Symptomatic osteochondromas in proximal femur can be excised with mini-arthrotomy to avoid damage to femur head blood supply.
Dr. Pranay Kondewar, Department of Orthopaedics, Grant Government Medical College and JJ Hospital, Byculla, Mumbai - 400 008, Maharashtra, India. E-mail: pranaypk1@gmail.com
Introduction: Osteochondromas are the most common benign bone tumors. They probably are developmental malformations rather than true neoplasms and are thought to originate within the periosteum as small cartilaginous nodules. The lesions consist of a bony mass produced by progressive endochondral ossification of a growing cartilaginous cap. Osteochondromas usually are found on the metaphysis of a long bone near the physis such as distal femur, proximal tibia, and proximal humerus. Surgical treatment for femur neck osteochondroma is difficult due to the high risk of avascular necrosis following excision. These lesions in femur are in close proximity to important neurovascular bundle and can cause ymptoms related to their compression. Furthermore, the symptoms related to labral tear and hip impingement are common. Recurrence is rare and is caused by failure to remove the entire cartilaginous cap.
Case Report: A 25-year-old female presented with the complaints of pain in the right hip and difficulty in walking and running for 1 year. On radiological examination, the right femur neck osteochondroma was diagnosed, it as located along the posteroinferior margin of the femur neck. Surgical removal of the lesion was done in lateral decubitus position using osterolateral approach to hip without dislocation of the femur.
Conclusion: Osteochondroma at femur neck can be safely removed without surgical hip dislocation. It’s necessary to remove it completely to avoid recurrence.
Keywords: Osteochondroma, proximal femur osteochondroma, benign bone tumor, femur neck osteochondroma, hereditary multiple exostoses.
Osteochondromas are most common benign bone tumors. They probably are developmental malformations rather than true neoplasms and are thought to originate within the periosteum as small cartilaginous nodules. The lesions consist of a bony mass, often in the form of a stalk, produced by progressive endochondral ossification of a growing cartilaginous cap [1]. Osteochondromas are hamartomatous proliferations of both bone and cartilage that are thought to arise from trapped growth plate cartilage, extend through the cortex, and grow through endochondral ossification beneath the periosteum. Osteochondromas grow until skeletal maturity and stop once the growth plate fuse, though slow growth from the cap may continue over time, this usually stops by age of 30. In contrast to true neoplasms, their growth usually parallels that of the patient and usually ceases when skeletal maturity is reached. Most lesions are found during the period of rapid skeletal growth. About 90% of patients have only a single lesion. Osteochondromas may occur on any bone preformed in cartilage but usually are found on the metaphysis of a long bone near the physis. They are seen most often on the distal femur, the proximal tibia, and the proximal humerus [2]. However, intra-articular osteochondromas may also occur, causing pain and discomfort and restricting the range of motion. The ratio of the diameter of the femoral neck to that of the shaft as an index of overgrowth of the femoral neck. This neck overgrowth also results in the discontinuity of Shenton’s line. Selective overgrowth along the inferior side can lead to coxa valga. The increased ratio of the neck/shaft diameter in patients with HME may simply reflect the presence of sessile osteochondromas of the femoral neck [3]. All the three features are seen in this patient bilaterally. Determining the optimal treatment may be difficult due to the high risk of avascular necrosis (AVN) following surgical excision due to the lesion location [4]. We herein report a rare case of an intra-articular osteochondroma involving the posteroinferior aspect of the femoral neck. Osteochondromas are of two types: Pedunculated and/or sessile. Pedunculated tumors are more common, and any definite stalk is directed away from the physis adjacent to which it takes its origin. The projecting part of the lesion has cortical and cancellous components, both of which are continuous with corresponding components of the parent bone. The lesion is covered by a cartilaginous cap that often is irregular and usually cannot be seen on radiograph. Recurrence is rare and probably is caused by failure to remove the entire cartilaginous cap.
A 25-year-old female presented with the complaints of pain in the right hip and difficulty in walking and running for 1 year. On examination, there was restriction of terminal external rotation and extension. Radiological investigation suggestive of an exophytic growth along the posteroinferior margin of the right femur neck (Fig. 1).
