Spontaneous spinal epidural hematoma can be rarely seen in pregnancy and the patient presents with acute onset paraparesis. Clinical suspicion of this rare condition, early diagnosis and multidisciplinary approach for management are necessary for better outcome of both mother and baby.
Dr. Suprava Naik, Department of Radiodiagnosis, All India Institute of Medical Sciences, Bhubaneswar - 751 019, Odisha, India. E-mail: drsuprava.rd@gmail.com
Introduction: Spontaneous development of spinal epidural hematoma (SEH) is rare condition with acute presentation and usually associated with some predisposing factors. Early diagnosis and management of SEH are very important because of the risk of permanent neurological deficit.
Case Report: Here, we report a rare case of SEH in young pregnant female at 35 week of gestation who presented with short history of paraplegia that was diagnosed on magnetic resonance imaging (MRI) and treated successfully with delivery of the baby by caesarean section and release of cord compression by laminectomy.
Conclusion: Spontaneous SEH can be rarely seen in pregnancy. MRI is the investigation of choice. Clinical suspicion is necessary for early management and better prognosis.
Keywords: Epidural hematoma, paraplegia, pregnancy.
Non-traumatic paraplegia developing in pregnancy is rare phenomenon with only sporadic reports [1, 2, 3]. Spontaneous development of spinal epidural hematoma (SEH) without any predisposing factor is rare and even more sporadic in pregnancy. The etiologies of SEH include hypertension, vascular malformation, neoplasia, and use of anticoagulant medications [4]. High clinical suspicion of this rare condition is necessary for better outcome of both mother and baby. Usual clinical presentation includes neck pain, pain in the interscapular area or back pain that progresses to paraparesis or quadriparesis depending on the location of hematoma. Immediate diagnosis and treatment are of utmost importance for better outcome. Standard treatment includes urgent operative decompression of the hematoma and conservative management and close monitoring for patients who show spontaneous recovery in short period of time. Delivery of the baby may be carried out in the same setting or at a later date depending of the gestational age. Here, we report a rare case of spontaneous SEH in a 35 weeks pregnant lady who presented with acute onset paraplegia.
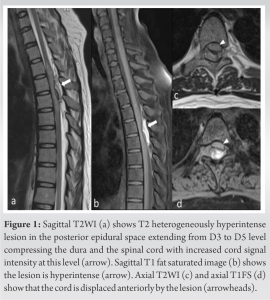
A 28-year pregnant female G1P0L0 presented with sudden onset upper back pain and associated weakness of bilateral lower limbs of 8 days duration. There was no history of trauma, fever, seizure, or altered sensorium. There was no history of bleeding disorders since childhood or intake of any anticoagulant, or tuberculosis. On examination, she was afebrile, vitals were stable. BP 110/80 mm of Hg, pulse of 84/min., and the abdomen distended corresponding to the 35 weeks gestational age. Fetal heart rate was 140/min and fetal movement could be appreciated. The neurological examination showed complete paraplegia (MRC-0/5 in both limbs) with a sensory level of D6. The bladder was catheterized and perianal sensation was absent. A magnetic resonance imaging (MRI) was done for further evaluation that showed elongated T2 and T1 hyperintense lesion (over a length of 3.5 cm and maximum thickness 8 mm) in posterior epidural region extending from D3 to D5 vertebral level. Signal of the lesion was not suppressed on fat suppressed image. The lesion was displacing the thecal sac and spinal cord anteriorly causing cord compression and increased T2 signal of the spinal cord at this level (Fig. 1). Vertebral bodies and intervertebral disc spaces appeared normal. Diagnosis of subacute posterior epidural hematoma causing compressive myelopathy was made based on MRI. Routine biochemical investigations revealed Hb-12 g/mL, TLC of 11,400, sodium of 142 meq/l, potassium of 4.5 meq/l, and platelet of 2.5 lacs/cmm. The patient had a normal bleeding time, prothrombin time and was negative for Protein C, Protein S, or Antiphospholipid antibody. Her TSH was raised to 102 mlU/l at the time of admission. The mother was given steroidsfor lung maturation of the fetus and after 48 h, a caesarean section (CS) was done and baby delivered. With escalating dose of thyroxine, laminectomy and decompression of spinal canal done and hematoma drained. The baby was normal while the mother was started on physiotherapy and electrical stimulation. At 6 months post-surgery, there is improvement in 2 grade MRC and one grade sensory. The patient is ambulatory on a wheel chair.
