We suggest a novel procedure of posterior vertebral column resection using a lateral lumbar interbody fusion cage.
Dr. Akira Itoi, Department of Orthopedic Surgery, Juntendo Shizuoka Hospital, 1129, Nagaoka, Izunokuni-shi, Shizuoka, Japan. E-mail: aitoi@juntendo.ac.jp
IntroductionStable fixation with a wide-foot-plate expandable cage and lateral lumbar interbody fusion (LLIF) cage has been reported as the ideal treatment for vertebral pseudarthrosis or deformity after an osteoporotic vertebral fracture. (OVF). The procedure requires anterior surgery, which may be associated with unique complications. Therefore, we performed a novel procedure consisting of posterior vertebral column resection (PVCR) using a lateral lumbar interbody fusion LLIF cage.
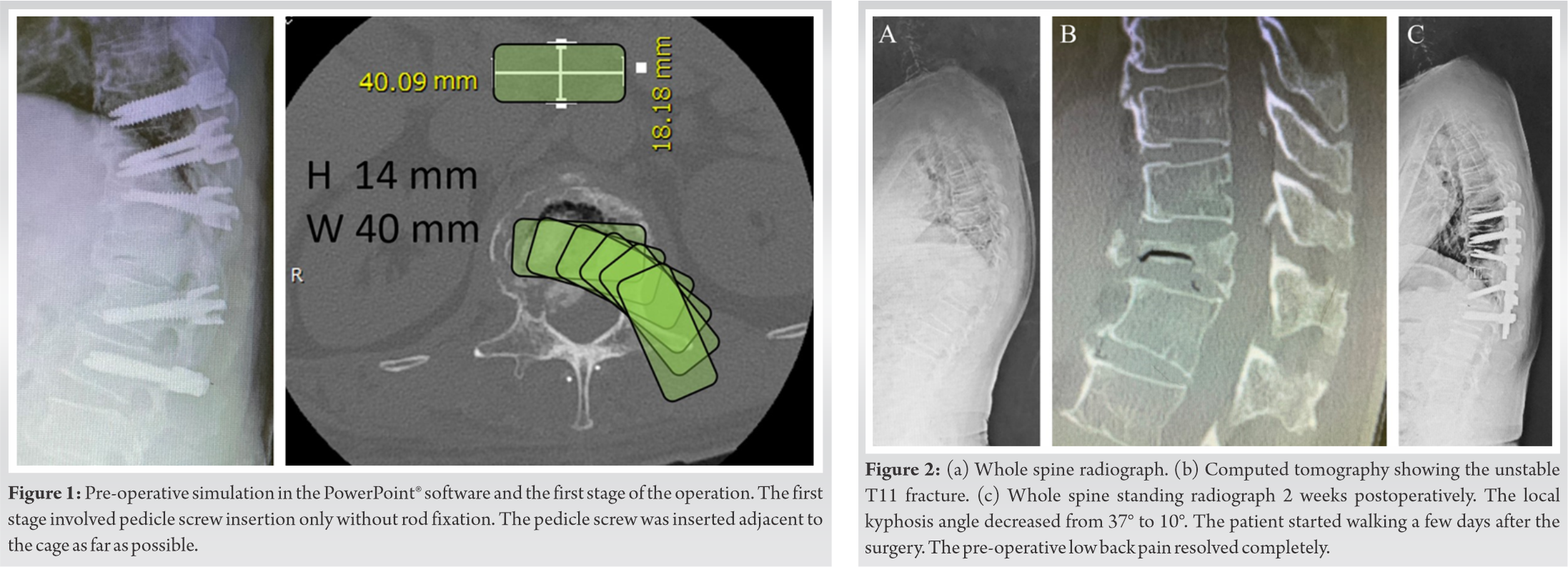
Case PresentationIn 2020, we prospectively studied three patients (one male and two female patients; mean age, 75.1 years) who underwent posterior insertion of a lateral lumbar interbody fusion LLIF cage for kyphotic deformity due to osteoporotic vertebral fractures. OVFs. The affected levels were L1, T12, and T11 in patients one, two, and three, respectively. The cage trajectory was confirmed by simulating the procedure using PowerPoint® software. Radiological outcomes were assessed using the angle of local kyphosis pre-preoperatively and postoperatively, and the clinical outcomes and neurological complications were reviewed. We inserted the cage smoothly and optimally in all three patients without sacrificing the nerve root, consistent with our pre-operative simulations. The mean operation time was 405 min (range, 368–433 min), and the mean blood loss was 845 mL (range, 800–865 mL). The mean local kyphotic angle was 46.3° preoperatively and 16.3° two2 weeks postoperatively. The pre-operative low back pain disappeared in all the patients. Post-operative neurological complications occurred in two of the patients, but did not interfere with walking rehabilitation.
