All differential diagnoses should be taken into consideration when dealing with any seemingly apparent knee problem.
Dr. Georgios Kalinterakis, Department of Trauma and Orthopedics, General Hospital of Rethymnon, Rethymnon 74100, Greece. E-mail: gkalinterakis@gmail.com
Introduction: Giant cell tumors(GCT) are uncommon and benign tumors originating due to proliferation of the tendon synovial sheath. Most commonly are located in the fingers. Involvement of the patellar tendon in the knee is extremely rare.
Case Report: We report two cases who presented with moderate swelling located in the anterior surface of the knee, localized anterior knee pain, and painful loss of flexion and catching and locking symptoms. Following detailed imaging evaluation, both cases were treated with open surgical excision and patellar tendon synovectomy. Histological examination revealed the presence of a giant cell tumor of the patellar tendon sheath in both cases.
Conclusion: Despite the rarity to GCT, the importance of considering all possible tumors in cases where a soft-tissue tumor is present should be stressed out.
Keywords: Giant cell tumor, patellar tendon, nodular synovitis, knee.
Giant cell tumor (GCT), also known as pigmented villonodular synovitis, is a rare, slow-growing, and benign neoplasm which arises from the synovium of a joint, tendon sheath, or bursa. Although it was first described by Jaffe et al. in 1941[1], it was only in 2002 when the World Health Organization clarified the histological description of this entity[2]. These tumors are separated into two distinct types: Diffuse type GCT and GCT originating from a tendon sheath. The diffuse type demonstrates more extensive involvement of the synovial membrane and capsule while the local form is less aggressive and is being confined to a distinct area of the synovium[3].
Giant cell tumors of the tendon sheath (GCTTS) are predominantly encountered in the hand and especially in the fingers followed by the ankle and foot. The incidence in the adult knee is approximately 1.8 in each million, but this includes both the diffuse and the localized form [4]. These tumors usually affect individuals aged between 30and 50 years, with female predominance [2]. The etiology remains unclear and a previous trauma history having been reported only in 15% of the cases [5]. The symptoms of GCTTS are non-specific and the diagnosis of GCTTS may be challenging particularly in large joints such as the knee where the symptoms are not specific and can therefore easily be mistaken for common injuries. A high index of suspicion is thus required. Magnetic resonance imaging (MRI)plays a crucial role in the diagnosis as opposed to plain radiographs which are not helpful [6]. The treatment of choice is surgical excision either arthroscopically or through a limited parapatellar approach. Despite its benign nature, the rate of local recurrence after excision has been reported to range between 10%and 20% [7, 8].
To date, only a few cases of GCTTS have been reported in the knee, especially arising from the patella tendon sheath. The present study reports two unusual cases in the knee mimicking a meniscaltear due to presence of catching and locking during knee flexion. The present study may assist clinicians in making the correct diagnosis in cases with non-traumatic knee mechanical symptoms and loss of motion.
Case 1
A22-year-old male football player presented to the outpatient orthopedic clinic with pain on the right knee localized at the medial joint line. The pain had appeared 2weeks prior his initial visit to the hospital after a mild injury during a football game. After the injury, the patient was not able to continue the game due to knee swelling and pain. His symptoms failed to improve with rest, anti-inflammatory medication, and physiotherapy. There was no history of prior knee trauma as well as nothing remarkable in his medical history. During the clinical examination, the patient’s knee presented mild swelling without increased skin temperature. He reported tenderness on palpation of the anteromedial aspect of the knee and discomfort with McMurray’s test. Furthermore, there was a decrease in knee flexion to 115° with no signs of ligamentous instability. The patient reported that limitation of flexion was present for 6 months compared to the contralateral knee. Neurovascular assessment revealed a strong palpable dorsally pedis and posterior tibial pulse while sensation of the lower extremity was normal. Plain radiography showed increased density at the infrapatellar region on the lateral view while nothing noteworthy was evident on the anteroposterior view (Fig. 1a and b).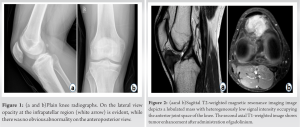 Blood analysis and basic metabolic panel results were within the normal range. MRI of the right knee demonstrated the presence of a homogenous and discrete mass with low-intensity signal in both T1 and T2 sequences with diffuse enhancement after administration of gadolinium, located in the infrapatellar region posterior and medial to the patellar tendon (Fig. 2a and b). Acomputed tomography (CT)-guidedbiopsy with fine needle aspiration was performed revealing the presence of mononuclear cells and giant cells indicative of GCTTS. The patient underwent complete open excision thorugh a medial parapatellar approach. A unique, solid,lobulated,49×40×32 mm in size, intraarticular soft-tissue mass adherent to the posterior surface of the patella tendon was excised(Fig. 3). Histological revealed the presence of dense fibrous tissue with accumulation of histiocytes and multinucleated giant cells establishing the diagnosis of GCT (Fig. 4). Recuperation of the patient was uneventful, and he returned to sports activities 1-month postoperatively. During the 20-month follow-up period, there was no evidence of tumor recurrence.
