Osteochondroma, if not excised properly can recur involving the neurovascular bundle, and thus, its proper excision becomes very crucial.
Dr. Shivam Mehra, Department of Orthopaedics, Padmashree Dr. D.Y. Patil School of Medicine, Navi Mumbai - 400 706, Maharashtra, India. E-mail: drshivammehra@gmail.com
Introduction:Osteochondromas (OCEs) are benign chondrogenic lesions arising on the external surface of the bone with aberrant cartilage (exostosis) from the perichondral ring that may contain a marrow cavity also. In few cases, depending on the anatomical site affected, different degrees of edema, redness, paresthesia, or paresis can take place due to simple contact or friction. Furthermore, depending on their closeness to neurovascular structures, the procedure of excision becomes crucial to avoid recurrence. We report a unique case of recurrent OCE of the proximal humerus enclosing the brachial artery which makes for an important case and procedure to ensure that no relapse occurs.
Case Report:We report a unique case of a 13-year-old female who had presented with a history of pain and recurrent swelling for 5 years. The swelling size was 4.4 cm × 3.7 cm × 4 cm with a previous history of swelling at the same site operated in 2018.
Conclusion:This case report demonstrates that when presented with a case of recurrent OCE of the proximal humerus, doing proper excision of the tumor is crucial to prevent its relapse.
Keywords:Recurrent osteochondroma, proximal humerus, brachial artery.
Osteochondromas (OCEs) are the most common benign tumors arising on the external surface of the bone with aberrant cartilage [1, 2, 3]. OCEs account for 20–50% of benign bone tumors and 9% of all bone tumors [1, 2, 3]. Most of these tumors (85%) are solitary and nonhereditary in nature, while approximately 15% of these tumors are hereditary multiple OCEs [1, 2, 3]. Diagnosis of OCE involves presence of a capped cartilage and cortical and medullary continuity with the parent bone [3, 4]. Many of the patients are asymptomatic, though pain can be a clinical feature due to neural irritation, bursitis, mechanical irritation, fractures, osseous deformities, and malignant changes [3, 5]. There are unique challenges in diagnosis and treatment of OCEs of the proximal humerus. One can be predisposed to tendinitis, tendon ruptures, limitations of shoulder motion, and neurovascular compression depending on their proximity to important structures [6, 7, 8, 9]. Furthermore, additional complications can occur due to surgical excision of symptomatic OCEs, such as brachial artery pseudoaneurysm, constant pain, and improper resections leading to recurrence. To avoid recurrence, wide resection is done, and the whole cartilage cap and bone are removed from the base, after which the whole base is cauterized using electric cauterization [10, 11, 12]. Most data concerning surgical treatment of proximal humerus OCE are based on case reports or small case series, particularly in the skeletally immature patient [10]. Here, we present a case of recurrent OCE of the proximal humerus enclosing the brachial artery.
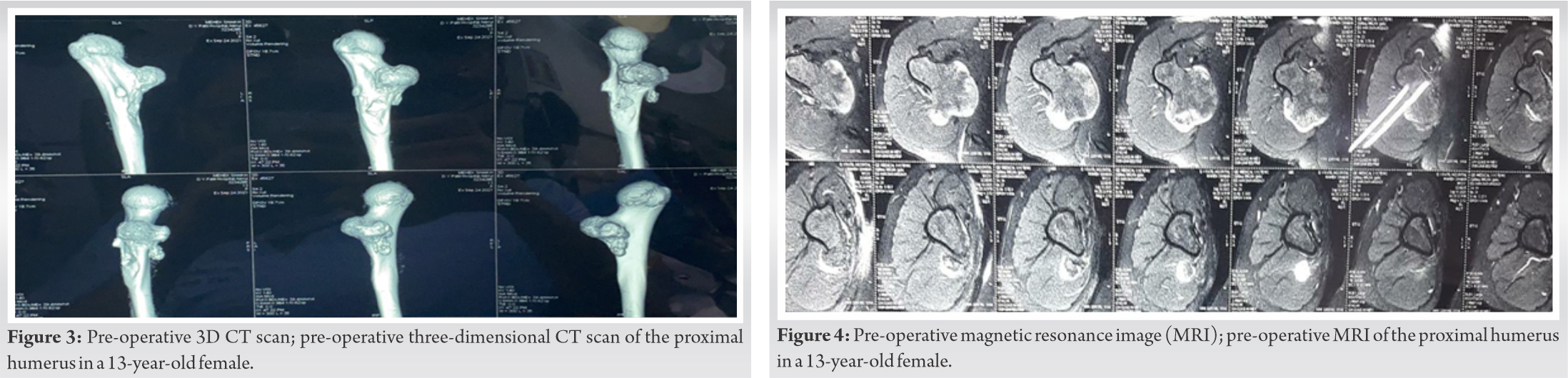