ConclusionThe present study is the first to demonstrate that posterior insertion of a lateral lumbar interbody fusionLLIF cage is feasible in patients undergoing posterior vertebral column resection. PVCR.
KeywordsLLIFLateral lumbar interbody fusion cage, osteoporotic vertebral fracture, posterior vertebral column resection, posterior insertion, spinal deformity
Osteoporotic vertebral fractures (OVFs) are widely prevalent [1, 2] and are often treated conservatively [2]. However, surgical treatment may be necessary for pseudarthrosis, delayed nerve palsy, or kyphotic deformity, due to the patients’ decreased quality of life (QOL) [3]. An ideal reconstruction surgery should ensure stable fixation with minimal invasiveness to avoid adjacent-level fractures or kyphosis, which increases in proportion to surgical invasiveness.
Anterior-posterior short-segment spinal fusion using a wide-foot-plate expandable cage and lateral lumbar interbody fusion (LLIF) cage may be an ideal procedure [4, 5]. However, this approach is expensive [6, 7, 8] and may require additional anterior release in cases where local kyphosis in OVF malunion has not been corrected and requires an anterior surgical approach, which is, in turn, associated with complications [9]. Although Fukuda et al. reported a less invasive method using LLIF cages [5], it is difficult to achieve lordosis beyond the expandable cage in patients with anterior shortening; therefore, we considered a novel procedure comprising a posterior vertebral column resection (PVCR) using an LLIF cage.
This novel procedure is appropriate for patients with back pain or disability due to postural abnormality and for those with or without neurological symptoms, but not for patients with complete paralysis due to kyphotic deformity with severe anterior shortening malunion of a fractured vertebral body. Pre-operative planning for cage insertion was performed as follows. Cage trajectory was confirmed using PowerPoint® (Microsoft Corp., Redmond, WA, USA) and simulated by moving a shape that accurately imitated the cage shape and size on the axial image of the fractured vertebra, obtained from pre-operative computed tomography (Fig. 1). We confirmed that the cage could be inserted without even slight compression of the dura mater or excessive compression of the thorax.
Surgery was indicated for OVF malunion in the thoracolumbar spine, accompanied by severe low back pain that produced standing and gait abnormalities and decreased QOL. The patients’ clinical characteristics are listed in (Table 1).
The operation was initially planned as a two-stage procedure, involving pedicle screw insertion only (without rod fixation), followed by reconstructive surgery 1–3 weeks later. There were two reasons behind using a two-stage approach: First, to confirm the position of the patient under full paralysis at the initial surgery and to consider the method of anterior reconstruction, and second, to spread out the invasiveness. There is some debate about performing one-stage or two-stage surgery [10]. Nevertheless, since our surgical plan is to change the procedure based on intraoperative findings and reports have previously suggested that two-stage surgery is preferable for elderly patients, we decided to perform a two-stage surgery [11]. The patients were placed prone on the Relton-Hall frame to decrease kyphosis. The pedicle screw was placed above and below two levels or three levels if there were ankylosing changes in adjacent vertebrae, through a posterior midline incision. The pedicle screw (CREO system, Globus Medical, USA) adjacent to the cage was inserted under fluoroscopy as far as possible (Fig. 1). After 1–3 weeks, the second operation was performed. Using the same incision, the left side facet joint and adjacent laminae of the fractured vertebra were resected first. We then resected the disk adjacent to the fractured vertebra and performed transpedicular pediculectomy and vertebrectomy. The posterior wall and posterior longitudinal ligament were gently detached from the ventral surface of the dura mater and resected to the maximum extent. We connected a temporary rod to the left side and resected the right side in the same manner. The lateral wall of the fractured vertebra and osteophytes that developed adjacent to the upper and lower vertebrae was completely removed after the lateral wall blunt dissection, and the posterior wall was resected along with the posterior longitudinal ligament. We attempted a cage trial with a distraction force on the opposite or central side using the laminar distractor. If safe insertion was judged difficult in terms of the spinal cord safety or nerve roots, as envisaged in the pre-operative plan, the procedure was converted to a combined anterior-posterior approach or the nerve root was sacrificed. After confirming that the cage was properly positioned using fluoroscopy, the cage (OLIF25; cross-section, 40–45 mm; length, 18 mm; angle, 6°; Medtronic Sofamor Danek, USA), filled with milled local bone, was inserted into the cavity with gentle exiting nerve root retraction and without contacting the dura mater. Once the cage was positioned appropriately, 6.0 mm titanium alloy rods were applied to the pedicle screws, and the cage was fixed with compressive force to correct kyphotic deformity and spinal column shortening. Augmentation was performed using a rod and side connector that was stronger than the cross-links. Finally, the remaining milled local bone and demineralized bone matrix (Grafton Matrix Strips; Medtronic Sofamor Danek, USA) were embedded in the posterolateral side of the columns for posterolateral fusion. Intraoperatively, echocardiography and motor-evoked potentials were used to confirm the spinal cord status. Approximately 1–2 days postoperatively, the patients were allowed to get out of bed while using a thoracolumbar orthosis frame.
