The clinical case highlights the significance of personalised patient management and assessment of risk factors, routine radiographic follow-up, and consultation with an orthopedic surgeon as surgical options with good prosthesis stability for patients with massive periprosthetic osteolysis are limited and could not reach a good long-term prognosis.
Assoc. Prof. Peteris Studers, Joint Laboratory of Traumatology and Orthopaedics, Riga Stradins University, Riga, Latvia. E-mail: Peteris.Studers@rsu.lv
Introduction: Periprosthetic osteolysis (PPOL) is a serious complication after total hip replacement and requires immediate action to prevent further spread to nearby tissues and has the opportunity to restore hip function successfully. We present the case of PPOL of a patient with a challenging course of treatment.
Case Report: We report a 75-year-old patient with PPOL that spreads to the soft tissues and pelvic region 14 years after primary total hip arthroplasty. At all stages of treatment, an elevated neutrophil-dominant cell count was detected in the analysis of synovial fluid aspiration of the left hip joint without detection of microbiological culture. Due to severe bone loss and general patient condition, no further surgical treatment was indicated, and there is no clear vision of future actions.
Conclusion: Management of severe PPOL can be challenging, as there are limited surgical treatment options with a good long-term prognosis. If an osteolytic process is suspected, it should be treated as soon as possible to avoid more severe progression of the complications.
Keywords: Periprosthetic osteolysis, total hip replacement, bone lesion.
Periprosthetic osteolysis (PPOL) is known to be one of the leading late complications after total hip replacement (THR) [1,2,3], with aseptic loosening (AL) accounting for most of all THA revisions [3]. Osteolysis occurs due to loosening of hip replacement prostheses due to loss of adjacent bone with chronic cell-mediated inflammation that leads to osteoclastic bone resorption and suppresses bone formation [2]. For 20% of patients, this process can be asymptomatic [4], it could be challenging to determine the exact beginning of osteolysis development. On plain radiographs, osteolytic zones with bone loss are seen, but computed tomography (CT) is used to supplement the information obtained from the radiographs, providing a complete look for clinical decision making [5]. Complaints about pain and radiographically confirmed destruction around the prosthesis are the main indications for further surgical intervention [2]. We represent a 75-year-old patient with massive osteolysis that spread to the soft tissue 14 years after primary THR with a non-cemented acetabular component and polyethylene insert, which failed for revision arthroplasty and, therefore, lacks a future treatment plan. This case suggests the importance of frequent follow-up visits and timely referral to an orthopedic surgeon if there are any changes in the follow-up radiograph, even not so many years after primary surgery, to detect possible osteolytic processes.
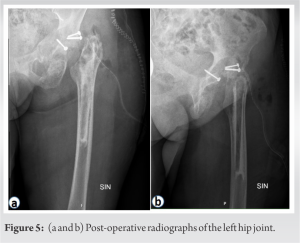
A 75-year-old woman (body mass index, 24.5 kg/m2) was admitted to the emergency department with severe abdominal pain in the left lower quadrant with diverticulitis or free fluid in the abdomen as suspected diagnosis. She also noted progressing chronic pain during the last weeks in the left hip groin and limited range of motion in the joint. Ultrasound imaging on the same day revealed fluid collection (9.7 × 4.6 × 5.0 cm) in the left lower quadrant with suspected abscess or hematoma. CT images (Fig. 1) showed a 2 cm thick destruction zone around the acetabular component of the left hip joint with signs of fragmentation and bone destruction and a noticeable spread to soft tissues-m. iliacus, with thickening, edema, and lobulated collections also spread to the inferior part of m. psoas (in the upper part of the less demarcated, in the lower part with thick, contrast-enhanced capsules (largest dimensions approximately 4.3 × 4.5 cm × 16.0 cm). 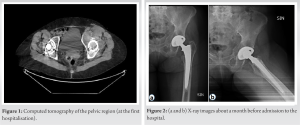
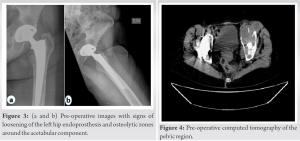
Until 30% of patients can develop osteolysis within 10 years after THR, which is more common at the femoral level [6], but in this case severe osteolysis occurred later, 14 years after primary THR and around the acetabular component. The osteolytic process does not always require operative treatment, if detected in the early stage, pharmacological treatment could be offered, such as bisphosphonates, anabolic, or human monoclonal antibody [2], which could also be used in this case for subsequent bone resorption if postmenopausal osteoporosis could be suspected. There is no information on vitamin D levels that had previously been done; therefore, an osteoporosis diagnosis could be confirmed and could be the reason for the severity of this case so quickly after primary THA. Furthermore, potential risk factors should be reviewed. The patient had a large bone cyst around the acetabular component months before severe pain began. Synovial fluid pressure within the joint may cause osteolysis, as sustained elevated pressure can alter normal bone perfusion and oxygenation, resulting in bone necrosis [7]. Furthermore, the previously reported diagnosis of C hepatitis should be considered, as there is a higher risk of osteoporosis among hepatitis C virus-infected patients [8], and these patients may have a higher risk of surgical complications and a revision rate [9]. A polyethylene insert was used and, taking into account the massive osteolytic process around the acetabulum, several authors also emphasise particle-associated wear osteolysis, which occurs when the polyethylene liner is completely worn through, the metallic femoral head now articulates with a metallic shell, and small fibrils are formed on the surface of the polymers, which can detach and accumulate in the joint cavity, activating the osteolytic cascade [2, 10, 11]. To monitor the appearance of osteolysis, a hip radiograph should be performed every 2–3 years, beginning 5 years after total hip arthroplasty [4, 12]. Radiographs are useful as a screening tool for osteolysis but may not accurately delineate the size of the lesion [4], as the patient had some signs of bone destruction, but only CT imaging revealed the degree of progression of the pathological process. There are similarities in patient complications for severe cases, worsening pain, appearance of acetabular shell loosening, and severe bone loss, leading to indications for revision surgery [13], as was similar in this case. However, if THA revision cannot be performed, at least some of the lost bone material should be restored. Although autograft is considered the gold standard for bone transplantation, it also has several limitations [7], as this patient had a limited amount of bone that could be acquired using this technique; therefore, allograft was used. Furthermore, the allograft has limited osteoinductive properties, but lacks osteogenesis and remodeling at a much slower rate [7]. Hempelvic prosthesis has shown promising results in improving function in patients after pelvic tumor resection [14], as well as being used in cases of severe PPOL [13], but in all of these cases, all patients were younger, and therefore, there could be doubts about osteointegration in this case, as the patient is older and the osteolytic process has already spread to the soft tissue. Furthermore, a cup-cage constructs for massive acetabular defect [15], but bone loss for the patient has been so severe that these options could not be used, as there are no stable bone fragments to attach to the prosthesis without risking repeated early revision surgery. Finally, it should be considered that the patient is not severely limited in mobility and can walk independently with the help of crutches. Therefore, the question remains whether any further surgical option is even an option and whether there are any cost-effective options available in such severe bone loss.