Blood analysis and basic metabolic panel results were within the normal range. MRI of the right knee demonstrated the presence of a homogenous and discrete mass with low-intensity signal in both T1 and T2 sequences with diffuse enhancement after administration of gadolinium, located in the infrapatellar region posterior and medial to the patellar tendon (Fig. 2a and b). Acomputed tomography (CT)-guidedbiopsy with fine needle aspiration was performed revealing the presence of mononuclear cells and giant cells indicative of GCTTS. The patient underwent complete open excision thorugh a medial parapatellar approach. A unique, solid,lobulated,49×40×32 mm in size, intraarticular soft-tissue mass adherent to the posterior surface of the patella tendon was excised(Fig. 3). Histological revealed the presence of dense fibrous tissue with accumulation of histiocytes and multinucleated giant cells establishing the diagnosis of GCT (Fig. 4). Recuperation of the patient was uneventful, and he returned to sports activities 1-month postoperatively. During the 20-month follow-up period, there was no evidence of tumor recurrence.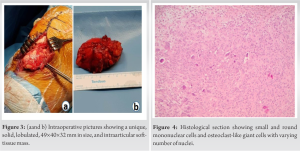
Case 2
A 35-year-old female gymnast presented with a history of right knee pain for 1 year, especially with knee flexion along with symptoms of locking and catching. She was referred from her general practioner with the initial diagnosis of a meniscal tear. There was no history knee trauma. On clinical examination, the patient presented with moderate knee swelling with 110° of knee flexion as opposed to 130° on the contralateral knee. In addition, the patient reported a lateral movement sensation on knee flexion, resembling dislocation of the patella. A mildly painful firm and mobile soft-tissue mass arising from the lateral aspect of her patella tendon was noted. X-ray evaluation and hematological examination were normal. MRI showed the presence of a well-defined lobulated lesion (2.4×1.7×1.2 mm)with low signal intensity in both T1- and T2‑weighted images arising from patella tendon (Fig. 5). The mass was excised with an open parapatellar approach and synovectomy of the patellar tendon was also performed. The post-operative period was uneventful, the effusion resolved, and there were no further episodes of locking or catching.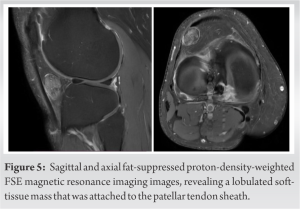
GCTTS are uncommon soft-tissue tumors with limited published cases. They are benign nodular tumors encountered in the extremities and originate from the synovial tissue of the joints, tendon sheaths, bursa, and fibrous tissue adjacent to tendons [9]. The average age of patients with GCTTS is typically from 30 to 50 years old and is particularly encountered in women. However, incidents of the lesion in younger patients have also been reported [10, 11, 12, 13]. Up to now, several cases of GCTTS originating in the knee joint have been reported in the literature [14, 15, 16, 17] and the cases regarding the patellar tendon are extremely rare (Table 1).
One of the most important clinical features of GCTTS is that the symptoms are non-specific. Thus, clinical manifestations vary from a painless slow-growing mass to local warmth, swelling, stiffness, and limitation of knee movements. In exceptional cases, this tumor may present with symptoms that suggest acute mechanical derange-ment such as catching or locking, imitating meniscal tears, or loose bodies [18, 19]. In this study, we present two cases of GCTTS mimicking a meniscal tear.