The cage could be inserted smoothly and optimally in all patients without touching the dura mater or sacrificing the nerve roots. Furthermore, motor-evoked potentials were maintained at ≥75%, pre-operative back pain disappeared quickly, and walking gradually recovered to pre-operative levels or higher. The mean follow-up period was 9 months (range: 6–12), and post radiographs at the final follow-up visit showed no signs of cage migration, implant failure, or adjacent-level kyphosis and fractures. A representative case of a 77-year-old man with a T11 vertebral fracture is shown in (Fig. 1, 2). The patient had been experiencing pain in the lower back for 20 months following an injury. This report was approved by the appropriate ethics review board, and all the patients provided written informed consent.
In all three representative cases of posterior insertion of a wide LLIF cage during the PVCR procedure, the cage insertion was smooth, pre-operative back pain disappeared quickly, and the patients’ walking level gradually recovered to pre-operative levels or higher. Recently, Fukuda et al. reported good results for interbody fixation with LLIF cage between fractured vertebrae using the usual LLIF technique for old OVF [5]. However, in principle, it is difficult to achieve lordosis using this method. This is because it is theoretically impossible to gain kyphosis by crushing the vertebral body that had a vacuum phenomenon and supporting them with the lateral walls while leaving the posterior column intact. Therefore, the technique described by Fukuda et al. [5] is not indicated for cases where kyphosis is related to the complaint. Using the LLIF cage in PVCR requires sufficient posterolateral soft-tissue expansion and resection of the vertebral body’s lateral walls. In this study, the LLIF cages with widths of ≥40 mm were inserted posteriorly in all the patients after simulation. In the third case, partial resection of the left 11th rib was necessary; however, in the other two cases, expansion of the surgical field beyond that required for PVCR was not required. The PowerPoint® software aided in the pre-operative simulation of the insertion trajectory. It was necessary to confirm the feasibility of the procedure preoperatively to ensure nerve protection. Although PowerPoint® can only display two-dimensional details, this did not limit our planning approach since we only required confirmation of organ location on a single plane. In all three cases, we used a length of 18 mm anteroposteriorly to ensure reliable insertion.