We report a unique case of a 13-year-old female who had presented with a history of pain and recurrent swelling for 5 years. On physical examination, the swelling was of size 4.4 cm × 3.7 cm × 4 cm, non-tender, non-mobile, two in number, non-cystic without any redness or sinus discharge, no visible pulsations, and no dilated veins. A 10 cm previous scar mark was present and the brachial artery pulsations were felt just over the swelling with a previous history of swelling at the same place, for which she was operated in 2018 (Fig. 1). The patient provided with discharge card and radiological investigation of previous surgery of a tertiary hospital from which OCE was diagnosed. CT reports were suggestive of a large well defined broad-based exophytic diaphyseal lesion in the medial side of the proximal humerus extending posteriorly (Fig. 2, 3). It measured approximately 4.4 cm × 3.7 cm × 4 cm in size. Another similar morphological lesion measuring approximately 9 mm × 7 mm was noted involving the posterior humeral shaft (Fig. 4). The minimal distance between the lesion and the brachial artery was 2 mm just anterior to the posteriomedial growth.
A cardiovascular thoracic team was involved for the dissection and a 6 cm incision was taken on the previous scar. The tumor was first dissected posteriorly (Fig. 5). A first interval was made between biceps brachii muscle and triceps brachii muscle. Then, the neurovascular bundle was identified and retracted followed by a second interval made by splitting the biceps brachii muscle. The anterior tumor was identified, after which the brachial artery was isolated and posteromedial exostosis was removed with the help of an osteotome of size 6 cm × 4 cm × 3.7 cm. This was followed by anterior exostosis of size 1 cm × 1.2 cm and of the whole cartilage cap was excised and electrical cauterization of the base was done to prevent further reoccurrence and a requirement of second surgery. Postoperatively, the patient was started on broad spectrum antibiotics and shoulder and elbow range of motion exercises were started post-operative day 1. The patient was discharged on post-operative day 5 and suture removal was done on post-operative day 14. Immediate post-operative X-Ray and post-operative 6 months X-Ray were done (Fig. 6, 7).
OCE is a cartilage-capped bony exostosis on the external surface of a bone containing a marrow cavity continuous with that of the underlying bone. Most cases are identified in children and adolescents which could be asymptomatic or complicated due to fractures and other lesions. OCEs may become malignant in approximately 1% of solitary forms and around 3–25% of multiple forms [13]. OCE can also recur post-excision if it has been removed imperfectly and is in close proximity to neurovascular structures. Although, this might not always be true. In a study reported by Vallance et al., they present cases of vascular complications of OCE. In one of the cases, they report an OCE of 6 cm in diameter arising from the upper medial fibula in a 19-year-old football player. Arteriography revealed complete occlusion of the proximal 2–3 cm of the anterior tibial artery. The posterior tibial artery was displaced backward and reduced above the origin of the peroneal artery [14,15].
In another case, a 24-year-old man presented with swelling in the upper part of his right arm with pain. The authors reported a very large calcified OCE arising from the upper humerus and clinical examination revealed reduced but palpable brachial and radial pulses. It was observed that there was marked forward displacement of the brachial artery which was lengthened and narrowed by extrinsic compression. Successful resection was done with placement of a vascularized graft [14]. Both these cases demonstrate that when presented with a case of recurrent OCE, proper removal of tumor is important keeping in view any blood vessels or nerves surrounding the tumor.