Imaging evaluation is an essential part of the diagnostic workup. Conventional plain radiographs are usually of limited benefit but occasionally Hoffa’s fat pad with its radiographic lucency may be replaced with areas of soft-tissue opacity[20]. If the disease is more aggressive, small cystic formations orperi-articular cortical erosion can sometimes be observed [21,22]. MRI imaging is the most valuable diagnostic modality. GCTTS appear as well circumscribed lesions which exhibit low signal intensity on both T1-and T2-weighted images due to the presence of dense fibrous tissue, as exemplified in our cases. The signal features are believed to be correlated with the varying amounts of hemosiderin in the lesion. Therefore, in case of hemosiderin deposits which are much more apparent on gradient echo images, T2-weighted images show variable signal intensity. Adding intra-articulargadolinium can help identify the nodules, especially in cases with minimal hemosiderin deposits [23, 24, 25]. Moreover, it should be pointed out that malignant tumors and other benign soft tissue tumors may be differentiated from GCTTS based on their radiographic features. Synovial sarcoma and malignant fibrous histiocytoma exhibit a non-homogenous appearance on MRI while they are characterized by calcifications and poorly defined margins [26]. Ganglion cysts show high signal intensity on T2 images without gadolinium enhancement, while lipomas demonstrate high signal on both T1- and T2-weighted images and saturation on fat suppression sequences [27].
Imaging-guided percutaneous needle biopsy for histopathological examination may occasionally be indicated, using ultrasound or CT imaging, although the definitive diagnosis can only be safely made with excision biopsy. The criteria for the diagnosis of GCT are proliferation of the synovial tissue with villi orsynovial nodules, hemosiderin deposits, a variable number of fibroblasts, and giant cells with fibrosis and hyalinization [28].
The principal treatment for GCTTS is surgical resection. For this purpose, either open or arthroscopic surgery can be performed. At present, there is no consensus regarding which technique is superior. The size, the site, and the extent of the tumor are important factors for the selection of the surgical excision. In Case 1, the size of the lesion was 4.9 cm at its largest dimension, so an open arthrotomy was preferred. It is of note that only a handful of giant cell tumors of the patellar tendon of this size have been reported in the literature [12, 29, 30, 31, 32]. Arthroscopic approaches have increased their popularity because they are minimally invasive procedures and reduce the risk of complications. A systematic review conducted by Van der Heijden et al. [9], showed no significant difference in terms of recurrence rates after open and arthroscopic resection of tumors. On the contrary, a recent international, multicenter, and cohort study showed that two factors associated with increased recurrence rates were the size of the tumor and initial treatment with arthroscopy. The same study concluded that open surgical approach most commonly leads to fewer complications and better functional outcomes [32].
GCTTS involving the patellar tendonisa rare entity and may mimic a variety of intraarticular knee problems. Adequate pre-operative imaging and complete tumor excision lead to permanent treatment of the tumor.
The present case study underlines the unique features of GCTTS in the knee mimicking a meniscal tear. Although it is uncommon, this entity should be taken into account more often in differential diagnosis of knee problems.
