This article gives us insight into the rarest form of metastasis seen in a chronic myeloid leukemia patient, presenting with acute paraparesis. This clinical presentation should be always corelated with the CML remission and should never be overlooked in differential diagnosis.
Dr. Vishnu Vikraman Nair, Department of Orthopaedics, Bombay Hospital and Medical Research Institute, Mumbai, Maharashtra, India. E-mail: vishnunair212@gmail.com
Introduction: Chloromas are defined as metastatic granulocytic solid tumors of myeloid origin occurring at an extramedullary site. In this case report, we present an uncommon case of chronic myeloid leukemia (CML) presenting with metastatic sarcoma to the dorsal spine causing acute paraparesis.
Case Report: A 36-year-old male presented in the OPD with complaints of progressive upper back pain and acute paraparesis since a 1 week. The patient is a previously diagnosed case of CML on treatment for the same. MRI of the dorsal spine indicated extradural soft-tissue lesions in D5-D9 extending to the right side of the spinal canal displacing the cord to the left. Considering the acute paraparesis that the patient developed, he was taken for an emergency decompression of the tumor. Microscopy showed infiltration of fibrocartilaginous tissue of polymorphous origin mixed with atypical myeloid precursor cells. Immunohistochemistry reports show atypical cells diffusely expressing myeloperoxidase, focally expressing CD34 and CD117.
Conclusion: Rare case reports like this are the only literature available on remission in CML cases with sarcomas. The acute paraparesis in our patient was prevented from increasing to a paraplegia by surgical means. Immediate decompression of the spinal cord in patients with paraparesis and associated radiotherapy and chemotherapy should be considered in all patients with myeloid sarcomas of CML origin. While examining patients of CML, the possibility of a granulocytic sarcoma should always be kept in mind.
Keywords: Chronic myeloid leukemia, chloroma, spinal metastasis.
Chloromas are defined as metastatic granulocytic solid tumors of myeloid origin occurring at an extramedullary site, further classified into the following four categories: (i) isolated GS; (ii) GS concurrent with acute myeloid leukemia (AML); (iii) GS as a sign of blast crisis in myeloproliferative neoplasm, myelodysplastic syndrome, chronic myeloid leukemia (CML), or other myeloproliferative disorders; and (iv) GS as a relapse of AML, CML, or hematopoietic stem cell transplantation [1]. Metastatic sarcomas of myeloid origin are very uncommon to see in daily practice. It is seen that leukemia patients are unlikely to suffer from malignant spinal cord compression, which occurs in <2.5% of all leukemic patients [2]. In this case report, we present an uncommon case of CML presenting with metastatic sarcoma to the dorsal spine causing acute paraparesis.
A 36-year-old male presented in the OPD with complaints of progressive upper back pain since a 1 week. On examination in OPD, he had a progressive unsteady gait and was not able to walk more than a few steps. On clinical examination, he had severe weakness in the lower limb muscles with hip and knee joint having 1+ MRC power grade and ankle and EHL/FHL having 4+ MRC power grade. He also had hyperreflexia in both lower limbs at knee and ankle joint. The patient is a previously diagnosed case of CML on treatment for the same. MRI of the dorsal spine indicated extradural soft-tissue lesions in D5-D9 extending to the right side of the spinal canal displacing the cord to the left (Fig. 1).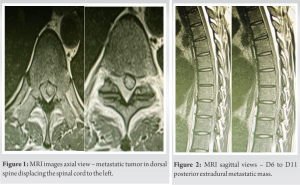 T1 hypointense and STIR hyperintense showed focal lesions found in the dorsal and lumbar vertebrae, pelvis, and both proximal femurs. Sagittal cuts of the MRI also show the extradural tumor (Fig. 2). A needle biopsy was done to rule out infective causes like endemic tuberculosis which came to be negative. Considering the acute paraparesis that the patient developed, he was taken for an emergency decompression of the tumor, which was displacing the cord to the right side. After exposure of the dorsal spine high-speed burr was used for laminectomy. Following laminectomy, the metastatic tumor was visualized under a high-definition microscope where below the layer of ligamentum flavum from D5 to D11 level, the tumor was compressing the spinal cord extradurally within the canal. Carefully, the tumor was dissected out from the dura without causing damage to the dural sac (Fig. 3). Postoperatively, the patient was immediately mobilized using a Taylors brace. An intraoperative tissue sample was collected which on microscopy showed infiltration of fibrocartilaginous tissue of polymorphous origin mixed with atypical myeloid precursor cells. Immunohistochemistry reports show atypical cells diffusely expressing myeloperoxidase (MPO), focally expressing CD34 and CD117. The IHC confirmed the probability of a metastatic sarcoma in a patient already diagnosed with CML. The patient had an improvement in gait and recovered MRC power grade in the lower limb from 4+ in ankle and EHL/EDL to 5. Postoperatively, the patient was mobilized immediately with a walker. The patient was already on nilotinib treatment for CML and was further referred to his oncology and hematology team for further chemotherapy.
