Excision with ray amputation of the involved metatarsal helps in complete removal of the lesion and helps in early weight-bearing.
Dr. Pranay Kondewar, Department of Orthopaedics, Campus JJ Hospital, Byculla, Mumbai - 400 008, Maharashtra, India. E-mail: pranaypk1@gmail.com
Introduction: The giant cell tumor of bone (GCTB), also known as an osteoclastoma or a myeloid sarcoma, is a benign local aggressive osteolytic bone tumor that primarily affects skeletally mature young adults typically 20–40 years of age. Giant cell tumors (GCTs) are usually solitary tumors and very rarely are found in the metatarsal bones. The characteristic histological appearance of GCT displays a high number of osteoclast-like multinucleated giant cells, which resulted in the classification “osteoclastoma” or “giant cell tumor.”
Case Report: A 38-year-old male presented to the hospital with a firm swelling over the 2nd metatarsal slowly progressing over a period of 4 months, initial screening radiological investigations included X-rays, X-rays showed a tumorous growth involving the shaft of the 2nd metatarsal of the right foot, and the X-rays showed a characteristic soap bubble appearance. Magnetic resonance imaging. On gross assessment, the intraoperative sample showed that the GCTB has a dark brown-to-reddish appearance that is friable in texture. The gold standard for diagnosing a GCT is based on biopsy histopathological findings. The key histomorphologic feature is multinucleated giant cells.
Conclusion: Giant cell tumors are frequently locally aggressive with high recurrence percentage, hence, excision was done. Nowadays, early radiological screening techniques help early detection of such rare occurrence of tumors such as the GCT and appropriate management. In conclusion, the giant cell tumor of the bone is a unique presentation of stromal cell and hematopoietic interaction in the bone.
Keywords: Giant cell tumor, benign tumors of bone, osteoclastoma, metatarsal GCT, ray amputation.
The giant cell tumor of bone (GCTB), also known as an osteoclastoma or a myeloid sarcoma, is a benign local aggressive osteolytic bone tumors that primarily affect skeletally mature young adults typically 20–40 years of age [1]. First documented by Cooper and Travers et al. [2], giant cell tumors of the bone are benign tumors of metaphysis predominantly which have a tendency to undergo aggressive malignant transformation. Giant cell tumor of the bone constitutes approximately 20% of the benign tumors of the bone and 4% of all the tumors of the bone [3]. Most common sites, distal femur and proximal tibia, represent the common locations for giant cell tumors [4, 5]. Giant cell tumors (GCTs) are usually solitary tumors and very rarely are found in the metatarsal bones. Giant cell tumors are mostly seen to occur in the second decade of life, this decade has shown to high incidence of tumors of spine and multicentric tumors [4]. Giant cell tumors get their nomenclature due to numerous multinucleated osteoclast-type giant cells. These similar cells are also seen in other tumorous growth which includes brown tumors associated with hyperparathyroidism, giant cell reparative granuloma, aneurysmal bone cyst, and osteosarcoma. However, the characteristic histological appearance of GCT displays a high number of multinucleated giant cells, along with stromal cells which resulted in the classification “osteoclastoma” or “giant cell tumor.”
A 38-year-old male presented to the hospital with a firm swelling over the 2nd metatarsal slowly progressing over a period of 4 months, during the time of presentation, the patient complained of pain while walking. On examination, the swelling was firm and hard, with deformity present over foot, there was no distal neurovascular deficit (Fig. 1). Blood investigations were within normal limits and infection markers were not raised. Initial screening radiological investigations included X-rays. It showed a tumorous growth involving the shaft of the 2nd metatarsal of the right foot, with a characteristic soap bubble appearance (Fig. 2). Magnetic resonance imaging (MRI) imaging and computerized tomographic (CT) scan done and excision of tumor planned with ray’s amputation of the 2nd metatarsal. MRI is a fairly non-specific modality of treatment, in this case, it was primarily done to assess preoperatively the surrounding soft tissue for better pre-operative planning of the excision. 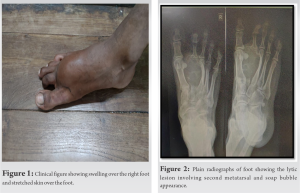
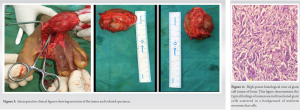
