The first case of an asymmetric bilateral inveterate shoulder dislocation in a young patient, emphasizing the importance of early recognition and diagnosis and the need for clinicians to consider this condition and determine a timely treatment strategy. Despite the uncertain prognosis of a bilateral chronic shoulder dislocation functional results, the surgeon must take into consideration the patient’s age, functional demand, and expectations to define the best treatment strategy.
Dr. Sara Elisa Diniz, Department of Orthopaedics, Centro Hospitalar Universitário do Porto-Hospital de Santo António, Largo Prof. Abel Salazar, 4099001 Porto. Portugal. E-mail: saradiniz4@gmail.com
Introduction: Chronic shoulder dislocations are infrequent and can be easily overlooked unless a carefully clinical history, physical examination, and radiographic evaluation are undertaken. Bilateral simultaneous instability is almost pathognomonic for a convulsive disorder. To the best of our knowledge, we describe the first case of asymmetric bilateral chronic dislocation.
Case Report: A 34-year-old male patient with a history of epilepsy and schizophrenia and multiple seizure episodes, suffered a bilateral asymmetric shoulder dislocation. Radiological examination revealed a posterior shoulder dislocation of the right shoulder with a severe reverse Hill-Sachs lesion comprising more than 50% of the humeral head surface, while on the left shoulder, a chronic anterior shoulder dislocation with a Hill-Sachs lesion of moderate dimension. On the right shoulder, a hemiarthroplasty was performed, and on the left, a stabilization with Remplissage Technique, subscapularis plication, and temporary trans-articular Steinmann pin fixation was done. After bilateral rehabilitation, the patient showed residual pain in the left shoulder and slight range of motion limitation. There were no new episodes of shoulder instability.
Conclusion: Our aim is to emphasize the importance of being alert to flag patients and make a prompt and accurate diagnosis of acute shoulder instability episodes, to avoid unnecessary morbidity, as well as of a high index of suspicion when a history of seizures is present. Despite the uncertain prognosis of a bilateral chronic shoulder dislocation functional results, the surgeon must take into consideration the patient’s age, functional demand, and expectations to define the best treatment strategy.
Keywords: Chronic bilateral dislocation, anterior shoulder dislocation, posterior shoulder dislocation, asymmetric dislocation.
The shoulder is the most frequently dislocated joint accounting for 85% of all dislocations [1]. Glenohumeral dislocations are more than twice as common in male than female patients and occur most often in the third decade of life [2]. While dislocations of the shoulder can occur in any direction, anterior dislocation is the most common, accounting for up to 95% [1]. Conversely, posterior instability is rare (4%), and the diagnosis can be difficult. Often, detection occurs only once the injury has become chronic and the joint is irreducible [3]. This type of injury can be easily undiagnosed unless a carefully clinical history, physical examination, and radiographic evaluation are undertaken [4]. Although the chronicity of the injury is one of the most important factors regarding prognosis, there is still no consensus on when to consider a shoulder dislocation a chronic injury. Twenty-four hours, 3 weeks and 1 month have all been used as a criteria to determine a dislocation as chronic [4, 5, 6]. A recent study defines chronic dislocation as a diagnosis within 21 days of the original trauma [7]. Bilateral shoulder dislocations can be either anterior or posterior and are well described since Cooper, in 1839, reported the first cases of bilateral symmetric posterior shoulder dislocations [8]. The literature seems to demonstrate that bilateral simultaneous instability is almost pathognomonic of a convulsive disorder [9]. However, up to our knowledge, this is the first description of a case of asymmetric bilateral chronic dislocation in a young male patient with history of epileptic seizures. The optimal treatment is yet to be established. Our goal is to discuss our choice of management, as well as the wide range of the treatment modalities described in the literature.
A 34-year-old male patient with diagnosis of epilepsy and schizophrenia, with a history of multiple seizure episodes and compulsive hospitalizations, suffered a posterior right shoulder dislocation during a seizure (Fig. 1).


