Although diagnosis of tubercular tenosynovitis is difficult, drug therapy can be initiated empirically on strong suspicion of tuberculosis, especially in TB endemic areas.
Dr. Madhan Jeyaraman, Department of Orthopaedics, Faculty of Medicine, Sri Lalithambigai Medical College and Hospital, Dr. MGR Educational and Research Institute, Chennai, Tamil Nadu, India. E-mail: madhanjeyaraman@gmail.com
IntroductionTubercular tenosynovitis of the wrist and hand, although rare, presents a diagnostic dilemma primarily due to its non-specific clinical presentation, insidious course, and the large number of differentials that mimic it. When the diagnosis is late or delayed, significant bone and tendon complications occur. Large progressive swelling around the wrist in TB endemic countries should raise an early suspicion of being of tubercular etiology and should be high on the list of differential diagnoses.
Case ReportA 48-year-old female presented with a large progressive swelling on the volar aspect of the left wrist and palm for 7 months, associated with increasing pain, stiffness, limited wrist range of movements, and weakened grip strength. Magnetic resonance imaging (MRI) revealed synovitis and fluid within flexor tendon synovial sheaths. The patient underwent an excision of the mass in toto and the cut section revealed an irregularly thickened wall with rice bodies within. Histopathological examination was indicative of a large ganglion cyst. GeneXpert MTB/RIF assay detected Mycobacterium tuberculosis. Despite histopathology being inconclusive, a diagnosis of TTS was considered due to the patient’s clinical presentation, MRI, and operative findings. The patient was started on an antitubercular drug regimen for a 1-year duration. The patient regained a complete range of movements of fingers and wrist and normal grip strength at the 3rd month follow-up.
ConclusionTTS is a challenging diagnosis entity. The diagnostic confirmation was achieved either by histopathology or detection of the organism either by culture or GeneXpert MTB/RIF assay. When the diagnosis is unsupported, drug therapy can be initiated empirically on strong suspicion of tuberculosis, especially in TB endemic areas.
KeywordsCompound palmar ganglion, Tubercular flexor tenosynovitis, Rice bodies.
Tubercular tenosynovitis (TTS) has also been known as compound palmar ganglion (CPG) which is a misnomer [1]. Its differential diagnosis includes a vast number of inflammatory and infective pathologies of the hand, making diagnosis difficult [2, 3]. Large progressive swelling in wrist or hand, with or without pain, limited range of movement (ROM) of wrist and fingers, weak grip strength, or presenting with median nerve compression [4] symptoms in tuberculosis (TB) endemic area must raise the suspicion of it being of tubercular etiology [4, 5, 6, 7]. Its insidious nature and slow progression usually delay diagnosis [2, 4, 7]. Laboratory tests and other investigative tools are useful diagnostic aids but are non-specific [4, 5, 6, 7, 8]. Absolute confirmation is by finding typical tubercular lesions on histopathological examination (HPE) or detection of Mycobacterium TB in microbiological tests [1, 2]. Suspicious cases must undergo excision biopsy, meticulous debridement with tenosynovectomy, and complete antitubercular therapy (ATT) to provide favorable outcomes [1, 4, 6]. We describe a case of TTS of the wrist presenting as a large dumbbell swelling that mimicked a large ganglion cyst.
