To prove the effective functional outcome and the use of platelet-rich plasma in the treatment of degenerative joint diseases of knee.
Dr. I Shebin Christin, Department of Orthopaedic Surgery, Vinayaka Missions Kirupananda Variyar Medical College and Hospitals, H3P7+8FR, Chinnasiragapadi, Salem - 636 308, Tamil Nadu, India. E-mail: shebinchristin@gmail.com
Introduction: Plasma rich in protein derived from platelets also known as platelet-rich plasma (PRP) is a recent science being used in many fields of medicine including cosmetic and musculoskeletal treatment. It has a very good ability to promote healing and decrease pain when added to certain treatment protocols. Being a simple and minimally invasive method of treatment, it is over-looked as a treatment option for the early osteoarthritis (OA) of knee joint. Well-designed randomized controlled studies and research are needed to measure outcomes, durability of effect while being cost effective
Aim of the Research Study: The aim of this study was to prove the use of PRP and its outcome in the clinical treatment of arthritic joint diseases of knee, progression of disease in people treated for early stage OA, and functional outcome of PRP injection in knee degenerative diseases.
Materials and Methods: This study was study period-6 months, sample size-50, sample type-patient, and functional outcome assessed using knee osteoarthritis outcome score (KOOS).
Methodology of Research Work: This study was aimed to prospectively quantify the effect of treatment with platelet-rich plasma (PRP) injection in patients with degenerative joint diseases. Degenerative joint disease treated using PRP injections with an average study period of 6 months was analyzed according to measure of pain at baseline and post-treatment using KOOS.
Data Analysis: Collected data will be analyzed by SPSS Software Version 19.
Primary Objective: PRP injections aim to relieve pain and to improve functional status of the patient.
Results: PRP is effective with treatment for degenerative knee arthritis. The patients found excellent relief in pain and mobility. The range of movement and KOOS score was found to be improved with P < 0.001.
Keywords: Platelet-rich plasma, cytokines, degenerative arthritis, knee osteoarthritis outcome scoring
As an autologous blood derivative, the platelets concentrated plasma protein is also known as platelet-rich plasma (PRP). It has been used in various medical fields involving skin to eye diseases and orthopedic surgery, with the aim of stimulating tissue healing through platelet-derived growth factor medium and other bioactive molecules. Platelet cells contain more cytokines and growth factors (GF) that can stimulate growth and duplication of cells, regeneration of tissues and collagen production. PRP injection provides a high level of these stimulants to the damaged tissue and helps regeneration. Conservative treatment has alleged scientifically to improve patient quality of living, more so in the beginning stages, where the cycle of pathology has minimal effects. PRP is a lot of platelets concentrated in a less amount of plasma. It is effect to a targeted tendon and cartilage tissue is evident.
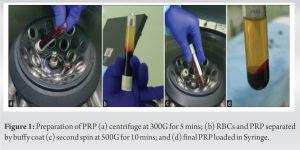
Preparation of PRP
To prepare PRP, it is recommended to use of “double-spin” method. Here, the blood is centrifuged at a speed to produce 100–300 G for 10 min in the first spin and then 400–700 G for 10–17 min for another spin (Fig. 1a-c). The sample prepared for treatment of degenerative conditions is recommended to contain at least 1,000,000–1,500,000 platelets/ml [1, 2]. As it is injected into soft-tissues activation of the content is not necessary. Collection of blood, preparation, and injection were done on the same day. Storage was not recommended [2].
Inclusion and exclusion criteria
Patient with the early degenerative changes was chosen for the treatment. Elderly who benefits more from total knee replacement or other conservative managements were excluded from the study [3]. Infection local and remote was a contra-indication. Other patients with thrombocytopenia or coagulation disorders were not advised to undergo PRP treatment. In general, patients were counseled and explained the nature of the treatment and teamed with proper physiotherapy. Our study group includes patients, 50–80 years, with Kellgren and Lawrence Grade 1 and 2 Osteoarthritis of knee [4]. Informed and signed consents taken from all patients.
The Ethical Committee of VMKV Medical College and Hospital, Salem was consulted and approved the study.
Procedure
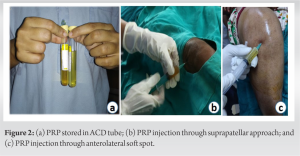
The patients were prepared and sterile drapped. A 6 ml PRP was injected intra-articular through the anterolateral soft spot or the superior-lateral-patellar approach of the knee [5] (Fig. 2a-c). The Fig 2d shows a sterile syringe loaded with the prepared PRP. Cycling done passively and the patients were advised rest for up to 1 day. Compression dressing and ice pack with oral NSAID and Collagen-1, Glucosamine supplements were given. Total of three injections given for 1 month interval. They were reviewed and compared with knee osteoarthritis outcome score (KOOS) over 0, 1, 2, 3, and 6 months (Table 1).
Two patients had persistent swelling for 3 days – Resolved with ice compression.
• No case of infection seen.
• No drop outs.
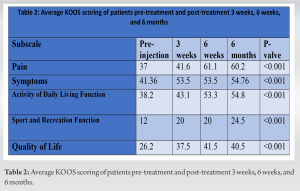
The results of the study were charted with the pain scale and grading by the KOOS (Table 2). The KOOS is a useful tool in compiling short-and long-term functional quality of knee. It comprises five questions regarding pain, four under symptoms, nine about the day-to-day activity, three questions under recreational and leisure, and two questions for life quality. The score is calculated in percentage from 0 to 100, with 0% being worst of problems and 100% no problems [6]. Patients with regular follow-up were found to have a significant improvement of the KOOS score over the period of evaluation. The average score was charted (Chart 1) and “P” value was derived.