We performed a two-stage surgery under anesthesia to confirm the reduction position and to reduce surgical invasiveness. Thus, it was essential to preoperatively confirm whether the acceptable correction could be achieved without osteotomy or vertebral resection. Further, it is important to confirm the position of the maximum reduction in the pre-operative awake state and to know how well it can be reproduced intraoperatively. Ultimately, the most appropriate method for pragmatic evaluation of these factors is to use the lateral radiographic view in the prone position under general anesthesia. Two of the three patients had post-operative neurological complications with persistent motor dysfunction, which did not interfere with walking rehabilitation. These complications occurred immediately after the surgery in the second patient and after initiating loading in the third. The second patient developed mild numbness in both thighs that persisted regardless of posture and motion, possibly caused by intraoperative epiconus injury. The third patient developed post-operative symptoms associated with an injury around the right T10 root, which improved gradually. His symptoms appeared late postoperatively. Consequently, an intraoperative injury was ruled out. Although the most likely explanation was a hematoma, this was not evident in post-operative magnetic resonance imaging. Intraoperative ultrasound and neurophysiologic monitoring are essential for preventing neural complications, although nerve root sacrifice is sometimes necessary. It is critical to thoroughly check for the absence of compression and spinal cord extension and the nerve roots before and after the correction. Ultrasound findings revealed that the spinal cord was bent posteriorly in all the patients but without flattening. Motor-evoked potentials exhibited no abnormal decrease in intensity, and motor paralysis did not occur. The only adverse post-operative symptom was a sensory disturbance. To prevent and detect these complications, gentle and sufficient resection of the posterior longitudinal ligament and posterior wall, extensive laminectomy, and gentle correction is necessary, and somatosensory evoked potentials may also be considered. While our proposed surgical method helps avoid anterior insertion of the LLIF cage, it does not decrease the invasiveness of the PVCR procedure. Although we used a transverse connection with 5.5 mm rods to increase the fixation force and decrease the fusion level, the impact of these two surgical choices could not be assessed. In addition, the correction of the kyphotic deformity was approximately 30°. However, this did not help to achieve satisfactory results consistently and remains a technical challenge that must be addressed.
The present study is the first to demonstrate that posterior insertion of a LLIF cage is feasible in patients undergoing PVCR. This report highlights the possibility that the cages for LLIF can be inserted posteriorly.
LLIF cage can be inserted posteriorly during PVCR. However, careful planning and optimized technique are necessary. A wide cage for posterior insertion may be developed in the future.
References
- 1.Bow CH, Cheung E, Cheung CL, Xiao SM, Loong C, Soong C, et al. Ethnic difference of clinical vertebral fracture risk. Osteoporos Int 2012;23:879-85. [Google Scholar]
- 2.Harada A, Matsuyama Y, Nakano T, Deguchi M, Kuratsu S, Sueyoshi Y, et al. Nationwide survey of current medical practices for hospitalized elderly with spine fractures in Japan. J Orthop Sci 2010;15:79-85. [Google Scholar]
- 3.Hu SS. Internal fixation in the osteoporotic spine. Spine 1997;22:43S-8. [Google Scholar]
- 4.Taiji R, Takami M, Yukawa Y, Hashizume H, Minamide A, Nakagawa Y, et al. A short-segment fusion strategy using a wide-foot-plate expandable cage for vertebral pseudarthrosis after an osteoporotic vertebral fracture. J Neurosurg Spine 2020;33:1-8. [Google Scholar]
- 5.Fukuda K, Katoh H, Takahashi Y, Kitamura K, Ikeda D. Minimally invasive anteroposterior combined surgery using lateral lumbar interbody fusion without corpectomy for treatment of lumbar spinal canal stenosis associated with osteoporotic vertebral collapse. J Neurosurg Spine 2021;1:1-9. [Google Scholar]
- 6.Goz V, Weinreb JH, Schwab F, Lafage V, Errico TJ. Comparison of complications, costs, and length of stay of three different lumbar interbody fusion techniques: An analysis of the Nationwide Inpatient Sample database. Spine J 2014;14:2019-27. [Google Scholar]
- 7.Yamamoto T, Yagi M, Suzuki S, Nori S, Tsuji O, Nagoshi N, et al. Limited cost benefit of lateral interbody fusion for adult spinal deformity surgery. Spine 2021;46:48-53. [Google Scholar]
- 8.Arutyunyan GG, Angevine PD, Berven S. Cost-effectiveness in adult spinal deformity surgery. Neurosurgery 2018;83:597-601. [Google Scholar]
- 9.Fujibayashi S, Kawakami N, Asazuma T, Ito M, Mizutani J, Nagashima H, et al. Complications associated with lateral interbody fusion: Nationwide survey of 2998 cases during the first 2 years of its use in Japan. Spine 2017;42:1478-84. [Google Scholar]
- 10.Henry HY, Asuma MP, Wallace CS, Kelly MP, Kang DG. Should surgery for adult degenerative lumbar deformity be staged? Clin Spine Surg 2019;32:269-71. [Google Scholar]
- 11.Yoshida G, Hasegawa T, Yamato Y, Kobayashi S, Oe S, Banno T, et al. Predicting perioperative complications in adult spinal deformity surgery using a simple sliding scale. Spine (Phila Pa 1976) 2018;43:562-70. [Google Scholar]