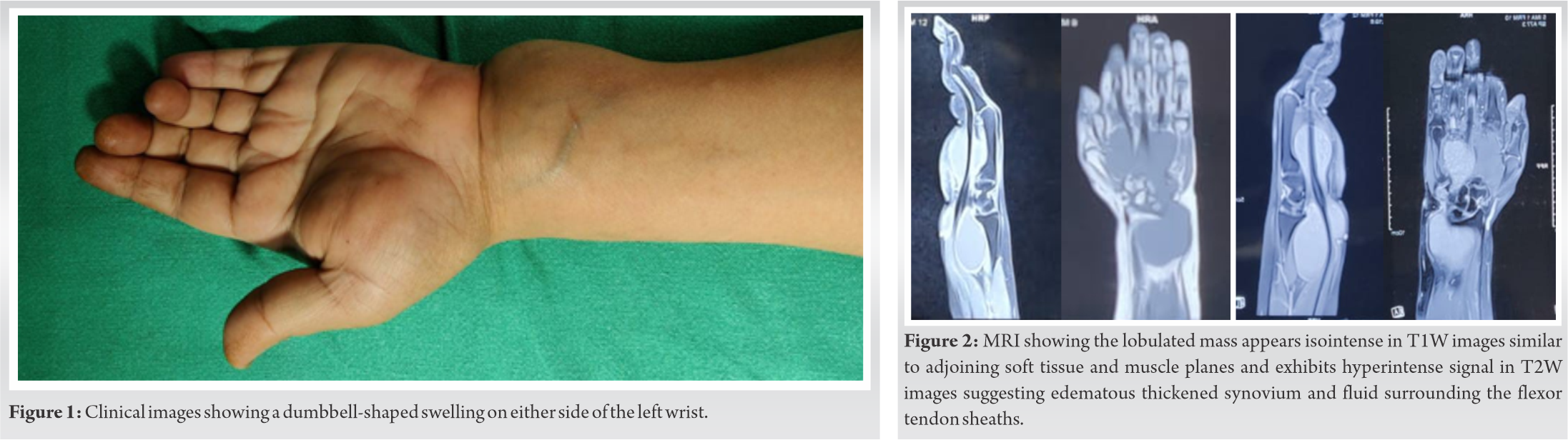
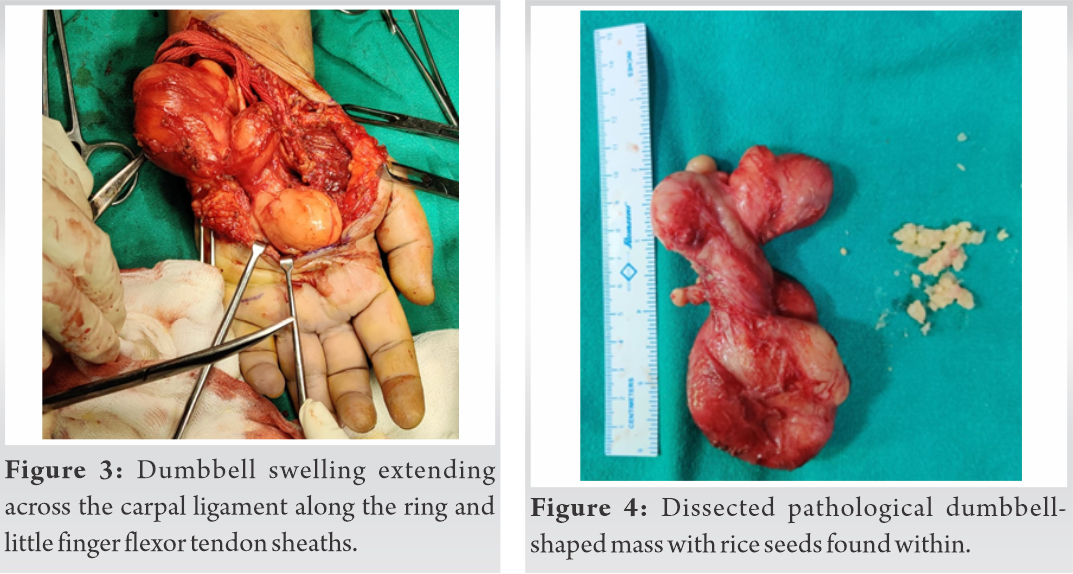
A 48-year-old female presented with a painless progressive swelling on the volar aspect of the left wrist and palm for 7 months associated with restricted wrist movements and weakened grip. She had no other comorbidities or previous exposure to TB. Examination revealed two swellings approximately 7 cm × 5 cm on the ulnavolar aspect of the wrist on either side of the carpal ligament, as shown in (Fig. 1), which was non-pulsatile, compressible, doughy in nature, and without any local signs of inflammation. Wrist ROM and grip strength were reduced without any distal neurovascular deficits. Lymph nodes, chest, spine, and other systems were clinically normal. Laboratory tests were essentially normal other than an elevated erythrocyte sedimentation rate of 40 mm in the 1st h. Wrist and hand X-rays revealed soft-tissue swelling shadow on the flexor aspect and periarticular osteoporosis of the wrist bones. Magnetic resonance imaging (MRI) revealed a lobulated altered signal intensity lesion seen in the distal forearm region along its flexor aspect and extending into the palmar hypothenar aspect of the hand engulfing the flexor tendons in a dumbbell fashion. The lobulated swelling appears iso-intense in T1-weighted images (WI) to adjoining soft-tissue muscle planes and exhibits a bright signal in T2-weighted axial images and short-tau inversion recovery sequences suggestive of thickened synovium and fluid surrounding the flexor tendon sheaths, as shown in (Fig. 2). Intraoperative, a large encapsulated mass arising from the ulnar bursa proximal to carpal ligament and extending distally to encompass the tendons sheaths of the ring and little fingers. On severing the carpal tunnel, the swelling was found to be in continuation in a dumbbell fashion across the carpal tunnel with the ring and little finger tendon sheaths. With meticulous dissection, the mass lesion was successfully removed in toto, as shown in (Fig. 3). To avoid spillage of contents and to remove the lesion en-masse, a tenotomy of the ring finger tendon was done as it was completely engulfed by the synovial mass and later resutured with Prolene 4-0 suture. The cut section revealed an irregularly thickened wall of the cyst cavity filled with yellowish material suggestive of rice bodies, as shown in (Fig. 4). The excised mass was sent for HPE and microbiological analysis. Grossly, a large irregular multilobed structure externally encapsulated with dimensions approximately 12 cm × 6 cm × 3 cm. Microscopic examination revealed fragments of a cystic wall which was made up of fibrocollagenous tissue containing necrotic material with thickened synovium and yellow cheesy material, which was suggestive of a large ganglion cyst. Tissue samples sent for Gram stain, acid-fast bacilli (AFB) staining, and aerobic culture sensitivity were negative. Samples subjected to the GeneXpert MTB/RIF assay for the detection of Mycobacterium TB revealed a positive result. Tissue sample staining or HPE did not reveal TB affection. The patient’s clinical presentation, MRI findings, intraoperative findings, and