Consider acute exertional compartment syndrome of the medial foot in a patient with severe atraumatic medial foot pain, swelling, and tenderness.
Dr. Benjamin Diedring, Department of Orthopaedic Surgery, Ascension Macomb-Oakland Hospital, 27351 Dequindre Rd, Madison Heights, Michigan 48071. E-mail: Benjamin.Diedring@ascension.org
Introduction: Acute compartment syndrome is a surgical emergency that is mainly diagnosed clinically. Acute exertional compartment syndrome of the medial compartment of the foot is a rare condition most often result from strenuous exercise. Early diagnosis is most often a clinical examination, however, laboratory and magnetic resonance imaging (MRI) can assist in the diagnosis if clinician uncertainty persists. We present a case report of acute exertional compartment syndrome of the medial compartment of the foot after physical activity.
Case Report: A 28-year-old male presents to the emergency department the day after playing basketball, with severe atraumatic medial foot pain. Clinical examination demonstrated tenderness and swelling over the medial arch of the foot. Creatine phosphokinase (CPK) results at 9500 international units. MRI demonstrated fusiform edema of the abductor hallucis. Subsequent fasciotomy revealed protruding muscle during fascial incision and relieved the patient of their pain. Return to surgery 48 h after initial fasciotomy revealed gray discoloration and lack of contractility of the muscle tissue. The patient was recovering well at the first post-operative visit, however, was lost to follow-up thereafter.
Conclusion: Acute exertional compartment syndrome of the medial compartment of the foot is a rarely reported diagnosis, likely due to a combination of missed diagnosis and underreporting. Laboratory tests for CPK may be elevated, and MRI may be helpful in the diagnosis of this condition. Fasciotomy of the medial compartment of the foot relieved the patient’s symptoms, and to our knowledge had a good outcome.
Keywords: Compartment syndrome, foot, medial compartment, abductor halluces.
Acute compartment syndrome is a common condition due to increased pressure in a closed myofascial compartment that serves as a surgical emergency to prevent irreversible tissue ischemia. The diagnosis is most often made by clinical suspicion with pain out of proportion to physical examination findings acting as the principle and often first finding. Other clinical examination findings include pain on passive stretching, pallor, pulselessness, paralysis, and paresthesia. Compartment pressures may also be measured, and a delta pressure (pre-operative diastolic blood pressure minus intracompartmental pressure) of <30 serves as the most common threshold for compartment syndrome diagnosis. Trauma represents the most common cause of compartment syndrome, but several other causes have also been documented [1]. We present a unique case of atraumatic exertional compartment syndrome in the medial foot. Case review found only nine similarly reported cases dating back to 1995. Of these cases, eight were exertional and one resulted as an unusual complication of spine surgery [2, 3, 4, 5, 6, 7, 8, 9, 10].
The patient is a 28-year-old male whose prior medical history includes only morbid obesity and smoking tobacco. He presented to the emergency department for right foot pain. He stated he was playing basketball the day before the presentation and was painless throughout the entirety of the day. He denied injuries to the foot or ankle. When he awoke the next morning, he felt severe spastic pain to the medial aspect of his foot with intermittent radiation to the knee. Physical examination revealed focal tenderness and moderate swelling over the medial arch of the foot, with soft, compressible, and painless compartments on the dorsum and plantar aspect of the foot. No other apparent swelling or pain was noted on the foot. The patient was able to actively flex and extend his great toe, and the passive range of motion of the toes did not increase pain unless the first metatarsal was flexed. Dorsalis pedis and posterior tibial pulses were strong and palpable. The sensory examination was normal throughout the extremity. Radiographic imaging of the foot and ankle demonstrated no osseous injuries; however, it was noted the patient had an os trigonum (Fig. 1), and a Geist Type 1 os navicularum (Fig. 2) [11]. Initial blood draws resulted in a creatine phosphokinase (CPK) of 9,500 international units (IU) without elevated creatinine or potassium. The patient was placed in an observation unit for pain control and monitoring due to the abnormal presentation, with high suspicion remaining for possible musculotendinous injury and lower suspicion for compartment syndrome. During this day of observation, the patient’s pain began to worsen. Magnetic resonance imaging (MRI) of the foot and ankle demonstrated fusiform edema in the proximal portion of the abductor hallucis muscle belly and proximal tendon without evidence of tear. 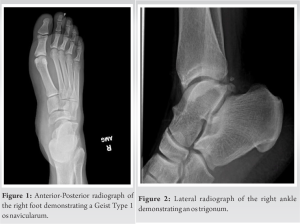 These findings are demonstrated in Fig. 3a, b, and c. Subsequent fasciotomy over the abductor hallucis muscle belly demonstrated obvious muscle expansion from the fasciotomy incision and grayish discoloration consistent with avascular injury. The incision was carried distally to the metatarsal head and proximally to the calcaneal insertion, measuring approximately 18 cm. The surgeon noted improvement in discoloration suggesting reperfusion of the muscle belly, as well as contractility of the muscle. Irrigation was performed and a negative pressure dressing at 125 mmHg of suction was placed with the intention to return within 48–72 h for re-evaluation of the tissue viability, irrigation, debridement, and potential wound closure. Following surgery, the patient reported significantly decreased pain. The patient returned to the operating room 48 h after the index procedure and 5 days from injury for irrigation, debridement, and wound closure. The proximal aspect of the muscle was necrotic, non-contractile, and without bleeding on excisional debridement. Much of the proximal muscle belly was excised. The distal muscle belly remained healthy and bleeding and was retained. The swelling had largely subsided, and primary wound closure was successful with the aid of an incisional negative pressure dressing. On post-operative day 1, the patient tolerated the procedures well, without complication, and the pain was controlled with oral narcotics. The incisional negative pressure dressing was removed, and the patient was subsequently discharged in the evening. The patient’s CPK decreased to 1300 IU by discharge, and there was no elevation in creatinine or potassium throughout the duration of the hospital stay. The patient had a delayed first post-operative follow-up at 4 weeks post-operative. At this time, the patient’s pain was appropriately controlled with intermittent paresthesias present over the medial aspect of the foot. The patient was prescribed 300mg gabapentin TID for neuropathic pain. A CAM boot was provided, and the patient was encouraged to weight bear as tolerated while in the boot. The surgical site demonstrated continued wound healing and staples were not removed. The patient was to return in 2 weeks for wound check and staple removal but was lost to follow-up and presumed to be doing well.
