet Med 2015;8:168-75. [Google Scholar]
- 18.Meknas K, Kartus J, Letto JI, Christensen A, Johansen O. Surgical release of the internal obturator tendon for the treatment of retro-trochanteric pain syndrome: A prospective randomized study, with long-term follow-up. Knee Surg Sports Traumatol Arthrosc 2009;17:1249-56. [Google Scholar]
- 19.Cass SP. Piriformis syndrome: A cause of nondiscogenic sciatica. Curr Sports Med Rep 2015;14:41-4. [Google Scholar]
- 20.Delp SL, Hess WE, Hungerford DS, Jones LC. Variation of rotation moment arms with hip flexion. J Biomech 1999;32:493-501. [Google Scholar]









