Repeated diabetic ulcers may mimic the effect of trauma in causing myositis ossificans and regardless of disease rarity this disease should be considered.
Ms. Prabodhinee Dhiren Jogiya, Department of Life Sciences, University of Leicester, Leicester, England. E-mail: pdj4@student.le.ac.uk
Introduction: Myositis ossificans (MO) is a disease with self-limiting, benign ossifying lesions. MO traumatica is most common cause and occurs after blunt trauma to muscle tissue and the most common site of occurrence is the anterior thigh often developing after an intramuscular hematoma. The pathophysiology of MO is not well understood. The association of myositis and diabetes is quite rare.
Case Report: A 57-year-old male presented with a discharging ulcer on the right lateral lower leg. A radiograph was carried out to ascertain the degree of bone involvement. However, the X-ray showed calcifications. Ultrasound, magnetic resonance imaging (MRI) and X-ray imaging were used to exclude malignant disorders such as osteomyelitis or osteosarcoma. The diagnosis of myositis ossificans was confirmed with MRI. As the patient had a background of diabetes, this could have led to MO as a result of the macrovascular complication of a discharging ulcer; hence, diabetes could be considered a risk factor for the disease.
Conclusion:The reader may appreciate that diabetic patients may present with MO and that repeated discharging ulcers may imitate the effects of physical trauma on calcifications. The specific take home message is that regardless of the apparent rarity of a disease and subversion to typical clinical presentation, it should still be considered. Furthermore, the exclusion of severe and malignant diseases which benign diseases may mimic is of utmost importance to correctly manage patients.
Keywords: Myositis ossificans, diabetes.
Myositis ossificans (MO) is a rare pathological condition characterized by formation of bony tissue from muscles or soft tissues usually after trauma; there are many types of MO. In this paper, when MO is referred to by the author, this highlights the most common version of the disease which represents almost 60–75% of the cases1. This type of MO, which is acquired with trauma, can also be referred to as MO Traumatica. As the overall number of people living with diabetes is at 3.8 million and as a majority of these are living with type 2 diabetes in particular, this condition is highly significant2 . Hence, any potential link between diabetes and MO is extremely important to discuss. Whilst this case is clearly a rare occurrence, the features of how the patient presented are of clinical relevance as they may help to probe a health-care professional to consider MO which could lead to improvement of any future management of a diabetic patient. This is especially important, as repeated ulceration in lower limbs is a very common macrovascular complication of diabetes and this was the key presenting complaint from our patient. We present this case report of an incidental finding of MO in an elderly type 2 diabetic male in the same area as a discharging diabetic ulcer. The authors have discussed the symptoms, differentials, and management plan of this patient below. The current literature was reviewed and studied for the potential pathophysiology of MO and if there is any previous link that the calcifications may have to diabetes. The significance of following typical textbook presentations alone and how this patient did not follow this clinical presentation was also discussed.
A 57-year-old male presented with a discharging ulcer on the lateral aspect of the right lower leg. He had a medical history of type 2 diabetes mellitus but was otherwise fit and well with no other systemic symptoms such as fever or malaise. It was initially thought that the patient may have osteomyelitis of the right tibia and fibula due to extensive past surgical debridement for chronic ulcers; this was investigated initially using an X-ray to see if any signs of bony infection were present. The X-ray image of the right lower lateral leg is shown below in Fig. 1. This showed calcifications which were suggestive of MO but may also have been indicative of more malignant disorders such as osteomyelitis or osteosarcoma. 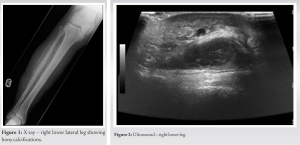
The calcifications seen on the X-ray in Fig. 1 made it difficult to rule out chronic bony infective changes in the right tibia and fibula, and hence, further investigations and imagery were needed to be carried out. After the radiograph, the patient had an ultrasound and an magnetic resonance imaging (MRI) scan which are both shown in Fig. 2–4 below, respectively.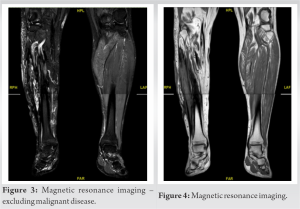
The ultrasound scan below in Fig. 2 showed the dysplastic changes of the muscle to bone, which again was a positive finding for MO but could not accurately exclude more serious malignant diagnoses such as those mentioned above. The MRI scan of the right lower leg definitively excluded the diagnoses of more serious diseases such as osteomyelitis or osteosarcoma as there were no further positive signs for malignant disease. This removed the need for any further investigations, and hence, there was no longer a need for considering more aggressive management options such as chemotherapy or radiation. The MRI concluded that there were indeed changes suggestive of MO alone. The patient was, thus, managed with surgical debridement of the ulcers, to aid with the presenting complaint of the discharging ulcer. For the management of the incidental finding of MO, the patient was reassured that there was no malignant nature to the calcifications, and a conservative approach to management was taken. The patient had regular dressings before being discharged home with analgesia to take when required. The patient was followed up 3 months ago and is fit, well, and back to work, with no more new investigations required and no new presenting complaints.