These findings are demonstrated in Fig. 3a, b, and c. Subsequent fasciotomy over the abductor hallucis muscle belly demonstrated obvious muscle expansion from the fasciotomy incision and grayish discoloration consistent with avascular injury. The incision was carried distally to the metatarsal head and proximally to the calcaneal insertion, measuring approximately 18 cm. The surgeon noted improvement in discoloration suggesting reperfusion of the muscle belly, as well as contractility of the muscle. Irrigation was performed and a negative pressure dressing at 125 mmHg of suction was placed with the intention to return within 48–72 h for re-evaluation of the tissue viability, irrigation, debridement, and potential wound closure. Following surgery, the patient reported significantly decreased pain. The patient returned to the operating room 48 h after the index procedure and 5 days from injury for irrigation, debridement, and wound closure. The proximal aspect of the muscle was necrotic, non-contractile, and without bleeding on excisional debridement. Much of the proximal muscle belly was excised. The distal muscle belly remained healthy and bleeding and was retained. The swelling had largely subsided, and primary wound closure was successful with the aid of an incisional negative pressure dressing. On post-operative day 1, the patient tolerated the procedures well, without complication, and the pain was controlled with oral narcotics. The incisional negative pressure dressing was removed, and the patient was subsequently discharged in the evening. The patient’s CPK decreased to 1300 IU by discharge, and there was no elevation in creatinine or potassium throughout the duration of the hospital stay. The patient had a delayed first post-operative follow-up at 4 weeks post-operative. At this time, the patient’s pain was appropriately controlled with intermittent paresthesias present over the medial aspect of the foot. The patient was prescribed 300mg gabapentin TID for neuropathic pain. A CAM boot was provided, and the patient was encouraged to weight bear as tolerated while in the boot. The surgical site demonstrated continued wound healing and staples were not removed. The patient was to return in 2 weeks for wound check and staple removal but was lost to follow-up and presumed to be doing well.
Acute compartment syndrome of the foot typically presents due to a high-energy bony or soft-tissue injury [10]. Much less common is the presentation secondary to exertional injury, with only eight cases in the medial compartment of the foot [3, 4, 5, 6, 7, 8, 10]. This case represents the third after playing basketball, while others presented after soccer, a marathon, rugby practice, aerobics class, and a football game [3, 4, 5, 6, 7, 8, 9, 10]. Although there has been debate on how to classify the compartments of the foot, the consensus persists that there are nine compartments broken into four groups for surgical management: The intrinsic, central, lateral, and medial compartments [6, 7, 12]. This case demonstrates clinical and MRI findings of fusiform edema isolated to the abductor hallucis without bony or soft-tissue trauma, suggesting a diagnosis of compartment syndrome of the medial foot. This finding correlates with the four other cases of exertional medial compartment syndrome of the foot that used MRI to aid in diagnosis [3, 4, 6, 7]. While MRI findings played a major part in formulating a diagnosis of our patient, compartment syndrome is traditionally diagnosed by clinical examination alone or by measuring intracompartmental pressure. Clinical examination alone is often sufficient to diagnose compartment syndrome in other areas of the body demonstrating the 6 P’s of: Pain out of proportion to physical examination, pain with passive stretch, pulselessness, paralysis, paresthesia, and pallor [13]. Others advocate for the necessity of measuring compartment pressures. Normal resting muscle compartment pressures measure <10 mmHg. When this pressure increases to 20–30 mmHg within the patient’s diastolic blood pressure, a diagnosis of compartment syndrome can be made. However, in the case of our patient, clinical suspicion for compartment syndrome was low due to the lack of trauma and overall low incidence of medial compartment syndrome of the foot. An MRI was ordered, as there was a concern for a musculotendinous injury, and ultimately used along with a clinical examination to diagnose compartment syndrome. Once the diagnosis of compartment syndrome was made, the patient was brought to the operating room for fasciotomy over the medial compartment of the foot. This treatment is consistent with 8 of the 9 other reported cases of atraumatic exertional medial compartment syndrome of the foot [2, 3, 4, 5, 6, 7, 8, 9, 10]. Atraumatic exertional compartment syndrome of the medial foot presents a challenging clinical diagnosis as few cases have been reported in the literature [3, 4, 5, 6, 7, 8, 9, 10]. However, timely identification of this condition decreases the risk of ischemic injury and its sequela. While diagnosis can be made using clinical examination and measurement of compartment pressures, MRI also can be used as a valuable way to diagnose this potentially devastating condition. Although it is important to associate acute compartment syndrome with trauma, it is equally important to note that it can be due to a multitude of etiologies and should be included on the differential whenever patients present with pain out of proportion to their physical examination.