References
- 1.Jaffe HL, Lichtenstein L, Sutro CJ: Pigmented villonodular synovitis, bursitis, tenosynovitis. Arch Pathol, 1941; 31: 731–65. [Google Scholar]
- 2.Somerhausen NA, Dal Cin P. Diffuse-type giant cell tumour. In: Fletcher CD, Unni KK, Mertens F, editors. Pathology and Genetics of Tumours of Soft Tissue and Bone. Lyon: IARC Press; 2002. p. 112-4. [Google Scholar]
- 3.De Ponti A, Sansone V, Malcherè M. Result of arthroscopic treatment of pigmented villonodular synovitis of the knee. Arthroscopy 2003;19:602-7. [Google Scholar]
- 4.Myers BW, Masi AT. Pigmented villonodular synovitis and tenosynovitis: A clinical epidemiologic study of 166 cases and literature review. Medicine (Baltimore) 1980;59:223-38. [Google Scholar]
- 5.Uriburu IJ, Levy VD. Intraosseous growth of giant cell tumors of the tendon sheath (localized nodular tenosynovitis) of the digits: Report of 15 cases. J Hand Surg Am 1998;23:732-6. [Google Scholar]
- 6.Abdul-Karim FW, El-Naggar AK, Joyce MJ, Makley JT, Carter JR. Diffuse and localized tenosynovial giant cell tumor and pigmented villonodular synovitis: A clinicopathologic and flow cytometric DNA analysis. Hum Pathol 1992;23:729-35. [Google Scholar]
- 7.Weiss SW, Goldblum JR, editors. Benign tumors and tumor-like lesions of synovial tissues. In: Enzinger and Weiss’s Soft Tissue Tumors. 5th ed. St Louis, MO: Mosby; 2007. p. 769-88. [Google Scholar]
- 8.Lowyck H, Smet L. Recurrence rate of giant cell tumors of the tendon sheath. Eur J Plast Surg 2006;28:385-8. [Google Scholar]
- 9.Van der Heijden L, Gibbons CL, Dijkstra PD, Kroep JR, van Rijswijk CS, Nout RA, et al. The management of diffuse-type giant cell tumour (pigmented villonodular synovitis) and giant cell tumour of tendon sheath (nodular tenosynovitis). J Bone Joint Surg Br 2012;94:882-8. [Google Scholar]
- 10.Sharma H, Jane M, Reid R. Pigmented villonodular synovitis: Diagnostic pitfalls and management strategy. Curr Orthop 2005;19:215-22. [Google Scholar]
- 11.Sun C, Sheng W, Yu H, Han J. Giant cell tumor of the tendon sheath: A rare case in the left knee of a 15-year-old boy. Oncol Lett 2012;3:718-20. [Google Scholar]
- 12.Abdullah A, Abdullah S, Haflah NH, Ibrahim S. Giant cell tumor of the tendon sheath in the knee of an 11-year-old girl. J Chin Med Assoc 2010;73:47-51. [Google Scholar]
- 13.Atik OŞ, Bozkurt HH, Özcan E, Bahadır B, Uçar M, Öğüt B, et al. Localized pigmented villonodular synovitis in a child knee. Eklem Hastalik Cerrahisi 2017;28:46-9. [Google Scholar]
- 14.Camillieri G, Di Sanzo V, Ferretti M, Calderaro C, Calvisi V. Intra-articular tenosynovial giant cell tumor arising from the posterior cruciate ligament. Orthopedics 2012;35:e1116-8. [Google Scholar]
- 15.Kim YM, Joo YB. Localized nodular tenosynovitis originated near the medial plicae. Knee Surg Relat Res 2014;26:52-5. [Google Scholar]
- 16.Otsuka Y, Mizuta H, Nakamura E, Kudo S, Inoue S, Takagi K. Tenosynovial giant-cell tumor arising from the anterior cruciate ligament of the knee. Arthroscopy 1996;12:496-9. [Google Scholar]
- 17.Khanduja V, Dannawi Z, Ng L, El-Zebdeh M. Giant-cell tumor of the tendon sheath arising from the patellar tendon. J Knee Surg 2004;17:28-9. [Google Scholar]
- 18.Ozalay M, Tandoğan RN, Akpinar S, Cesur N, Hersekli MA, Ozkoç G, et al. Arthroscopic treatment of solitary benign intra-articular lesions of the knee that cause mechanical symptoms. Arthroscopy 2005;21:12-8. [Google Scholar]
- 19.Loriaut P, Djian P, Boyer T, Bonvarlet JP, Delin C, Makridis KG. Arthroscopic treatment of localized pigmented villonodular synovitis of the knee. Knee Surg Sports Traumatol Arthrosc 2012;20:1550-3. [Google Scholar]