positive GeneXpert MTB assay report guided us to start the patient on daily ATT (2[HRZE] and 10[HRE]) regimen. Postoperatively, the hand and wrist were maintained in a posterior slab in a functional position. Under supervision, early active mobilization of fingers and wrist was started once the patient was pain free. The patient was reviewed at 3, 6, and 12 months post-surgery for follow-up. Her surgical wound healed well with no scar complications. At 3-month post-surgery, the patient had obtained full ROM of fingers and wrist. She reported a complete return to functional activity with good grip strength, using the affected hand in daily activities, as shown in (Fig. 5a, b, c).
TTS represents only 2–5% of osteoarticular TB [7]. The hand and wrist are the most common site, although rare it occurs in 10% of all osteoarticular lesions with most lesions found on the flexor and ulnar aspect of the hand and wrist [1, 2, 4, 5, 6, 7]. TTS involving the radial and ulnar bursa (CPG) is rare but not uncommon in TB endemic zones [4, 5, 6, 9]. Pathogenesis of TTS is commonly by hematogenous spread from primary foci within lungs, lymph nodes, bone, or direct inoculation [5, 9]. Risk factors include males, trauma, dominant hand with overuse, low socioeconomic status, old age, malnutrition, and immunocompromised status [1, 7, 9]. Our patient did not fit the risk factors profile commonly described in the literature and neither the mechanism of infection was clear although she belonged to a TB endemic region.
TTS progresses through three histopathological stages depending on the virulence of the organism, duration of disease, and resistance of the individual [10]. In the hygromatous stage, there are serous exudates within the tendon sheath but the tendon is unaffected, in the serofibrinous stage, the tendon sheath is replaced by granulation tissue and is followed by the formation of rice or melon bodies. In the fungoid stage, there is caseation, abscess and sinus formation, bone involvement, and tendon rupture. If untreated, TTS may spread to adjacent bones and joints and deep spaces of the hand and forearm [1]. The progression of the disease is slow and insidious [4, 7]. Initially, the symptoms are minimal with a gradually progressive swelling which becomes evident many months later with restricted movements of fingers and wrist [1, 5, 6]. Local inflammatory signs are usually discreet or absent [2, 5, 7]. Another common presentation of TTS is a slow-growing sausage-shaped mass [7] along the affected tendon sheath with or without pain or as a CPG [1, 2, 4] presenting as a painless progressive swelling proximal and distal to the carpal tunnel and mostly involving the flexor tendon of the little finger [6], and ulnar bursa with the presence of rice bodies [2, 3, 4]. Some may present with carpal tunnel syndrome [1, 4, 6]. Pyogenic and fungal infections, brucellosis, foreign body tenosynovitis, sarcoidosis, rheumatoid arthritis, gouty arthritis, de Quervain’s disease, pigmented villonodular synovitis, systemic lupus erythematosus, and ganglion cyst forms the list of differential that needs to be considered with such a swelling [2, 3].