Proper curettage and excision of the tumor were done after dissecting and removing the soft tissue, blood vessels, and nerves so that there were very less chances of relapse. Post-operative X-ray was done and post 6 months of follow-up, there were no changes, and no relapse was observed. To conclude, OCE of the proximal humerus near the base of the axilla should always be excised properly so that the chances of reoccurrence should be very less as the neurovascular bundle is very near to the shaft.
When presented with a case of recurrent OCE of the proximal humerus, OCE could also be in proximity to important vasculature as in this case enclosing the brachial artery. Thus, proper curettage and excision should be done in such cases to avoid recurrence.
References
- 1.Garcia RA, Inwards CY, Unni KK. Benign bone tumors recent developments. Semin Diagn Pathol 2011;28:73-85. [Google Scholar]
- 2.Brien EW, Mirra JM, Luck JV Jr. Benign and malignant cartilage tumors of bone and joint: Their anatomic and theoretical basis with an emphasis on radiology, pathology and clinical biology. II. Juxtacortical cartilage tumors. Skeletal Radiol 1999;28:1-20. [Google Scholar]
- 3.Tepelenis K, Papathanakos G, Kitsouli A, Troupis T, Barbouti A, Vlachos K, et al. Osteochondromas: An updated review of epidemiology, pathogenesis, clinical presentation, radiological features and treatment options. In Vivo 2021;35:681-91. [Google Scholar]
- 4.Motamedi K, Seeger LL. Benign bone tumors. Radiol Clin North Am 2011;49:1115-34. [Google Scholar]
- 5.Kitsoulis P, Galani V, Stefanaki K, Paraskevas G, Karatzias G, Agnantis NJ, et al. Osteochondromas: Review of the clinical, radiological and pathological features. In Vivo 2008;22:633-46. [Google Scholar]
- 6.Bae DS, Kim JM, Reidler JS, Das De S, Gebhardt MC. Surgical treatment of osteochondroma of the proximal humerus: Radiographic and early clinical results. J Pediatr Orthop 2014;34:529-33. [Google Scholar]
- 7.Onga T, Yamamoto T, Akisue T, Marui T, Kurosaka M. Biceps tendinitis caused by an osteochondroma in the bicipital groove: A rare cause of shoulder pain in a baseball player. Clin Orthop Relat Res 2005;431:241-4. [Google Scholar]
- 8.Padua R, Castagna A, Ceccarelli E, Bondì R, Alviti F, Padua L. Intracapsular osteochondroma of the humeral head in an adult causing restriction of motion: A case report. J Shoulder Elbow Surg 2009;18:e30. [Google Scholar]
- 9.Cho CH, Jung GH, Song KS, Min BW, Bae KC, Lee KJ. Osteochondroma of the bicipital tuberosity causing an avulsion of the distal biceps tendon. Orthopedics 2010;33:1-3. [Google Scholar]
- 10.Bottner F, Rodl R, Kordish I, Winkelmann W, Gosheger G, Lindner N. Surgical treatment of symptomatic osteochondroma: A three-to eight-year follow-up study. J Bone Joint Surg Br 2003;85:1161-5. [Google Scholar]
- 11.Scotti C, Marone EM, Brasca LE, Peretti GM, Chiesa R, Del Maschio A, et al. Pseudoaneurysm overlying an osteochondroma: A noteworthy complication. J Orthop Traumatol 2010;11:251-5. [Google Scholar]
- 12.Zwierzchowski TJ, Fabis J. Double recurrent humerus osteochondroma. Chir Narzadow Ruchu Ortop Pol 2004;69:55-7. [Google Scholar]
- 13.Ramos-Pascua LR, Sanchez-Herraez S, Casas-Ramos P, Mora-Fernández M, Izquierdo-García FM. Osteochondromas of the proximal humerus. Diagnostic and therapeutic management. Rev Esp Cir Ortop Traumatol 2018;62:168-77. [Google Scholar]
- 14.Vasseur MA, Fabre O. Vascular complications osteochondromas. J Vasc Surg 2000;31:532-8. [Google Scholar]
- 15.Vallance R, Hamblen DL, Kelly IG. Vascular complications of osteochondroma. Clinical radiology. 1985;36:639-42. [Google Scholar]