Osteoarthritis (OA) is the most common chronic joint illness changing the life activities and functions of living widely [7]. It is a cascade of progressive dehydration, cartilage withering, eburnation with formation of loose bodies, and sclerosis of joint surface [4, 7]. The histopathological findings of OA are caused by increase of inflammatory markers such as IL-1, TNF-α, matrix metalloproteinases, nitric oxide, and prostaglandins between the destruction and repair mechanisms of articular cartilage. It shows that homeostasis is disturbed by reduced production of GF, collagen forming protein, proteoglycans, and other anti-inflammatory cytokines (IL-4 and IL-10) and leading to joint destruction [8]. PRP treatment in these joints decreases destruction and matrix formation, and synovium improved hyaluronan synthase-2 production and regeneration of cartilaginous cells. The “α” granules of platelet induce release of various GF, including vascular endothelial growth factor. All this aids cell proliferation and protein secretion in a previously deranged knee joint cartilage [9]. Injections of plasma proteins from platelet cell concentrate thus control pain and thickness of synovium, mostly by altering targeted of M1 and M2 macrophage-associated factors [10]. The pain in arthritis is leukocyte dependent. PRP reduces IL-1β, which produces a chain of 2α in turn reducing leukocyte activity. Some studies with microRNAs suggest delay in PRP treated knee progression of arthritis by controlling inflammation and apoptosis. It is also proven that activated or in-active PRP injections had no differences in vivo observations. GFs released after PRP injection into OA knee joint such as TNF, IGF, transforming growth factor, disintegrin, and fibroblastic growth factor are also shown to have significance [11, 12].
PRP is a wonder therapy in degenerating knee. More number of clinical studies and their results based on outcomes in the early OA knee it has become evident [13]. It is a simple, day care procedure, and relatively cost effective in institutional setting. As it provides natural environment for repair of joint, safety is guaranteed. This study showed significant reduction of pain and improved joint activities of patient with measurable increase in active flexion without pain more beneficial in early disease. Hence, we conclude that PRP injection is a promising therapy for the early aseptic degenerative diseases of knee.
PRP is a wonder therapy in degenerating knee. More number of clinical studies and their results based on outcomes in the early OA knee it has become evident [11]. It is a simple, day care procedure, and relatively cost effective in institutional setting. As it provides natural environment for repair of joint, safety is guaranteed. This study showed significant reduction of pain and improved joint activities of patient with measurable increase in active flexion without pain more beneficial in early disease. Hence, we conclude that PRP injection is a promising therapy for the early aseptic degenerative diseases of knee.
References
- 1.Helmick CG, Lawrence RC, Felson DT, Gabriel S, Hirsch R, Deyo RA, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States Part II. Arthritis Rheum 2008;58:15-25. [Google Scholar]
- 2.Gerwin N, Hops C, Lucke A. Intraarticular drug delivery in osteoarthritis. Adv Drug Deliv Rev 2006;58:226-42. [Google Scholar]
- 3.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis 1957;16:494-502. [Google Scholar]
- 4.Araki J, Jona M, Eto H, Aoi N, Kato H, Suga H, et al. Optimized preparation method of platelet-concentrated plasma and noncoagulating platelet-derived factor concentrates: Maximization of platelet concentration and removal of fibrinogen. Tissue Eng Part C Methods 2011;18:176-85. [Google Scholar]
- 5.J Cutan Aesthet Surg. 2014 Oct-Dec; 7(4): 189–197.; doi: 10.4103/0974-2077.150734; PMCID: PMC4338460; PMID: 25722595; Principles and Methods of Preparation of Pl a te l e t-Ri ch Pl a sma : A Re v i ew and Author's Perspective Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4338460. [Google Scholar]
- 6.Sharma B. Efficacy of knee osteo-arthritis outcome score (KOOS) in measuring functional status of knee osteo-arthritis patients in the Indian population. Indian J Physiother Occup Ther Int J 2012;6:73-5. [Google Scholar]
- 7.Chahla JL, Cinque ME, Piuzzi NS, Mannava S, Geeslin AG, Murray IR, et al. A call for standardization in platelet-rich plasma preparation protocols and composition reporting: A systematic review of the clinical orthopaedic literature. J Bone Joint Surg Am 2017;99:1769-79. [Google Scholar]
- 8.Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage 2008;16:137-62. [Google Scholar]
- 9.Halpern B, Chaudhury S, Rodeo SA, Hayter C, Bogner E, Potter HG, et al. Clinical and MRI outcomes after platelet-rich plasma treatment for knee osteoarthritis. Clin J Sport Med 2013;23:238-9. [Google Scholar]
- 10.Akeda K, An HS, Okuma M, Attawia M, Miyamoto K, Thonar EJ, et al. Platelet rich plasma stimulates porcine articular chondrocyte proliferation and matrix biosynthesis. Osteoarthritis Cartilage 2006;14:1272-80. [Google Scholar]
- 11.Patel S, Dhillon MS, Aggarwal S, Marwaha N, Jain A. Treatment with platelet-rich plasma is more effective than placebo for knee osteoarthritis a prospective, double-blind, randomized trial. Am J Sports Med 2013;41:356-64. [Google Scholar]
- 12.Dold AP, Zywiel MG, Taylor DW, Dwyer T, Theodoropoulos J. Platelet-rich plasma in the management of articular cartilage pathology: A systematic review. Clin J Sport Med 2014;24:31-43. [Google Scholar]
- 13.Raeissadat SA, Rayegani SM, Babaee M, Ghorbani E. The effect of platelet-rich plasma on pain, function, and quality of life of patients with knee osteoarthritis. Pain Res Treat 2013;2013:165967. [Google Scholar]