MO is the abnormal calcification or the heterotopic formation of bone in striated muscle and soft tissues.1 These lesions are often described as “non-touch” as often repeated trauma can inadvertently worsen the symptoms. This disease, especially the MO traumatica version of this disease, can usually present following trauma as a growing mass associated with pain and tenderness in the larger muscles of the lower or upper limbs. In particular, often in the quadricep muscles.3 Patients normally present at a younger age and often these patients are athletes who have suffered trauma multiple times to the long limbs4 . The nature of athlete injury leads to a patient more likely to suffer from MO. As athletes often suffer from repetitive trauma to long limbs, this can cause dysplastic changes to the muscle which forms bony calcifications. On imagery and histologically myositis, can be similar to osteomyelitis or osteosarcoma5 The changes seen in diseases such as osteosarcoma are osteoblastic, fibroblastic, and chondroblastic6 Due to these similarities, malignant diagnoses must be excluded before an accurate diagnosis of MO can be delivered. Overall, the location of the calcifications, the age, and the history of our patient was of clinical significance as it subverted common clinical presentation. Clinically, our patient was a 57-year-old diabetic male who presented with a non-healing surgical ulcer of the lateral right lower tibia. The average age of patients with MO, as described by Nuovo et al, could be considered to be 23 years old. Our patient however subverted this average “young athlete” patient who is prone to injury and trauma of muscle4 Preceding trauma is also a known risk factor for developing MO often linking to the pathophysiology of the disease, however, clearly the absence of trauma does not rule out this diagnosis, as observed in this patient. This, therefore, highlights the importance of having a low sensitivity for this disease regardless of a negative history of trauma7 Our patient did not have the typical history of trauma, he instead had a diabetic ulcer. This made clinicians suspicious of a more aggressive malignant disease such as osteomyelitis or osteosarcoma, especially after the X-ray findings. Radiographically, when MRI findings show aggressiveness or a lack of a clear diagnosis, this can be suggestive of malignancy8. In these cases, where a diagnosis is uncertain, a biopsy is required to ascertain the most accurate diagnosis. When considering the MRI findings of MO, the extent of the disease determines the radiological appearance. For example, taking the earliest stage of T1, these can present as “ill-defined” areas which are a typical feature of malignant disease9. Radiographically, even though an MRI is the gold standard for MO, often initial investigations include X-ray of the affected area9. In MO, this shows muscle calcification with lucent center, usually within 2–6 weeks of trauma. Conventional treatment includes NSAIDs, rest, ice, compression, and elevation and if severe pain persists, then, patients could opt for surgical excision of the calcified muscle10 The exact pathophysiology of MO is not well known11. However, on a cellular level, it is perhaps an abnormal response of stem cells in the bone to injury or inflammation12. In particular, stem cells can undergo metaplastic changes and the formation of chondrocytes and osteoblasts can result in bone formation in soft tissues.13 Our patient, however, presented with calcification lateral to the right tibia and fibula in the area of a diabetic ulcer. This may be significant as this perhaps has caused the MO, especially as this may have caused dysregulation in the stem cells due to the underlying injury and inflammation14. This is an extremely rare presentation and the authors have found very little research displaying myositis in diabetic patients. Sharma et al. presented a case series of three patients with MO in the diabetic foot and showed how important the knowledge of a link was, especially to management of diabetic patient by health-care professionals15 Perhaps, the inflammation from the repeated ulceration and poor healing could have caused a similar metaplastic change of the stem cells that are associated with the pathophysiology of MO and, hence, contributed to the ossification in our patient. Once the ulcer was managed, in this case through surgical debridement, this may have reduced the inflammatory processes. Reducing the inflammation through debridement should in-turn result in less insult and dysregulation to the muscle and stem cells, respectively, and ultimately reduce or halt the progression of the ossification.