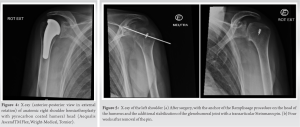
There is no agreement on a definition for chronic glenohumeral dislocation. Despite other timings described in the literature [4, 5, 6], after 3 weeks is the more consensual timing [10]. Shoulder dislocations are rising among the elderly population due to increased longevity, and its chronic presentation is mostly seen in elderly and mentally disabled patients [11]. Bilateral posterior shoulder dislocation is the most common. It happens following unbalanced muscle contractions such as those caused by electric shock, epileptic seizure, and hypoglycemia [1, 3, 4, 6, 8, 12]. External rotators of the humerus are weaker and overpowered by the stronger internal rotators, resulting in adduction and internal rotation with consequent posterior dislocation [1, 12]. Bilateral anterior shoulder dislocation usually results from a traumatic origin and it is rarely seen [1, 6, 12]. The arm usually extends and abducts, with the coracoacromial arch and rotator may cause subscapularis ruptures, labrum lesions, glenoid bone deficiencies, or associated defects on the posterolateral aspect of the humeral head. Concomitant fracture of the greater tuberosity occurs in 15% [1, 4]. On the other hand, posterior dislocations are associated with posterior labrum lesions, glenoid bone defects, and anteromedial humeral head injuries [4]. The degree of these changes determines the degree of instability. These defects must be detected and studied to plan appropriate treatment [5], through X-ray, CT scan and/or MRI [12]. Articular deterioration happens over time when the joint is dislocated. Softening of the articular cartilage, humeral head osteoporosis, soft-tissue contractures, and scarring adhesions of the neurovascular structures all start to develop [1, 4]. As the duration of dislocation lengthens, patients suffer from chronic pain, stiffness, disability, and decreased ROM [3]. Paradoxically, as time passes, patients may evolve to only a mild discomfort and ROM limitation may gradually improve due to functional adaptation [10, 12]. O’Connor-Read et al. [12] described the first case of posterior shoulder dislocation to be missed on initial examination. Misdiagnosis rates were reported to be in the range of 50–80% [13]. This reinforces the need for a careful history, clinical examination, and radiographic evaluation in case of suspicion. In our case, there was an initial diagnosis and treatment of the right posterior shoulder dislocation in the context of an epileptic seizure. We believe that he developed anterior left instability due to additional convulsive episodes. The delayed of diagnosis of bilateral chronic asymmetric shoulder dislocation was probably due to his unstable mental status, which is often compromised in patients with significant psychiatric conditions [14]. Successful management of chronic glenohumeral dislocation is related to the duration of dislocation, the degree of soft-tissue and bone changes, the patient’s age, and compliance with a rehabilitation program [4, 12]. A variety of options exist, including conservative treatment, close reduction, open reduction with tendon and bone transfers, osteotomies of the humerus, allograft, and arthroplasty. However, treatment choice also highly depends on the experience of the surgeon [4, 5, 13, 14]. Success in reducing the joint by closed manipulation diminishes over time. Iatrogenic complications such as a fracture or neurovascular damage further limit the choice of treatment [1, 15]. Lasanianos and Mouzopoulos [1], as well as Goga [16], suggest that closed reduction of a chronic shoulder dislocation should be tried only up to 6 weeks post-injury. The first surgery was on the right shoulder (posterior shoulder dislocation), because it was the most painful. One year after the first event, an X-ray showed more than 50% of anteromedial humeral head fracture impaction. Reverse Hill-Sachs lesions are reported to occur in 40– 90% of patients with an initial posterior dislocation [13]. Arthroplasty is used to treat dislocations associated with a large humeral head defect or associated with deformity or osteoarthritis [11, 13, 14, 15], and in this particular case, an important defect was found. Gavriilidis et al. [14] reported reliable results when choosing shoulder arthroplasty in cases of more than 45% involvement of the articular surface of the humeral head. Hemiarthroplasty was chosen instead of total arthroplasty based on the patient’s age, the intrinsic risk of wear and loosening, glenoid bone stock erosion, and the need for revision surgery. However, some other alternatives could be reasoned [14]. With smaller defects (25–45%), joint protective methods such as bone grafting, the McLaughlin procedure (by tenotomizing subscapularis tendon and burying it into the defective area), or the modification technique of the McLaughlin operation (by osteotomizing the lesser tuberosity with the attached subscapularis tendon and fixing it to the defective area) would be preferable [15, 17, 18, 19]. Thereafter, the left shoulder (anterior) dislocation was treated. There is scarce literature related to chronic unreducible anterior shoulder dislocation: Minimally invasive repair (arthroscopic Bankart and Remplissage Technique), open reduction with internal fixation, anterior stabilization with tendon transfer (e.g., Infraspinatus), allograft reconstruction, and articular replacement are all described [6, 20]. The Bristow-Latarjet procedure was excluded, once an important coracoid deficiency was found. Hill-Sachs lesions and glenoid bone fractures have a high incidence in epileptic patients and are determining factors in glenohumeral instability in patients with seizures [21, 22] A Hill-Sachs lesion was present with a 25% of anteroinferior glenoid bone deficiency. A Remplissage Technique and a subscapularis plication were performed. Nevertheless, shoulder instability persisted and it was necessary to temporarily fix the glenohumeral joint with a transarticular Steinmann pin. The patient evolved favorably, besides residual pain and ROM limitations on the left side. The functional outcomes depend mainly on the duration of the dislocation and the extent of the articular injury. A careful articular reconstruction is advised to diminish recurrence rates. When reconstruction is not possible, arthroplasty procedures can be considered, but the clinical outcomes are not well-known since the number of studies and patients is scarce [3].
A rare case of an asymmetric bilateral chronic shoulder dislocation in a young patient is presented. To the best of our knowledge, the first case described in the literature. There is still insufficient evidence in the literature about the best surgical approach to a chronic shoulder dislocation, especially if anterior, which is typically more difficult to treat. Our aim is to emphasize the importance of being alert to flag patients and make a prompt and accurate diagnosis of acute shoulder instability episodes, to avoid unnecessary morbidity, as well as of a high index of suspicion when a history of seizures is present. Despite the uncertain prognosis of a bilateral chronic shoulder dislocation functional results, the surgeon must take into consideration the patient’s age, functional demand, and expectations to define the best treatment strategy. Despite uncertainty in prognosis of a bilateral chronic shoulder dislocation, and despite the need for good compliance to anticonvulsive medication in this population, our case highlights that a satisfactory clinical outcome is possible.
