All arthroscopic fixation of tibial spine avulsion fractures involving the ACL and PCL roots can be successfully carried out with current techniques, offering an opportunity to avoid an open approach to the posterior knee in cases where an adequate arthroscopic reduction of the PCL fragment can be achieved.
Dr. Jeremy R. Bruce, Department of Orthopaedic Surgery, University of Tennessee, College of Medicine, Chattanooga, Tennessee. E-mail: Jeremy.bruce@erlanger.org
Introduction: Tibial-sided anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) avulsion fractures compose a rare subset of cruciate ligament injuries. Fixation strategies are mixed in the literature, particularly regarding the PCL, which has traditionally been addressed using an open approach.
Case Report: A 41-year-old male sustained avulsion fractures of the tibial eminence involving the ACL, PCL, and posterior medial meniscal root through an unknown mechanism while sleepwalking. Surgical treatment comprised of entirely arthroscopic reduction and transtibial suture fixation. Only seven cases of combined ACL/PCL avulsion fracture have been reported and all but one utilized open fixation for at least the PCL and restricted weight-bearing postoperatively.
Conclusion: This previously unreported triad of injury was successfully managed arthroscopically, negating a posterior approach to the knee. Early post-operative weight-bearing and aggressive range of motion aided in swift recovery and a favorable outcome.
Keywords: Anterior cruciate ligament, posterior cruciate ligament, tibial spine fracture, multi-ligamentous knee injury.
The majority of anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) injuries occur as tears of the intrasubstance collagen fibers. This typically occurs with a valgus blow to the knee or a non-contact related twisting/pivoting injury for the ACL and either a direct anterior blow or hyperflexion/varus moment for the PCL. Sudden traumatic displacement of the knee, however, can result in avulsion fractures of these ligaments, most often from their tibial insertions. Ligamentous avulsion fractures are considered rare injuries even in the pediatric population, where they are more prone to occur due to the relative weakness of the insertion points compared to mid-substance [1]. Tibial-sided ACL avulsion fractures represent only 1–5% of all ACL injuries in adults. According to the literature, the incidence is 3:100,000 compared to 68.6:100,000 for mid-substance tears [2]. PCL injuries are much less frequent and represent 3–23% of all ligamentous knee injuries [3]. PCL avulsion fractures specifically make up a rare subset of PCL injuries with an incidence that has not been clearly stated in the literature. Posterior medial meniscal root tears are not a rare occurrence; however, the incidence of posteromedial meniscal root tears in multi-ligamentous knee injuries has been reported as 3% [4]. Simultaneous avulsion fracture of the ACL and PCL tibial insertions, from our understanding of the literature, has not been reported outside of the setting of high energy trauma. Further, no cases have been reported with a concomitant meniscal root avulsion fracture. We present the case of a patient who sustained combined ACL and PCL avulsion fractures in addition to a posterior medial meniscal root avulsion fracture with significant extrusion into the joint during an episode of sleepwalking.
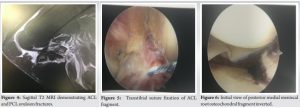
A healthy 41-year-old male presented to the Emergency Department after waking up in the middle of the night with severe left knee pain. The patient denied any history of antecedent pain or injury to the knee. He endorsed a remote history of a left femur and tibia fracture as a child that were successfully treated with surgery. He had no retained hardware. He reported a history of sleepwalking and stated that he went to bed with no knee pain whatsoever and awoke hours later with severe left knee pain, inability to bear weight, and a mechanical block to motion. On initial examination, he held the knee at 90°, the position of least pain. The knee was moderately swollen, but with no erythema or bruising. He had significant tenderness to palpation globally about the knee. Range of motion testing revealed an inability to extend the knee past 40°. Ligamentous examination was very limited secondary to guarding and pain. No tenderness, swelling, or abnormal range of motion was present about the hip or ankle. He was neurovascularly intact distally with ABI’s >1 bilaterally. Plain films of the left knee revealed a tibial eminence fracture with a large intraarticular osteochondral fragment and significant joint effusion (Fig. 1 and 2).
Computed tomography angiography of the left lower extremity was obtained prior to orthopedic evaluation due to suspicion for hyperextension/dislocation, which revealed no sign of vascular injury. MRI ultimately revealed a multi-fragmentary tibial spine avulsion fracture running anterior to posterior with complete involvement of the insertions of the ACL, PCL, and posterior horn of the medial meniscus (Fig. 3 and 4). In addition, the posterior medial fragment with attachment to the posterior horn of the medial meniscus appeared significantly displaced and angulated. The patient was placed in a knee immobilizer and given next day outpatient follow-up.