T1 hypointense and STIR hyperintense showed focal lesions found in the dorsal and lumbar vertebrae, pelvis, and both proximal femurs. Sagittal cuts of the MRI also show the extradural tumor (Fig. 2). A needle biopsy was done to rule out infective causes like endemic tuberculosis which came to be negative. Considering the acute paraparesis that the patient developed, he was taken for an emergency decompression of the tumor, which was displacing the cord to the right side. After exposure of the dorsal spine high-speed burr was used for laminectomy. Following laminectomy, the metastatic tumor was visualized under a high-definition microscope where below the layer of ligamentum flavum from D5 to D11 level, the tumor was compressing the spinal cord extradurally within the canal. Carefully, the tumor was dissected out from the dura without causing damage to the dural sac (Fig. 3). Postoperatively, the patient was immediately mobilized using a Taylors brace. An intraoperative tissue sample was collected which on microscopy showed infiltration of fibrocartilaginous tissue of polymorphous origin mixed with atypical myeloid precursor cells. Immunohistochemistry reports show atypical cells diffusely expressing myeloperoxidase (MPO), focally expressing CD34 and CD117. The IHC confirmed the probability of a metastatic sarcoma in a patient already diagnosed with CML. The patient had an improvement in gait and recovered MRC power grade in the lower limb from 4+ in ankle and EHL/EDL to 5. Postoperatively, the patient was mobilized immediately with a walker. The patient was already on nilotinib treatment for CML and was further referred to his oncology and hematology team for further chemotherapy.
Burns in 1811 described a yellowish-brown tumor of unknown origin on the dura in spine. King referred to this tumor as chloroma, and Dock explained how chloroma is associated with leukemia [3]. The first ever case of chloroma was described in 1903 by Turk. Metastatic cells from myeloid origin contain more amounts of MPO, giving the typical color explained, but on exposure to air they turn gray in color as a result of oxidization [4]. Patients presenting with metastatic granulomatous tumors usually present with typical symptoms of myeloproliferative disease along with Local pain (78%), tumor nodules (65%), and sensory disturbances (52%) [5]. The occurrence of spinal cord compression has also been explained most commonly seen in thoracic spine causing back and radicular leg pain [6, 7]. Granulocytic sarcomas of leukemic origin usually tend to invade the periosteum through the Haversian canals and then spread to the dura mater [8]. Granulocytic metastasis is also seen in CNS, most commonly presenting as intracranial hemorrhage in patients who have been treated with imatinib [9]. Metastatic tumors from CML origin are known not only to metastasize to spinal cord but also to intracranial structures. Studies using CT scans report, intracranial granulocytic sarcomas have been identified with a medium to high amount of attenuation (60–80 HU) and often show a regular enhancement when exposed to contrast [10]. Some studies report the MRI features of such granulocytic tumors as isointense with white matter on both T1- and T2-weighted images. A patient presenting with a mass in the thoracic spine causing severe back pain and acute paraparesis can be due to differentials such as hematoma, abscess, meningioma, lymphoma, and metastasis. The identification of the cause is predominantly the most important factor in determining the prognosis associated with the underlying condition. Studies show that patients presenting with acute neurodeficit due to metastatic sarcoma in the spinal cord, benefit from surgical decompression more that radiotherapy [11].
Systematic treatment protocols for such cases of metastatic sarcomas of myeloid origin have not been devised yet. Rare case reports like this are the only literature available on remission in CML cases with metastatic sarcomas. The acute paraparesis in our patient was prevented from progressing to paraplegia by surgical decompression means. Immediate decompression of the spinal cord in patients with paraparesis and associated radiotherapy and chemotherapy should be considered in all patients with myeloid sarcomas of CML origin. While examining patients of CML, the possibility of a metastatic granulocytic sarcoma should always be kept in mind.
Granulocytic sarcomas of metastatic origin in chromic myeloid leukemia, even though rare are a very important clinical entity which might require aggressive treatment specially if it presents within the spinal cord causing acute paraparesis. Appropriate and timely management can prevent from complete paraplegia and also help reverse the paraparesis.
References
- 1.Han S, Li Y, Niu T, Wang X, Li Z, Ren X, et al. Granulocytic sarcoma causing long spinal cord compression: Case report and literature review. J Spinal Cord Med 2022;45:481-5. [Google Scholar]
- 2.Loblaw DA, Laperriere NJ, Mackillop WJ. A population-based study of malignant spinal cord compression in Ontario. Clin Oncol (R Coll Radiol) 2003;15:211-7. [Google Scholar]
- 3.Frohna BJ, Quint DJ. Granulocytic sarcoma (chloroma) causing spinal cord compression. Neuroradiology 1993;35:509-11. [Google Scholar]
- 4.Neiman RS, Barcos M, Berard C, Bonner H, Mann R, Rydell RE, et al. Granulocytic sarcoma: A clinicopathologic study of 67 biopsied cases. Cancer 1981;48:1426-37. [Google Scholar]
- 5.Liu PI, Mcgregor DH, Okada H, Steer A. Autopsy study of granulocytic sarcoma (chloroma) in patients with myelogenous leukemia, Hiroshima-Nagasaki 1949-1969. Cancer 1973;31:948-55. [Google Scholar]
- 6.O’Brien CE, Saratsis AM, Voyadzis JM. Granulocytic sarcoma in a patient with blast crisis mimicking a chronic subdural hematoma. J Clin Oncol 2011;29:e569-71. [Google Scholar]
- 7.Campo E, Swerdlow SH, Harris NL, Pileri S, Stein H, Jaffe ES. The 2008 WHO classification of lymphoid neoplasms and beyond: Evolving concepts and practical applications. Blood 2011;117:5019-32. [Google Scholar]
- 8.Barnett MJ, Zussman WV. Granulocytic sarcoma of the brain: A case report and review of the literature. Radiology 1986;160:223-5. [Google Scholar]
- 9.Song KW, Rifkind J, Al-Beirouti B, Yee K, McCrae J, Messner HA, et al. Subdural hematomas during CML therapy with imatinib mesylate. Leuk Lymphoma 2004;45:1633-6. [Google Scholar]
- 10.Klimo P Jr., Thompson CJ, Kestle JR, Schmidt MH. A meta-analysis of surgery versus conventional radiotherapy for the treatment of metastatic spinal epidural disease. Neuro Oncol 2005;7:64-76. [Google Scholar]