On X-ray, GCTs are lytic/lucent lesions that have an epiphyseal location and grow to the articular surface of the involved bone. Most common sites, distal femur and proximal tibia, represent the common locations for giant cell tumors [5]. The giant cell tumors can show numerous patterns and presentations ranging from small contained lesions with a hard solid soft-tissue involvement to locally aggressive tumors with significant bone loss, cortical loss, pathological fractures, and compression pressure changed affecting the local soft tissue [4, 6]. MRI as an imaging modality to assess the giant cell tumors of bone is very non-specific, the tumors often display reduced imaging in the T1-weighted figures and increased in T2-weighted imaging. Sometimes, gadolinium scan is of particular value to detect the hemosiderin deposition which is frequently found in the giant cell tumors of the bone [7]. On scintigraphic feature of this tumor, shows the “donut sign” which is high intensity radionuclear uptake in the peripheral tissue as a result of hyperemia and photopenia and necrosis in the center of the tumor, however, this is not a finding specific to this tumor. Some surgeon advice in doing a full body PET scan to look for secondary metastasis. The most common presenting symptom of a GCT is pain, these symptoms may vary in accordance to the location of the tumor, the joint involved and the resultant limitations in the range of motion. Patients may even present with pathological fractures when the cortex becomes thing as a result of the lytic bone activity in the weight-bearing bone and radiologically shows areas of ill-defined bone loss. Campanacci et al. described radiographic classification in 1987 which continues to be referenced in clinical practice [8]. This classification system differentiates lesions based on their amount of bone destruction. Grade 1 tumors have well-marginated (geographic), defined borders (the least common presentation) and a subsequent report has indicated that local recurrence in these lesions is lower than those without the sclerosis. Grade 2 lesions have a poorly defined tumor borders but remained contained within the bone (this category is subdivided into 2-A lesions without fractures and 2-B lesions with a pathological fracture) and Grade 3 lesions being non-geographic with associated cortical destruction and soft-tissue extension. The majority of the GCTB lesion fit into the latter two grades. The Campanacci system appears to be helpful when utilized clinically to help determine treatment options. Excision (curettage) is the most common surgical treatment aimed at removing the tumor (intralesional resection), while preserving as much as bone as possible. Complete tumor removal is the most important aspect of this treatment and should be done through an adequate cortical window that allows visualization of the entire defect. This case the metatarsal is a rare location, the best plan was to perform a Ray’s amputation of the 2nd toe. Prashant et al. reported metatarsal GCT case which was managed with excision and reconstruction using fibula autograft with good outcome; they had lesion involving first metatarsal, fibular graft was taken and was inserted into the troughs created in medial cuneiform and proximal phalanx and fixed with K-wire, both proximally and distally [9]. Minhas et al. studied data of 25 years and found 240 cases of giant cell tumor, out of which only seven were affecting the metatarsals. Four GCTs in the 1st metatarsal and one in the 2nd metatarsal were in Stage 3 and were treated by en bloc resection and reconstruction with free fibular graft. Fibular graft was held with intramedullary K-wire. Rest of the tumors in all metatarsals were Stage 2 and were treated by curettage and autologous cancellous bone grafting. At 1 year follow-up, there was no recurrence [10].
Metatarsal giant cell tumors are very rare and less data available on management. They have high recurrence percentage, hence, excision was done which gave good clinical outcome and there was no local recurrence of the tumor.
Rays amputation with complete excision of tumor mass gives good clinical outcome without chances of recurrence.
References
- 1.Wülling M, Engels C, Jesse N, Werner M, Delling G, Kaiser E. The nature of giant cell tumor of bone. J Cancer Res Clin Oncol 2001;127:467-74. [Google Scholar]
- 2.Cooper AS, Travers B. Surgical Essays. London: Cox Longman and Co.; 1818. [Google Scholar]
- 3.Larsson SE, Lorentzon R, Boquist L. Giant-cell tumor of bone. A demographic, clinical, and histopathological study of all cases re-corded in the Swedish cancer registry for the years 1958 through 1968. J Bone Joint Surg Am 1975;57:167-73. [Google Scholar]
- 4.Werner M. Giant cell tumour of bone: Morphological, biological and histogenetical aspects. Int Orthop 2006;30:484-9. [Google Scholar]
- 5.Montgomery C, Couch C, Emory CL, Nicholas R. Giant cell tumor of bone: Review of current literature, evaluation, and treatment options. J Knee Surg 2019;32:331-6. [Google Scholar]
- 6.Raskin KA, Schwab JH, Mankin HJ, Springfield DS, Hornicek FJ. Giant cell tumor of bone. J Am Acad Orthop Surg 2013;21:118-26. [Google Scholar]
- 7.Mallick A, Chawla SP. Giant cell tumor of bone: An update. Curr Oncol Rep 2021;23:51. [Google Scholar]
- 8.Campanacci M, Baldini N, Boriani S, Sudanese A. Giant cell tumor of bone. J Bone Joint Surg Am 1987;69:106-14. [Google Scholar]
- 9.Prashant K, Bhattacharyya TD, Frank H, Ram P. An unusual case of giant cell tumor of first metatarsal: A rare case report and review of literature. J Orthop Case Rep 2016;6:3-6. [Google Scholar]
- 10.Minhas MS, Khan KM, Muzzammil M. Giant cell tumour of foot bones - 25 years experience in a tertiary care hospital. J Pak Med Assoc 2016;65:S67-71. [Google Scholar]