Surgical findings and treatment
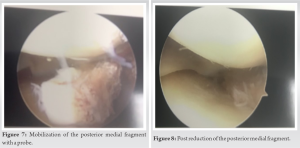
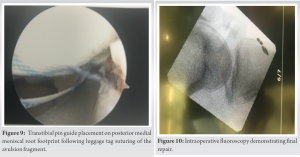
Four days after injury, the patient was taken to the operating room for arthroscopic repair of his avulsion fractures. The ACL was found to be mostly reduced and was secured in place with two #2 FiberWire (Arthrex, Inc., Naples, FL, USA) luggage tag sutures passed through an anteromedial transtibial pin tunnel (Fig. 5). These were tensioned, tied over a dog bone anchor, and secured to the tibia. The posterior medial fragment, which was attached to the posterior horn of the medial meniscus, was inverted and significantly displaced into the posterior medial compartment (Fig. 6 and 7).
Reduction of this piece was achieved with manipulation using a probe and grasper but was very difficult requiring three accessory medial portals (Fig. 8). Once fully reduced, a luggage tag stich was passed through the fragment while a probe held it in place (Fig. 9). A second stitch was passed into the minimally displaced PCL fragment. A transtibial pin was then passed through the meniscal root fragment and a second into the bony PCL fragment. The two separate tag stiches were then passed through their respective pin tunnels, tensioned, and tied over a single dog bone anchor on the anteromedial surface of the tibia (Fig. 10). The patient was then found to have stable anterior and posterior drawer testing.
Post-operative course
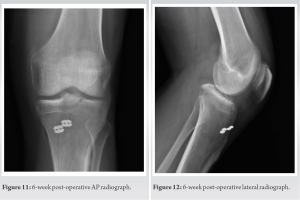
The patient was given a hinged knee brace and allowed to weight-bear as tolerated locked in extension immediately postoperatively. Early weight-bearing in the brace was ordered to aid with fracture site compression and early range of motion was encouraged to prevent post-operative stiffness. Physical therapy (PT) commenced 2 days after surgery. The patient dealt with a significant amount of pain in the first 2 weeks with therapy but was able to reach 5° of extension and 125° of flexion at 6-week postoperatively. At 2 months, the patient achieved full extension and 130° of flexion. Plain films reveal healing of his avulsion fractures and no hardware complication (Fig. 11 and 12). The patient continued with a home exercise program following discharge from formal PT. There have been no signs or reports from the patient of any complications to date at 2 years from injury.
An expansive search of the literature for cases of combined ACL/PCL avulsion injuries was carried out and included the following databases: NCBI, JAMA, PUBMED, Science Direct, and Research Gate. This search revealed seven total cases of combined ACL and PCL avulsion fractures, four of which were sustained in motorcycle crashes, one in a motor vehicle crash with an ipsilateral diaphyseal femur and patella fracture, and two with unspecified etiology [1, 5, 6, 7, 8]. Meniscal pathology was only noted in one case, which was a white zone lateral meniscus tear [6]. Interestingly, only one of seven cases was treated entirely arthroscopically [1]. All others had a combination of arthroscopic treatment for the ACL and open vs. mini-open treatment of the PCL. Literature review was also carried out regarding the prevalence and types of injuries sustain during sleep walking. About 2–3% of adults experience sleepwalking episodes [9]. Injury during sleepwalking is exceedingly rare and the spectrum is clearly vast. In a study of ER admissions following injury during sleepwalking, there were only 11 patients among 620,000 admissions related to sleepwalking trauma. Four of these patients sustained orthopedic injuries requiring intervention; however, there were no reports of knee trauma. The spectrum of injury included minor lacerations and contusions to multisystem trauma in one patient including intracranial hemorrhage, craniofacial fractures, cervical spine fractures, open femur fracture, and multiple soft-tissue contusions after a patient fell out of a window while sleepwalking [10]. The mechanism of injury during this patient’s sleepwalking episode is unfortunately unknown. The treatment chosen for our patient was comprised of an all-arthroscopic approach. Both the ACL and posteromedial root avulsion injuries were treated with a transtibial suture repair, which appears to be largely the treatment of choice today according to the literature for arthroscopically reducible fractures [4, 11]. Other options include transtibial wiring or cannulated screw fixation [12]. Surgical treatment of PCL avulsion injuries, however, has been under debate in the literature. Hooper et al. carried out a systematic review comparing open versus arthroscopic treatment of PCL avulsion type injuries. Patients who underwent arthroscopic fixation saw better postoperative subjective outcomes and 100% of them reported return to previous level of activity (vs. 86.2% in the open group). The arthroscopic group did experience a statistically significant higher rate of arthrofibrosis (0–36% vs. 0–25%). The authors emphasized that the clear advantage of arthroscopic fixation is the ability to directly visualize important intra-articular structures and address concomitant pathology while limiting the morbidity of a posterior approach to the knee [3]. Surgical treatment of this combination of injuries can be effectively and adequately addressed arthroscopically with typical instrumentation and techniques, such as transtibial suture fixation, avoiding the morbidity and surgical risk of a posterior approach to the knee to address the PCL fragment. Based on our interpretation of the literature available and experience with this case, it is our opinion that only arthroscopically irreducible fractures should be converted to an open procedure. Regarding post-operative care, four case reports described their protocol. Full weight-bearing was restricted in two of the four cases for 6–10 weeks [5, 7]. Range of motion was restricted for 2 [5], 4 [1, 6], or 6 weeks [7]. Our patient was allowed to weight-bear fully in a brace locked in extension immediately with the idea that body weight would increase compression of the fractures. In addition, he was allowed early, full active and passive range of motion to help maximize final range of motion and help prevent arthrofibrosis.