Diagnosis is most often delayed due to insidious onset and non-specific clinical presentation [2, 4]. Our patient had a similar swelling extending across the carpal ligament with restricted wrist movements and weakened grip but no nerve compression symptoms. Local signs of inflammation over the swelling were absent and a systemic search did not reveal any tubercular foci of infection. Laboratory investigations such as complete blood count, erythrocyte sedimentation rate, and C-reactive protein may be normal [1, 5, 6] or elevated in such cases [4, 11], but these are non-specific for TTS and it cannot be excluded when these tests are normal [2, 5]. Chest X-ray in extrapulmonary TB is most often normal and cannot exclude a diagnosis of TTS [2, 5, 11]. Radiographic features of TTS affecting the wrist include bone erosions or cavitation, localized osteoporosis, gross destruction, and ankylosis at late stages [8]. These findings are non-specific and may deceptively mimic inflammatory arthritis, pigmented villonodular synovitis, gout, or a soft-tissue tumor [8]. Ultrasonography, for evaluating patients with suspected TTS, can detect synovial thickening, peritendinous effusion, pus formation, and extension of lesions, however, they are operator dependent and non-specific [5]. MRI is more sensitive and specific than USG for detecting and visualization of tubercular synovial tendon sheaths. Prominent synovial thickening around the flexor tendons with the fluid collection is the recognized MR findings [2, 6, 8]. The thickened tenosynovium presents as hypointense signal intensity on T1WI and characteristic hypointense synovium on T2WI is suggestive of granuloma and seen in 40% of cases [8]. Synovial fluid usually demonstrates hypointense signal intensity on T1WI and predominantly hyperintense signal intensity on T2WI. The small low signal foci or dots scattered in the synovial fluid on T2WI may refer to regions of tissue debris, caseous material, or rice bodies. In our patient, MRI findings revealed a lobulated dumbbell shape swelling arising from the synovial sheaths with images suggestive of thickened synovium and fluid within flexor tendon sheaths which are consistent with TTS. The ultimate diagnosis is by HPE and microbiological tests [1, 2, 5, 7]. HPE findings usually reveal granulomatous lesions showing central caseation and surrounded by multiple giant cells and epithelioid cells confirming TB [5, 7]. The characteristic “rice bodies” or “melon seeds bodies” are found inside the synovial sheaths of tendons [2, 3, 4, 5, 6]. Rice bodies found in TTS consist of fibrinous masses (tubercles) and formed due to microinfarction following inflammation and ischemia of the synovial sheath and are present in 50% of cases [7]. According to Woon, the presence of rice bodies together with “millet” or “melon seed”-shaped lesions are diagnostic of TTS, but rice body formation also occurs in rheumatoid arthritis, seronegative arthritis, SLE, and osteoarthritis hence making diagnosis difficult [3]. Microbiological studies are usually insufficient; because AFB can be detected in only 10% synovial fluid, 20 % synovial tissue, and 30% regional lymph nodes, and therefore, negative findings cannot exclude the disease [5]. The lesion excised from our patient grossly resembled a CPG with rice bodies within it but HPE did not support the diagnosis. When the diagnosis is uncertain and tissue cultures are pending or delayed, crucial time is lost which may delay diagnosis and treatment. Hence with a provisional diagnosis of TB, ATT can be started empirically [7].
In our patient, the HPE report indicated a large ganglion cyst, but the patient’s history, being a TB endemic region, clinical signs, intraoperative findings, and positive GeneXpert, was suggestive of a TTS presenting as a CPG. We started the patient on ATT using four drugs – isoniazid, rifampicin, ethambutol, and pyrazinamide for 2 months and continued with isoniazid, rifampicin, and ethambutol for 10 months. In literature, the duration of ATT ranges from 6 to 12 months with surgical debridement [1, 2, 4, 5, 6]. Some authors have reported complete resolution of TTS using 12 months of ATT without any need for surgical debridement [11]. ATT should be started as soon as possible after diagnosis and completing the full course is essential to prevent recurrence and resistant strains [5]. The role of surgical debridement as the first line of management in TTS is controversial [10, 11]. Tuli recommends that surgical debridement should be performed on an in-patient who is resistant to 4 or 5 months of ATT [10]. Other indications are large mass lesions requiring debulking, late (Stage 2 or 3) stage of the disease [5], and those causing median nerve compression [4, 7]. Many authors recommend that this condition should be treated surgically by a debulking tenosynovectomy and appropriate chemotherapy and with the release of the carpal tunnel to prevent further recurrence [4, 7, 11]. We advocate that for patients presenting with a large mass with restricted wrist movements and poor grip, a debulking procedure is a must. This will provide tissue for HPE and microbiological testing, thorough debridement with synovectomy will reduce the initial bulk of the disease, and carpal ligament release will not only decompress the carpal tunnel contents but also allow better access to the lesion with direct visualization of the affected tendon, tendon sheaths, and median nerve.