- 20.Murphey MD, Rhee JH, Lewis RB, Fanburg-Smith JC, Flemming DJ, Walker EA. Pigmented villonodular synovitis: Radiologic-pathologic correlation. Radiographics 2008;28:1493-518. [Google Scholar]
- 21.Akahane T, Morin, Yoshida K. Giant cell tumor of the tendon sheath extending around the patellar tendon and invading the knee joint and tibia: A case report. Oncol Lett 2014;8:2800-2. [Google Scholar]
- 22.Dines JS, DeBerardino TM, Wells JL, Dodson CC, Shindle M, DiCarlo EF, et al. Long-term follow-up of surgically treated localized pigmented villonodular synovitis of the knee. Arthroscopy 2007;23:930-7. [Google Scholar]
- 23.Bessette PR, Cooley PA, Johnson RP, Czarnecki DJ. Gadolinium-enhanced MRI of pigmented villonodular synovitis of the knee. J Comput Assist Tomogr 1992;16:992-4. [Google Scholar]
- 24.Jelinek JS, Kransdorf MJ, Utz JA, Berrey BH, Thomson JD, Heekin RD, et al. Imaging of pigmented villonodular synovitis with emphasis on MR imaging. AJR Am J Roentgenol 1989;152:337-42. [Google Scholar]
- 25.Kottal RA, Vogler JB, Matamoros A, Alexander AH, Cookson JL. Pigmented villonodular synovitis: A report of MR imaging in two cases. Radiology 1987;163:551-3. [Google Scholar]
- 26.26. Kitagawa Y, Ito H, Amano Y, Sawaizumi T, Takeuchi T. MR imaging for preoperative diagnosis and assessment of local tumor extent on localized giant cell tumor of tendon sheath. Skeletal Radiol 2003;32:633-8. [Google Scholar]
- 27.Jacobson JA, Lenchik L, Ruhoy MK, Schweitzer ME, Resnick D. MR imaging of the infrapatellar fat pad of Hoffa. Radiographics 1997;17:675-91. [Google Scholar]
- 28.Kumar R, Bharani V, Gupta N, Gupta K, Dey P, Srinivasan R, et al. Giant cell tumour of tendon sheath: A 10-year study from a tertiary care centre. Cytopathology 2018;29:288-93. [Google Scholar]
- 29.Panagopoulos A, Tsoumpos P, Tatani I, Iliopoulos I, Papachristou D. Giant cell tumor of the patella tendon sheath presenting as a painful locked knee. Am J Case Rep 2015;16:568-73. [Google Scholar]
- 30.Bedir R, Balik MS, Sehitoglu I, Güçer H, Yurdakul C. Giant cell tumour of the tendon sheath: Analysis of 35 cases and their Ki-67 proliferation indexes. J Clin Diagn Res 2014;8:FC12-5. [Google Scholar]
- 31.Chechik O, Amar E, Khashan M, Morag G. Giant cell tumors in the patellar tendon area. J Knee Surg 2010;23:115-9. [Google Scholar]
- 32.Kılıçaslan ÖF, Katı YA, Kose O, Erol B, Alikanoglu AS. Giant cell tumor of the patellar tendon sheath: A rare case of anterior knee pain. Cureus 2017;9:e1690. [Google Scholar]
- 33.Mastboom MJ, Staals EL, Verspoor FG, Rueten-Budde AJ, Stacchiotti S, Palmerini E, et al. Surgical treatment of localized-type tenosynovial giant cell tumors of large joints: A study based on a multicenter-pooled database of 31 international Sarcoma centers. J Bone Joint Surg Am 2019;101:1309-18. [Google Scholar]
- 34.Arıcan M, Turhan Y, Gamsızkan M. A rare localized giant cell tumor of the tendon sheath originating from the ligamentum mucosum: A case report. Jt Dis Relat Surg 2020;31:149-53. [Google Scholar]
- 35.Lu KH. Arthroscopic excision of juxta-articular giant-cell tumor arising from the patellar tendon sheath. Arthroscopy 2004;20:eE35-8. [Google Scholar]
- 36.Goyal R, Chopra R, Bhatia N, Goel A, Gupta P. Unusual occurrence of tenosynovial giant cell tumor in Hoffa’s fat pad: A potential differential diagnosis for nontraumatic knee swelling and pain. Cureus 2020;12:e9008. [Google Scholar]
- 37.Relwani J, Factor D, Khan F, Dutta A. Giant cell tumour of the patellar tendon sheath--an unusual cause of anterior knee pain: A case report. Knee 2003;10:145-8. [Google Scholar]