Concomitant ACL and PCL avulsion fractures with an associated posterior medial meniscal root avulsion is an extremely rare injury and unique to the literature. Surgical repair with standard arthroscopic techniques of reduction and trans-tibial fixation can be successful for this pattern of injury. Advantages of this treatment strategy included avoiding the risks associated with an open approach to the posterior knee to address the PCL as well as allowance of immediate full weightbearing and range of motion.
Conventionally, avulsion fractures of the ACL and particularly the PCL have been treated in an open fashion exposing the patient to increased risk during a posterior approach to the knee and increased scar tissue burden. In this case of concomitant ACL, PCL, and posterior medial meniscal avulsion fractures, an all-arthroscopic repair can be successful in both reduction and fixation, allowing for a robust repair without the morbidity of an open approach. An attempt as all arthroscopic fixations for similar injuries should be carefully considered by the treating surgeon.
References
- 1.Lombardo-Torre M, Espejo-Reina A, Garcia-Gutierrez G, Espejo-Baena A, Espejo-Reina MJ. Arthroscopic treatment of concurrent avulsion fracture of anterior and posterior cruciate ligament with suspension device. J Orthop Case Rep 2018;8:81-5. [Google Scholar]
- 2.Sanders TL, Kremers HM, Bryan AJ, Larson DR, Dahm DL, Levy BA, et al. Incidence of anterior cruciate ligament tears and reconstruction: A 21-year population-based study. Am J Sports Med 2016;44:1502-7. [Google Scholar]
- 3.Hooper PO 3rd., Silko C, Malcolm TL, Farrow LD. Management of posterior cruciate ligament tibial avulsion injuries: A systematic review. Am J Sports Med 2018;46:734-42. [Google Scholar]
- 4.Pache S, Aman ZS, Kennedy M, Nakama GY, Moatshe G, Ziegler C, et al. Meniscal root tears: Current concepts review. Arch Bone Jt Surg 2018;6:250-9. [Google Scholar]
- 5.de Souza Leao MG, Santoro ES, Avelino RL, Granjeiro RC, Junior NO. Combined anterior and posterior cruciate ligaments avulsion from the tibial side in adult patient: Case report. Rev Bras Ortop 2013;48:581-5. [Google Scholar]
- 6.Rangaswamy D, Dixit S, Jagadeeshan M. Staged primary fixation of combined bicruciate traumatic avulsion fractures from tibial eminence. Saudi J Sports Med 2016;16:156-8. [Google Scholar]
- 7.Calpur OU, Copuroglu C, Ozcan M. Avulsion fractures of both anterior and posterior cruciate ligament tibial insertions. Knee Surg Sports Traumatol Arthrosc 2002;10:223-5. [Google Scholar]
- 8.Marupaka SK, Kataria S, Jakkani R, Jampala V, Chavva S. Avulsion fractures around the knee and their importance. Int J Contemporary Med Surg Radiol 2019;4:C241-7. [Google Scholar]
- 9.Ohayon MM, Guilleminault C, Priest RG. Night terrors, sleepwalking, and confusional arousals in the general population: Their frequency and relationship to other sleep and mental disorders. J Clin Psychiatry 1999;60:268-76; quiz 277. [Google Scholar]
- 10.Sauter TC, Veerakatty S, Haider DG, Geiser T, Ricklin ME, Exadaktylos AK. Somnambulism: Emergency department admissions due to sleepwalking-related trauma. West J Emerg Med 2016;17:709-12. [Google Scholar]
- 11.Anderson CN, Anderson AF. Tibial eminence fractures. Clin Sports Med 2011;30:727-42. [Google Scholar]
- 12.Rajanish R, Jaseel M, Murugan C, Kumaran CM. Arthroscopic tibial spine fracture fixation: Novel techniques. J Orthop 2018;15:372-4. [Google Scholar]