This case shows a rare disease with an even rarer presentation. It is often easy to ignore rare diagnoses due to a patient not fitting the demographic mold, especially as pattern recognition is so key to medical practice. In this case, health-care professionals dealing with diabetic patients should be aware of potential myositis in diabetic patients. As well as this, a clear theme in the literature is to ensure accurate diagnosis through imagery, to exclude potentially malignant diseases. This can help to prevent mismanagement of the patient and prevent misinformation shared to the patient and often the wrong diagnosis being made.
The clear clinical message for this case report is that MO is an important differential to consider, regardless of patient profile not fitting with the standard textbook clinical presentation, especially if the patient is diabetic.
References
- 1.Marques JP, Pinheiro JP, Costa SJ, Moura D. Myositis ossificans of the quadriceps femoris in a soccer player. BMJ Case Rep 2015;2015:bcr2015210545. [Google Scholar]
- 2.Smith J. Health Matters: Preventing Type 2 Diabetes. Health Matters; 2018. Available from: https://www.publichealthmatters.blog.gov.uk/2018/05/24/health-matters-preventing-type-2-diabetes (Last accessed: 17/07/21) [Google Scholar]
- 3.Saber M, Farooq S. Myositis Ossificans. Radiopaedia Available from: https://www.radiopaedia.org/ articles/ myositis-ossificans-1?lang=gb (Last accessed: 17/07/21) [Google Scholar]
- 4.Nuovo M, Norman A, Chumas J, Ackerman LV. Myositis ossificans with atypical clinical, radiographic, or pathologic findings: A review of 23 cases. Skeletal Radiol 1992;21:87-101. [Google Scholar]
- 5.Moser T, Ehlinger M, Bouaziz MC, Ladeb MF, Durckel J, Dosch JC. Pitfalls in osteoarticular imaging: How to distinguish bone infection from tumour? Diagn Interv Imaging 2012;93:351-9. [Google Scholar]
- 6.Medrado AR, Almeida E, Mascarenhas BA, Cerqueira A. Chondroblastic osteosarcoma. J Oral Maxillofac Pathol 2014;18:464-8. [Google Scholar]
- 7.Aneiros-Fernandez J, Caba-Molina M, Arias-Santiago S, Ovalle F, Hernandez-Cortes P, Aneiros-Cachaza J. Myositis ossificans circumscripta without history of trauma. J Clin Med Res 2010;2:142-4. [Google Scholar]
- 8.Nascimento D, Suchard G, Hatem M, de Abreu A. The role of magnetic resonance imaging in the evaluation of bone tumours and tumour-like lesions. Insights Imaging 2014;5:419-40. [Google Scholar]
- 9.Lacout A, Marcy PY, Carlier RY, Jarraya M, Thariat J. Myositis ossificans imaging: Keys to successful diagnosis. Indian J Radiol Imaging 2012;22:35-9. [Google Scholar]
- 10.Galan N, Morrison W. Myositis Ossificans: Causes, Risk Factors and Treatment. Brighton, East Sussex: Medical News Today; 2018. Available from: https://www.medicalnewstoday.com /articles/320718 (Last accessed: 17/07/21) [Google Scholar]
- 11.Devilbiss Z, Hess M, Ho GW. Myositis ossificans in sport: A review. Curr Sports Med Rep 2018;17:290-5. [Google Scholar]
- 12.Lees-Shepard JB, Goldhamer DJ. Stem cells and heterotopic ossification: Lessons from animal models. Bone 2018;109:178-86. [Google Scholar]
- 13.Walczak BE, Johnson CN, Howe BM. Myositis ossificans. J Am Acad Orthop Surg 2015;23:612-22. [Google Scholar]
- 14.Kan L, Liu Y, McGuire TL, Berger DM, Awatramani RB, Dymecki SM, et al. Dysregulation of local stem/progenitor cells as a common cellular mechanism for heterotopic ossification. Stem Cells 2009;27:150-6. [Google Scholar]
- 15.Sharma V, Sharma D, Dinar H, Dhatariya KK. Myositis ossificans in the diabetic foot: A review of the literature with an illustrative case series. JRSM Open 2019;10:2054270419885231. [Google Scholar]