It is rare for such massive PPOL to spread to soft tissue after initial THR. Due to the patient’s age, general health condition, and severity of bone loss, surgical options were available only if good stability of the prosthesis and an excellent long-term prognosis were expected. This case indicates the importance of individual patient management and assessment of potential risk factors, routine follow-up radiographs, and a follow-up visit to an orthopedic surgeon.
In the cases of severe pain in the lower abdomen and a history of hip arthroplasty, a complication due to surgery should be suspected. Suppose that the osteolytic process has spread to the soft tissue and severe bone loss is detected. In that case, several surgical options should be considered, but at the same time, consider the patient’s participation and the best possible outcome because, in addition, non-surgical options are the only available options at the time.
References
- 1.Sheth NP, Rozell JC, Paprosky WG. Evaluation and treatment of patients with acetabular osteolysis after total hip arthroplasty. J Am Acad Orthop Surg 2019;27:e258-67. [Google Scholar]
- 2.Goodman SB, Gallo J. Periprosthetic osteolysis: Mechanisms, prevention and treatment. J Clin Med 2019;8:2091. [Google Scholar]
- 3.Pajarinen J, Gallo J, Takagi M, Goodman SB, Mjöberg B. Particle disease really does exist. Acta Orthop 2018;89:133-6. [Google Scholar]
- 4.Gallo J, Kamínek P, Zapletalová J, Cechová I, Spicka J, Ditmar R. Is osteolysis associated with a stable total hip replacement asymptomatic? Acta Chir Orthop Traumatol Cech 2004;71:20-5. [Google Scholar]
- 5.Ries MD, Link TM. Monitoring and risk of progression of osteolysis after total hip arthroplasty. J Bone Joint Surg Am 2012;94:2097-105. [Google Scholar]
- 6.Alamino RP, Casellini C, Baňos A, Schneeberger EE, Gagliardi SA, Cocco JA, et al. Prevalence of periprosthetic osteolysis after total hip replacement in patients with rheumatic diseases. Open Access Rheumatol 2012;4:57-62. [Google Scholar]
- 7.Dattani R. Femoral osteolysis following total hip replacement. Postgrad Med J 2007;83:312-6. [Google Scholar]
- 8.Wijarnpreecha K, Thongprayoon C, Panjawatanan P, Phatharacharukul P, Ungprasert P. Hepatitis C virus infection and risk of osteoporosis: A meta-analysis. Saudi J Gastroenterol 2017;23:216-21. [Google Scholar]
- 9.Issa K, Pierce TP, Harwin SF, Scillia AJ, McInerney VK, Mont MA. Does hepatitis C affect the clinical and patient-reported outcomes of primary total hip arthroplasty at midterm follow-up? J Arthroplasty 2017;32:2779-82. [Google Scholar]
- 10.Atkins GJ, Haynes DR, Howie DW, Findlay DM. Role of polyethylene particles in peri-prosthetic osteolysis: A review. World J Orthop 2011;2:93-101. [Google Scholar]
- 11.Callaghan JJ, Rosenberg AG, Rubash HE, Clohisy J, Beaule P, DellaValle C. The Adult Hip. 3rd ed. Philadelphia, PA: Wolters Kluwer; 2015. p. 1624. [Google Scholar]
- 12.Kandahari AM, Yang X, Laroche KA, Dighe AS, Pan D, Cui Q. A review of UHMWPE wear-induced osteolysis: The role for early detection of the immune response. Bone Res 2016;4:16014. [Google Scholar]
- 13.Xing D, Li R, Li JJ, Tao K, Lin J, Yan T, et al. Catastrophic periprosthetic osteolysis in total hip arthroplasty at 20 years: A case report and literature review. Orthop Surg 2022;14:1918-26. [Google Scholar]
- 14.Wang B, Xie X, Yin J, Zou C, Wang J, Huang G, et al. Reconstruction with modular hemipelvic endoprosthesis after pelvic tumor resection: A report of 50 consecutive cases. PLoS One 2015;10:e0127263. [Google Scholar]
- 15.Arvinte D, Kiran M, Sood M. Cup-cage construct for massive acetabular defect in revision hip arthroplasty-a case series with medium to long-term follow-up. J Clin Orthop Trauma 2020;11:62-6. [Google Scholar]