SEH is a rare cause of spinal cord compression and spinal emergency seen in 0.3–0.9% of all epidural space-occupying lesions [5]. Post-traumatic SEH is common in men having ankylosing spondylitis or rheumatoid arthritis. Non-traumatic SEH is usually seen in patients having congenital or acquired bleeding disorders, spinal arteriovenous malformations, hemorrhagic tumors, and in hypertensive patients [4]. In patients without any predisposing factors, possible etiopathogenesis could be acute increase of the spinal epidural venous pressure. Epidural veins are more susceptible to congestion during pregnancy [6].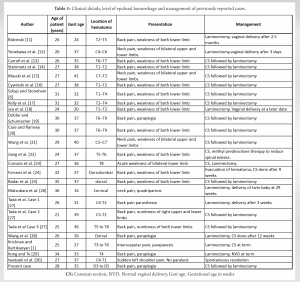
Spontaneous SEH in pregnancy is a rare clinical condition with acute presentation. Clinical suspicion is necessar y for early management. MRI is the investigation of choice. Early decompression is required to avoid complications.
Diagnosis of a case of acute onset paraplegia is challenging. Most common cause for the same is dorsal cord compression. MRI is the investigation of choice to see the status of the spinal cord and extent of involvement. Also, it does not use ionizing radiation and thus relatively safe in pregnancy. Early diagnosis and management are necessary to avoid detrimental consequences.
References
- 1.Krishnan P, Kartikueyan R. Spontaneous spinal epidural hematoma: A rare cause of paraplegia in pregnancy. Neurol India 2014;62:205-7. [Google Scholar]
- 2.Kaushal S, Dora SK, Thakur S. Spinal tuberculosis with paraplegia in pregnancy. JNMA J Nepal Med Assoc 2015;53:123-5. [Google Scholar]
- 3.Kulkarni M, Tv S, Gopal N. Hypokalemic paraplegia in pregnancy. J Clin Diagn Res 2014;8:OD03-4. [Google Scholar]
- 4.Groen RJ, Ponssen H. The spontaneous spinal epidural hematoma. A study of the etiology. J Neurol Sci 1990;98:121-38. [Google Scholar]
- 5.Alexiadou-Rudolf C, Ernestus RI, Nanassis K, Lanfermann H, Klug N. Acute non-traumatic spinal epidural hematomas. An important differential diagnosis in spinal emergencies. Spine (Phila Pa 1976) 1998;23:1810-3. [Google Scholar]
- 6.Szkup P, Stoneham G. Case report: Spontaneous spinal epidural haematoma during pregnancy: Case report and review of the literature. Br J Radiol 2004;77:881-4. [Google Scholar]
- 7.Mohanty CR, Jain M, Dash C, Behera SS. Postpartum paraparesis due to aggressive vertebral hemangioma causing spinal cord compression presenting for emergency cesarean section. J Obstet Gynaecol India 2019;69:185-7. [Google Scholar]
- 8.Henry JB, Messerer M, Thomas V, Diabira S, Morandi X, Hamlat A. Nontraumatic spinal epidural hematoma during pregnancy: Diagnosis and management concerns. Spinal Cord 2012;50:655-60. [Google Scholar]
- 9.Holtås S, Heiling M, Lönntoft M. Spontaneous spinal epidural hematoma: Findings at MR imaging and clinical correlation. Radiology 1996;199:409-13. [Google Scholar]
- 10.Bhoi SK, Naik S, Gupta D, Pradhan PK, Kalita J, Misra UK. Recurrent spontaneous cerebrospinal fluid leaks at multiple levels. Neurol India 2021;69:1828-30. [Google Scholar]
- 11.Bidzinski J. Spontaneous spinal epidural hematoma during pregnancy. Case report. J Neurosurg 1966;24:1017. [Google Scholar]
