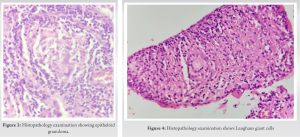
The need of early diagnosis of Tubercular Tenosynovitis is emphasised in this article but it delayed due to the condition's lack of clinical awareness and similarities to numerous other illnesses and also hallmarking the importance of Histopathological examination for its confirmation.
Dr. B Vijitha, Department of Orthopedics, Viswabharathi Medical College and Hospital, Kurnool, Andhra Pradesh, India. E-mail: vijithadiva3@gmail.com
Introduction: Compound dorsal ganglion of tubercular etiology involving the dorsum aspect of wrist is a rare entity. It is very rarely seen lately, due to early diagnosis and effective treatment regimen and this case is probably the first to be reported involving the dorsum aspect of wrist.
Case Report: This case report presents a 54-year-old male patient presented to us complaints of swelling and pain in dorsum of hand and wrist for 6 months. On examination, we found multiple swellings on Rt. dorsum of hand and dorsal aspect of wrist restriction of movements at wrist. After thorough clinical and radiological evaluation, patient has been posted for excision biopsy and confirmed as compound dorsal ganglion.
Conclusion: Compound dorsal ganglion is a disease with great diagnostic challenge due to its masquerade clinical presentation and confirmed by histopathological examination. Early diagnosis, complete debulking, and antitubercular therapy prevent further spread of disease and improves the patient functionally.
Keywords: Compound dorsal ganglion, histopathology, tuberculosis, tenosynovitis.
Compound dorsal ganglion is the medical term for tuberculous tenosynovitis of the extensor tendons of the forearm, hands, and fingers [1]. Rarely, a bursa or synovial sheath will develop isolated tubercular illness; nevertheless, any bursa or synovial sheath may be affected. Although it is a rare illness, chronic tendon sheath infection is primarily caused by tuberculous tenosynovitis. Direct inoculation or hematogenous spread are the two possible infection routes [2]. The diagnosis of compound dorsal ganglion is a significant problem due to its variable presentation and similarities to other conditions that are identical [3, 4]. The condition must be identified early since it might advance and cause severe damage to the structures around the wrist.
A 54-year-old male presented to our hospital with complaints of pain and progressive multiple swellings in the right hand and wrist for the past 6 months. No history of trauma. No loss of appetite and weight loss. There was no contact history of tuberculosis. On local examination, one swelling of size 5×4×2 cm presents on dorsum of hand (Fig. 1). Two swellings of size 2×1×1cm present over dorsolateral aspect of wrist (Fig. 2) with positive cross fluctuation test. 
In India, tuberculosis is pervasive and effects numerous organ systems. The CNS, lymph nodes, genitourinary tract, and musculoskeletal system, including bursa and tendons, are the extrapulmonary sites most frequently affected, accounting for 1.3% of all cases of tuberculosis [5]. An uncommon instance of extrapulmonary tuberculosis is tuberculous tenosynovitis. By direct hematogenous route from a focal focus in the lung or by direct inoculation from the underlying bone and joint disease, the synovial or bursal sheath becomes contaminated. Lower limbs are less likely to be effected than the upper limbs. The flexor tendons of the dominant limb’s wrist and hand are more usually affected in the upper limb than the extensor side [6]. Compound dorsal ganglion is the name for tuberculous tenosynovitis that affects the common sheath of the forearm extensor tendons. In 1923 [8], Kanavel published the first comprehensive investigation of tuberculous tenosynovitis that included the three conventional histological phases. The duration of the illness, patient resistance, and bacterial virulence is the three variables that determine the stages. The tendon sheaths first experience inflammation, which is followed by obliteration and fibrosis. In the second stage, the fibrinous tubercles or masses created by the caseous necrosis are visible as the rice body or melon seed body. Third stage is brought on by severe caseation and tendon sheath rupture. Tendon ruptures were documented in 10 out of the 21 instances in Kanavel’s study. Our case is an example of tuberculous tenosynovitis in its second stage. A clinical diagnosis and subsequent treatment are frequently delayed due to the large variety of differential diagnoses and inadequate clinical awareness, which increases the risk of consequences. Inflammatory arthritis (rheumatoid arthritis and gouty arthritis), sarcoidosis, infectious (pyogenic infections, foreign body tenosynovitis, and fungal granuloma), and other tendon sheath lesions are among the differential diagnoses for compound dorsal ganglion (pigmented villonodular synovitis, giant cell tumor, amyloidosis, and synovial chondromatosis). By doing an open excision biopsy, histological analysis, and mycobacterial culture on the specimen, the diagnosis can be verified. The sensitivity of synovial fluid AFB staining (32%), culture (80%), histology (65%), and PCR (63%) were reported by Lertsrisatit et al. They also came to the conclusion that PCR can be employed as an early diagnostic tool [9, 10]. In our case report, a 54-year-old male presented with pathology in Rt. upper limb with varied presentation potentiated the challenge of diagnosis. His clinical presentation was distinctive, patient presented with multiple swellings in dorsum of hand and wrist rather volar aspect, involvement of extensor compartment rather flexor compartment complicated our diagnosis. Then, the patient was planned for excision biopsy which revealed the suspicion of diagnosis and strong positivity of Mantoux test confirmed the diagnosis of compound dorsal ganglion. Early diagnosis with combined surgical and medical therapies which include excision of infected tissue, tenosynovectomy followed by antitubercular therapy for 6–9 months yields better prognosis and prevents recurrence of disease.