Acute exertional compartment syndrome of the medial compartment of the foot is a rarely reported diagnosis, likely due to a combination of missed diagnosis and underreporting. To date, there have been 10 reported cases of acute exertional compartment syndrome of the medial compartment of the foot, including this case report. Most are a result of athletic activity, and present with medial-sided foot pain and tenderness. Laboratory tests for CPK may be elevated, as in this reported case. MRI may be helpful in the diagnosis of this condition and will reveal fusiform edema throughout the muscle belly or musculotendinous junction without evidence of a tear. Fasciotomy of the medial compartment of the foot relieved the patient’s symptoms, and to our knowledge had a good outcome.
Acute exertional compartment syndrome of the medial compartment of the foot is a rare condition that may be missed due to its low incidence. It is important to consider compartment syndrome in an athlete with acute medial-sided foot pain and tenderness without associated injury. CPK and MRI are instrumental in supporting the differential diagnosis of compartment syndrome of the medial compartment of the foot.
References
- 1.McMillan TE, Gardner WT, Schmidt AH, Johnstone AJ. Diagnosing acute compartment syndrome-where have we got to? Int Orthop 2019;43:2429-35. [Google Scholar]
- 2.Stotts AK, Carroll KL, Schafer PG, Santora SD, Branigan TD. Medial compartment syndrome of the foot: An unusual complication of spine surgery. Spine (Phila Pa 1976) 2003;28:E118-20. [Google Scholar]
- 3.Park YH, Ahn JH, Choi GW, Kim HJ. Exertional medial compartment syndrome of the foot-referred pain and sequelae of delayed diagnosis: A case report. Clin J Sport Med 2019;29:e83-5. [Google Scholar]
- 4.Miozzari HH, Gerard R, Stern R, Toman J, Assal M. Acute, exertional medial compartment syndrome of the foot in a high-level athlete: A case report. Am J Sports Med 2008;36:983-6. [Google Scholar]
- 5.Lam SK, McAlister J, Oliver N, Pontell D. Bilateral medial foot compartment syndrome after an aerobics class: A case report. J Foot Ankle Surg 2012;51:652-5. [Google Scholar]
- 6.Kelsey NR, Edmonds LD, Biko DM. Acute exertional medial compartment syndrome of the foot in a teenager. Radiol Case Rep 2015;10:1092. [Google Scholar]
- 7.Chambers L, Hame SL, Levine B. Acute exertional medial compartment syndrome of the foot after playing basketball. Skeletal Radiol 2011;40:931-5. [Google Scholar]
- 8.Blacklidge DK, Kurek JB, Soto AD, Kissel CG. Acute exertional compartment syndrome of the medial foot. J Foot Ankle Surg 1996;35:19-22. [Google Scholar]
- 9.Middleton DK, Johnson JE, Davies JF. Exertional compartment syndrome of bilateral feet: A case report. Foot Ankle Int 1995;16:95-6. [Google Scholar]
- 10.Myerson MS, Berger BI. Isolated medial compartment syndrome of the foot: A case report. Foot Ankle Int 1996;17:183-5. [Google Scholar]
- 11.Geist ES. Supernumerary bone of the foot: A roentgen study of the feet of 100 normal individuals. Am J Orthop Surg 1914;12:40. [Google Scholar]
- 12.Faymonville C, Andermahr J, Seidel U, Müller LP, Skouras E, Eysel P, et al. Compartments of the foot: Topographic anatomy. Surg Radiol Anat 2012;34:929-33. [Google Scholar]
- 13.Tzioupis C, Cox G, Giannoudis PV. Acute compartment syndrome of the lower extremity: An update. Orthop Trauma 2009;23:433-40. [Google Scholar]