- 12.Yonekawa Y, Mehdorn HM, Nishikawa M. Spontaneous spinal epidural hematoma during pregnancy. Surg Neurol 1975;3:327-8. [Google Scholar]
- 13.Carroll SG, Malhotra R, Eustace D, Sharr M, Morcos S. Spontaneous spinal extradural hematoma during pregnancy. J Matern Fetal Med 1997;6:218-9. [Google Scholar]
- 14.Steinmetz MP, Kalfas IH, Willis B, Chalavi A, Harlan RC. Successful surgical management of a case of spontaneous epidural hematoma of the spine during pregnancy. Spine J 2003;3:539-42. [Google Scholar]
- 15.Masski G, Housni B, Ibahiouin K, Miguil M. Spontaneous cervical epidural haematoma during pregnancy. Int J Obstet Anesth 2004;13:103-6. [Google Scholar]
- 16.Cywinski JB, Parker BM, Lozada LJ. Spontaneous spinal epidural hematoma in a pregnant patient. J Clin Anesth 2004;16:371-5. [Google Scholar]
- 17.Kelly ME, Beavis RC, Hattingh S. Spontaneous spinal epidural hematoma during pregnancy. Can J Neurol Sci 2005;32:361-5. [Google Scholar]
- 18.Jea A, Moza K, Levi AD, Vanni S. Spontaneous spinal epidural hematoma during pregnancy: Case report and literature review. Neurosurgery 2005;56:E1156. [Google Scholar]
- 19.Doblar DD, Schumacher SD. Spontaneous acute thoracic epidural hematoma causing paraplegia in a patient with severe preeclampsia in early labor. Int J Obstet Anesth 2005;14:256-60. [Google Scholar]
- 20.Case AS, Ramsey PS. Spontaneous epidural hematoma of the spine in pregnancy. Am J Obstet Gynecol 2005;193:875-7. [Google Scholar]
- 21.Wang P, Xin XT, Lan H, Chen C, Liu B. Spontaneous cervical epidural hematoma during pregnancy: Case report and literature review. Eur Spine J 2011;20 Suppl 2:S176-9. [Google Scholar]
- 22.Jiang W, Tan XY, Li JA, Dong M. Spontaneous spinal epidural hematoma complicated by pulmonary embolism during pregnancy: A case report. Front Med (Lausanne) 2022;9:832693. [Google Scholar]
- 23.Consolo D, Vadala AA, Rollin P, Merle B, Girard C. Spontaneous spinal epidural haematoma during pregnancy. Ann Fr Anesth Reanim 2007;26:455-8. [Google Scholar]
- 24.Forsnes E, Occhino A, Acosta R. Spontaneous spinal epidural hematoma in pregnancy associated with using low molecular weight heparin. Obstet Gynecol 2009;113:532-3 [Google Scholar]
- 25.Badar F, Kirmani S, Rashid M, Azfar SF, Yasmeen S, Ullah E. Spontaneous spinal epidural hematoma during pregnancy: A rare obstetric emergency. Emerg Radiol 2011;18:433-6. [Google Scholar]
- 26.Matsubara S, Inoue H, Takamura K, Kimura A, Okuno S, Fujita A, et al. Spontaneous spinal epidural hematoma at the 16th week of a twin pregnancy. J Obstet Gynaecol Res 2011;37:1466-9. [Google Scholar]
- 27.Tada S, Yasue A, Nishizawa H, Sekiya T, Hirota Y, Udagawa Y. Spontaneous spinal epidural hematoma during pregnancy: Three case reports. J Obstet Gynaecol Res 2011;37:1734-8. [Google Scholar]
- 28.Wang ZL, Bai HX, Yang L. Spontaneous spinal epidural hematoma during pregnancy: Case report and literature review. Neurol India 2013;61:436-7. [Google Scholar]
- 29.Kong CW, To WW. Spontaneous spinal epidural haematoma during pregnancy. J Obstet Gynaecol 2018;38:129-31. [Google Scholar]
- 30.Iwatsuki K, Deguchi M, Hirata H, Kanamono T. Spontaneously resolved recurrent cervical epidural hematoma in a 37-week primigravida. Global Spine J 2015;5:e44-7. [Google Scholar]