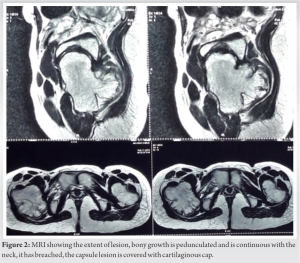
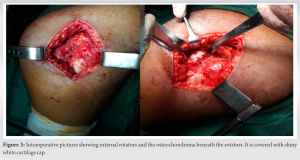

Osteochondroma is diagnosed as a solitary lesion or as part of a hereditary multiple osteochondromatosis involving the hip in 30–90% of patients. Approximately 25% of these patients have growth anomalies such as medial hyperostosis, femoral lateralization, coxa valga, and progressive acetabular dysplasia with the possibility of subluxation and dislocation of the hip and progressive deformity of the femoral head [5]. Possible clinical presentations that can arise from these lesions such as labral tears, nerve compression, hip dislocation, external snapping hip, acetabular dysplasia ,vascular compromise, and rarely malignant transformation. Because of the specific anatomy, osteochondroma of the femoral neck may lead to mechanical restriction of hip motion. Mechanical blocking occurs through direct contact of the widened and enlarged femoral neck against the ischium or the acetabular rim or both, which may serve as a fulcrum with forced motion. This mechanism explains the clinical symptoms and may lead to damage of the labrum and the adjacent articular cartilage, leading to progressive osteoarthritis [6]. Radiographic evaluation using MRI plays an important role in confirming the diagnosis and estimating prognosis. Thecontinuity of the cortex and medulla of the lesion with that of the native bone is the pathognomonic feature of osteochondroma. MRI is the gold standard investigation of choice to assess the thickness of the cartilage cap covering the exostosis. Irregular cartilage cap with thickness exceeding 15mm have a higher risk of malignant transformation, although it should be borne in mind that younger patients can present with cartilage cap measuring 1–3 cm without signs of malignancy [7, 8]. Resection of osteochondroma of the femoral neck, which frequently involves the anterior, inferior, and posterior aspects of the femoral neck, poses difficulties in choosing an adequate surgical approach to reach the entire lesion. Approaches using hip dislocation have high chances of AVN of femur head after surgery due to damage to the medial circumflex femoral artery supplying the head. Hence, mini-arthrotomy after separating the external rotators was done in this case without dislocating hip. Bottner et al. reported a series of 86 patients to investigate the outcome of surgical excision of osteochondroma [13]. In their series, 93.4% of pre-operative symptoms resolved after surgical excision. Four patients had major complications including one intraoperative fracture of the femoral neck and three peroneal nerve palsies. Local recurrence was observed in 5.8% of cases. Incomplete excision of the lesion and young age at presentation were risk factors for local recurrence [9]. In our case, we did not find local recurrence of the tumor over a follow-up period of 1 year. Other modalities of treatment are arthroscopic excision, mainly for smaller size lesions, and completely intra-articular location such as acetabular osteochondromas and navigation-assisted excision of the osteochondroma. In a case series of seven patients of femoral osteochondroma navigation system was used for excision using anterior (four patients) and posterolateral (three) patients. Computed tomography images of each patient’s proximal femur and a size-matched normal proximal femur were fused on software. The intended resection margins were then plotted and the plan executed using intraoperative navigation guidance [10]. One might need prophylactic fixation using CC screws if fracture of the neck is anticipated after excision of tumor.
A solitary, symptomatic osteochondroma of the proximal femur must be treated surgically, with a detailed pre-operative workup in every case. Surgeons should consider the possibility of intraoperative fracture or chances of damage to the vascular supply of head and post-operative AVN of femur head. Depending on its implantation and extent, en bloc resection of the tumor may be performed through a single wide surgical incision with special curved instruments, without dislocating the hip.
Excision of the proximal femoral osteochondromas can be done without surgical hip dislocation to avoid development of AVN of femur head.
References
- 1.De Souza AM, Júnior RZ. Osteocondroma: Ignore or investigate? Rev Bras Ortop 2014;49:555-64. [Google Scholar]
- 2.Ramos-Pascua LR, Sánchez-Herráeza S, Alonso-Barrioa JA, Alonso-Leónb A. Osteocondromas solitarios del extremo proximal del fémur. Indicación y resultados de la resección en bloque sin luxación de la cadera. Rev Cir Ortop Traumatol 2012;56:24-31. [Google Scholar]
- 3.Porter DE, Benson MK, Hosney GA. The hip in hereditary multiple exostoses. J Bone Joint Surg Br 2001;83:988-95. [Google Scholar]
- 4.Wang SI, Park EH, Yoon SJ, Kim JR. Intra-articular osteochondroma of the posteroinferior femoral neck associated with hip joint osteochondromatosis: A case report. Mol Clin Oncol 2017;7:915-8. [Google Scholar]
- 5.Malagón V. Development of hip dysplasia in hereditary multiple exostosis. J Pediatr Orthop 2001;21:205-11. [Google Scholar]
- 6.Siebenrock K, Ganz R. Osteochondroma of the femoral neck. Clin Orthop Rel Res 2002;394:211-8. [Google Scholar]
- 7.Saglik A, Altay M, Unal VS, Basarir K, Yildiz Y. Manifestations and management of osteochondromas: A retrospective analysis of 382 patients. Acta orthop Belg 2006;72:748-55. [Google Scholar]
- 8.Murphey MD, Choi JJ, Kransdorf MJ, Flemming DJ, Gannon FH. Imaging of osteochondroma: Variants and complications with radiologic pathologic correlation. Radiographics 2000;20:1407-34. [Google Scholar]
- 9.Bottner F, Rodl R, Kordish I, Winklemann W, Gosheger G, Lindner N. Surgical treatment of symptomatic osteochondroma a three-to eight-year follow-up study. J Bone Joint Surg Br 2003;85:1161-5. [Google Scholar]
- 10.Sun Y, Chan C, Niu X. Proximal Femoral Osteochondroma Excision Aided by Computer Navigation: Surgical Technique and Case Series. The 18th Annual Meeting of the International Society for Computer Assisted Orthopaedic Surgery; 2018. p. 193-9. [Google Scholar]