Up to our knowledge, we describe the first case of an asymmetric bilateral inveterate shoulder dislocation in a young patient, emphasizing the importance of early recognition and diagnosis and the need for clinicians to consider this condition and determine a timely treatment strategy.
References
- 1.Lasanianos N, Mouzopoulos G. An undiagnosed bilateral anterior shoulder dislocation after a seizure: A case report. Cases J 2008;1:342. [Google Scholar]
- 2.Zacchilli MA, Owens BD. Epidemiology of shoulder dislocations presenting to emergency departments in the United States. J Bone Joint Surg Am 2010;92:542-9. [Google Scholar]
- 3.Aydin N, Kayaalp ME, Asansu M, Karaismailoglu B. Treatment options for locked posterior shoulder dislocations and clinical outcomes. EFORT Open Rev 2019;4:194-200. [Google Scholar]
- 4.Shajpal DT, Zuckerman JD. Chronic glenohumeral dislocation. J Am Acad Orthop Surg 2008;16:385-98. [Google Scholar]
- 5.Rowe CR, Zarins B. Chronic unreduced dislocations of the shoulder. J Bone Joint Surg Am 1982;64:494-505. [Google Scholar]
- 6.El Rassi G, Hijjawi A, Matta J, Fahs S, Khair OA. Bilateral locked anterior shoulder dislocation in a bench-pressing athlete: Case report. Arch Orthop Trauma Surg 2015;135:747-9. [Google Scholar]
- 7.Diallo M, Soulama M, Kaboré DS, Dakouré PW, Liverneaux P. Bilateral anterior shoulder dislocations: A review of two cases and the relevant literature. Clin Case Rep 2020;8:3379-88. [Google Scholar]
- 8.Cooper SA. A Treatise on Dislocations, and on Fractures of the Joints. Boston, MA: Wells and Lilly; 1825. [Google Scholar]
- 9.Shaw JL. Bilateral posterior fracture-dislocation of the shoulder and other trauma caused by convulsive seizures. J Bone Joint Surg Am 1971;53:1437-40. [Google Scholar]
- 10.Thomas T, Noel E, Bouvier M. Pitfall of stiff shoulder: Inveterated posterior dislocation. Clin Rheumatol 1995;14:467-70. [Google Scholar]
- 11.Chung H, Yoon YS, Shin JS, Shin JJ, Kim D. Chronic irreducible anterior dislocation of the shoulder without significant functional deficit. Clin Orthop Surg 2016;8:333-8. [Google Scholar]
- 12.Connor-Read L, Bloch B, Brownlow H. A missed orthopaedic injury following a seizure: A case report. J Med Case Rep 2007;10:20. [Google Scholar]
- 13.Basal O, Dincer R, Turk B. Locked posterior dislocation of the shoulder: A systematic review. EFORT Open Rev 2018;3:15-23. [Google Scholar]
- 14.Gavriilidis I, Magosch P, Lichtenberg S, Habermeyer P, Kircher J. Chronic locked posterior shoulder dislocation with severe head involvement. Int Orthop 2009;34:79-84. [Google Scholar]
- 15.Aksekili MA, Uğurlu M, Işık Ç, Yüksel K, Biçici V, Bozkurt M. Posterior bone block of chronic locked posterior shoulder dislocations with glenoid augmentation: A retrospective evaluation of ten shoulders. Int Orthop 2016;40:813-20. [Google Scholar]
- 16.Goga IE. Chronic shoulder dislocations. J Shoulder Elbow Surg 2003;12:446-50. [Google Scholar]
- 17.McLaughlin HL. Locked posterior subluxation of the shoulder: Diagnosis and treatment. Surg Clin North Am 1963;43:1621-2. [Google Scholar]
- 18.Delcogliano A, Caporaso A, Chiossi S, Menghi A, Cillo M, Delcogliano M. Surgical management of chronic, unreduced posterior dislocation of the shoulder. Knee Surg Sports Traumatol Arthrosc 2005;13:151-5. [Google Scholar]
- 19.Benhamida MK, Ouertatani M, Hasayri I, Benhassine A, Meherzi M, Bouhdiba S, et al. Locked posterior dislocation of the shoulder: A report of three cases. Chir Main 2015;34:98-101. [Google Scholar]
- 20.Sanel S, Şencan S, Oçgüder A, Solakoğlu C. Bilateral, locked, recurrent anterior shoulder dislocation: Case report. Eklem Hastalik Cerrahisi 2015;26:52-5. [Google Scholar]
- 21.Purchase RJ, Wolf EM, Hobgood ER, Pollock ME, Smalley CC. Hill-sachs “remplissage”: An arthroscopic solution for the engaging hill-sachs lesion. Arthroscopy 2008;24:723-6. [Google Scholar]
- 22.Bühler M, Gerber C. Shoulder instability related to epileptic seizures. J Shoulder Elbow Surg 2002;11:339-44. [Google Scholar]