TTS of the hand, although a rare entity, is still commonly encountered in TB endemic zones. It poses a diagnostic dilemma because of its slow progression, non-specific clinical picture, and a large list of differentials. Delayed diagnosis leads to significant complications involving the tendon, bone, and joint. Laboratory investigations, X-rays, USG, and MRI are helpful modalities but lack specificity. Final confirmation is HPE or isolation of TB from tissue samples. In clinical scenarios, where the diagnosis is unsupported by HPE or microbiology, a provisional diagnosis of TTS can be considered in highly suspicious cases and ATT can be empirically started to prevent late complications. Complete ATT is the mainstay of treatment with debulking synovectomy a must for patients with large swellings, pressure symptoms, or a weakened grip.
TTS can present as large dumbbell swelling around the wrist which can mimic a large ganglion cyst. The presence of rice bodies or melon seed bodies is strongly suggestive of a tubercular etiology but needs to be corroborated with HPE or microbiological tests. Even when the diagnosis is unsupported by HPE or microbiological studies, highly suspicious cases in TB endemic zones can be empirically started on ATT with adjuvant debridement and synovectomy.
References
- 1.1. Wali H, Al-Khuwaitir S, Hafeez MA. Compound palmar ganglion: A case report and literature review. Ann Saudi Med 1986;6:55-8. [Google Scholar]
- 2.2. Bayram S, Ersen A, Altan M, Durmaz H. Tuberculosis tenosynovitis with multiple rice bodies of the flexor tendons in the wrist: A case report. Int J Surg Case Rep 2016;27:129-32. [Google Scholar]
- 3.3. Woon CY, Phoon ES, Lee JY, Puhaindran ME, Peng YP, Teoh LC, et al. Rice bodies, millet seeds, and melon seeds in tuberculous tenosynovitis of the hand and wrist. Ann Plast Surg 2011;66:610-7. [Google Scholar]
- 4.4. Altaf W, Attarde D, Sancheti P. Tubercular compound palmar ganglion presenting as a severe carpal tunnel syndrome a case report. J Clin Orthop Trauma 2020;11:S889-91. [Google Scholar]
- 5.5. Suwannaphisit S, Ranong NN. Tuberculous tenosynovitis of the flexor tendons of the hand and wrist: A case report and mini-review. Ann Med Surg(Lond) 2020;57:249-52. [Google Scholar]
- 6.6. Panigrahi S, Jain M, Panda R. Patient with tuberculous flexor tenosynovitis of the hand. BMJ Case Rep 2021;14:e243091. [Google Scholar]
- 7.7. Baidoo PK, Baddoo D, Ocloo A, Agbley D, Lartey S, Baddoo NA, et al. Tuberculous tenosynovitis of the flexor tendons of the wrist: A case report. BMC Res Notes 2018;11:238. [Google Scholar]
- 8.Rajadurai N. Tuberculous tenosynovitis of the wrist joint: Imaging findings on MRI. J Infect Dis Ther 2016;4:307. [Google Scholar]
- 9.Higuchi S, Ishihara S, Kobayashi H, Arai T. A mass lesion of the wrist: A rare manifestation of tuberculosis. Intern Med 2008;47:313-6. [Google Scholar]
- 10.Tuli SM. Tuberculosis of the Skeletal System: Bone, Joints, Spine, and Bursal Sheaths. 3rd ed. New Delhi: Jaypee Brothers Medical Publishers; 2004. [Google Scholar]
- 11.Jain A, Rohilla R, Devgan A, Wadhwani J. Tubercular tenosynovitis of hand: A rare presentation. J Orthop Case Rep 2016;6:69-72. [Google Scholar]