It is possible for tuberculosis to look like a wrist ganglion. One uncommon manifestation of extra pulmonary tuberculosis is compound dorsal ganglion. In developing nations, it is important to keep in mind that wrist tenosynovitis that is persistent might be from tuberculous origin. To get a favorable functional outcome as well as to prevent complications and a recurrence of the disease, the time between presentation, diagnosis, and care should be kept to a minimum. Therefore, the peculiarity of this case report is highlighted by its varied clinical presentation, extensor compartment involvement, well-timed excisional biopsy, and early commencement of antitubercular therapy. These factors also show the significance of the compound dorsal ganglion.
This is a rare case report of compound dorsal ganglion of Rt. wrist. This case report highlights the varied clinical presentation of the patient with no significant diagnostic findings. The unique feature of this report highlights the involvement of extensor compartment of wrist and hand which usually involves flexor compartment. Therefore, the diagnosis is done by histopathological examination. Early diagnosis, complete debulking, and antitubercular therapy prevents further spread of disease and improves the patient functionally.
References
- 1.Williamson JC. Chronic tenosynovitis of extensors of hand and fingers (“compound dorsal ganglion”). Ann Phys Med 1961;6:109-15. [Google Scholar]
- 2.Ahmad J, Shrivastava VK, Khanna M, Ayaz A. Tubercular compound Dorsal ganglion-a review. Indian J Orthop Rheumatol 2019;5:22-5. [Google Scholar]
- 3.Bayram S, Ersen A, Altan M, Durmaz H. Tuberculosis tenosynovitis with multiplerice bodies of the flexor tendons in the wrist: A report. Int J Surg Case Rep 2016;27:129-32. [Google Scholar]
- 4.Stirrat CR. Treatment of tenosynovitis in rheumatoid arthritis. Hand Clin 1989;5:169-75. [Google Scholar]
- 5.Higuchi S, Ishihara S, Kobayashi H, Arai T. A mass lesion of the wrist: A rare manifestation of tuberculosis. Intern Med 2008;47:313-6. [Google Scholar]
- 6.Shen PH, Chu CM, Huang GS, Wu SS, Lee CH. Tuberculous tenosynovitis of the flexor tendons of the wrist and hand. J Med Sci 2002;22:227-30. [Google Scholar]
- 7.Tuli SM. Tuberculosis of the Skeletal System. Delhi: Jaypee Brothers; 2021. [Google Scholar]
- 8.Kanavel AB. Tuberculous tenosynovitis of the hand: A report of fourteen cases of tuberculous tenosynovitis. Surg Gynecol Obstet 1923;37:635-47. [Google Scholar]
- 9.Tyllianakis M, Kasimatis G, Athanaselis S, Melachrinou M. Rice body formation and tenosynovitis of the wrist: A case report. J Orthop Surg 2006;14:208-11. [Google Scholar]
- 10.Padmanabhan K, Palanisamy P, Muthusamy MP. Compound Dorsal ganglion associated with tuberculous arthritis of wrist causing compression of the median and ulnar nerves: Management. J Indian Orthop Rheumatol Assoc 2018;4:28-33. [Google Scholar]