Closed reduction and K-wire fixation in a case of volar carpometacarpal joint dislocation in a pediatric patient are effective methods of treatment which can result in an excellent functional outcome.
Dr. Seung Il Choi, Department of Orthopedics, Whakatane Hospital, Whakatane, New Zealand. E-mail: samuelchoi94@gmail.com
Introduction: Carpometacarpal joint (CMCJ) dislocations are a rare presentation and a volar dislocation in a pediatric patient even more so. We present a case of this condition along with management strategies to help guide future treatment of this injury.
Case Report: A fit and well 8-year-old boy presented with pain and deformity of his right hand following a fall from a horse. He had no history of previous trauma or injury to this hand. X-rays demonstrated a volar dislocation of the second CMCJ, along with several metacarpal base fractures. This injury was managed emergently with closed reduction in the Emergency Department and then underwent definitive treatment through percutaneous Kirschner wire (K-wire) fixation 2 days after injury. At 3- month follow-up, the patient and his family reported no pain, and on examination, there was no deformity and he had excellent range of motion. The patient had already returned to horse riding with no issues.
Conclusion: A volar carpometacarpal dislocation in a pediatric patient is an uncommon presentation. We were able to achieve a full functional recovery using a mixture of closed reduction and K-wire fixation techniques. This clinical experience offers several learning points and also guidance around management strategies for future presentations of this condition.
Keywords: Carpometacarpal joint, dislocation, Kirschner wires, pediatric.
Carpometacarpal joint (CMCJ) dislocation is a relatively rare injury, representing approximately 1% of hand trauma injuries [1, 2]. This prevalence decreases even further when considering the injury in this case report, an isolated volar dislocation of a second CMCJ in a child [3]. Published case reports mostly focus on adult or adolescent injuries [4, 5, 6], and there is a paucity of literature in regard to the management options and outcomes of treatment strategies in this injury. Previous case reports have managed these conditions with a mixture of Kirschner wire (K-wire) and plate fixation, with varying results. This case report describes an unusual case of volar CMCJ dislocation. It also described the initial management strategies, definitive treatment decisions, and also final patient outcomes.
This study describes the case of a fit and well, 8-year-old boy, who presented to the emergency department following a fall from a horse and sustaining an injury to his right hand. On examination, the index finger was deviated radially and the hand was swollen. It was a closed injury with no neurovascular deficit. Plain radiographs taken at this time demonstrated multiple MC base fractures and an isolated volar dislocation of the second CMCJ (Fig. 1). 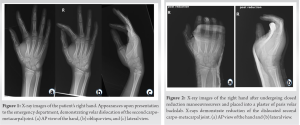 The patient underwent conscious sedation and the second CMCJ was reduced uneventfully (Fig. 2). This reduction was achieved with the application of axial traction and pressure over the volar aspect of the second metacarpal (MC) base with countertraction. A subsequent CT scan demonstrated fractures of the second, third, and fifth MC bases with buckling of the fourth MC base. The second CMCJ had minor incongruity and all the other CMCJs were well enlocated (Fig. 3).
The patient underwent conscious sedation and the second CMCJ was reduced uneventfully (Fig. 2). This reduction was achieved with the application of axial traction and pressure over the volar aspect of the second metacarpal (MC) base with countertraction. A subsequent CT scan demonstrated fractures of the second, third, and fifth MC bases with buckling of the fourth MC base. The second CMCJ had minor incongruity and all the other CMCJs were well enlocated (Fig. 3). Given the perceived instability of this injury and its unusual nature, informed consent was received from the patient’s parents for examination under anesthesia +/− percutaneous fixation +/− open reduction and internal fixation depending on the degree of intra-operative stability. In theater, the second CMCJ was stable on examination, which was confirmed with intra-operative image intensifier use during joint stress maneuvers. Axial loading and dorsal pressure were applied to reduce the incongruity of the second CMCJ seen on CT before fixation with 2 percutaneous 1.6 -mm K-wires was performed – one wire through the second MC into the capitate and the other through the fifth MC into the hamate and capitate (Fig. 4). These wires were cut and left proud. The patient was placed into a plaster of Paris backslab. At subsequent clinic visits, radiographs demonstrated stable fixation. The K-wires were removed 4- week post-operatively and the total period of cast immobilization was 6 weeks. Radiographs at this point also demonstrated satisfactory healing and maintenance of reduction (Fig. 5).
Given the perceived instability of this injury and its unusual nature, informed consent was received from the patient’s parents for examination under anesthesia +/− percutaneous fixation +/− open reduction and internal fixation depending on the degree of intra-operative stability. In theater, the second CMCJ was stable on examination, which was confirmed with intra-operative image intensifier use during joint stress maneuvers. Axial loading and dorsal pressure were applied to reduce the incongruity of the second CMCJ seen on CT before fixation with 2 percutaneous 1.6 -mm K-wires was performed – one wire through the second MC into the capitate and the other through the fifth MC into the hamate and capitate (Fig. 4). These wires were cut and left proud. The patient was placed into a plaster of Paris backslab. At subsequent clinic visits, radiographs demonstrated stable fixation. The K-wires were removed 4- week post-operatively and the total period of cast immobilization was 6 weeks. Radiographs at this point also demonstrated satisfactory healing and maintenance of reduction (Fig. 5).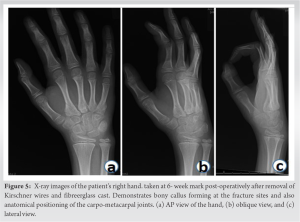 At 3- month post-operative follow-up, the patient and his family reported no pain and no functional losses. Examination demonstrated well-healed wire site scars, no deformity of the hand, stable CMCJs to manual stressing, and full range of motion of the hand and wrist compared to the contralateral side (Fig. 6).
At 3- month post-operative follow-up, the patient and his family reported no pain and no functional losses. Examination demonstrated well-healed wire site scars, no deformity of the hand, stable CMCJs to manual stressing, and full range of motion of the hand and wrist compared to the contralateral side (Fig. 6).
Injuries to the upper extremity are an extremely common orthopedic presentation, comprising 20–40% of injuries which present to the emergency department [7, 8]. While some injuries have clear guidelines on management strategies and their expected outcomes, others, such as this unusual case of volar second CMCJ dislocation, do not. CMCJ stability is composed of a variety of factors including the interlocking nature of the surrounding saddle joints, various ligamentous structures (dorsal, volar, and inter-MC ligaments), other encompassing soft tissues such as the flexor and extensor tendons, and also the intrinsic muscles of the hand. All these structures in conjunction provide excellent stability and resistance to dislocation [9]. The overall principle of CMCJ dislocation management while not widely researched follows general dislocation management: To restore the normal articular anatomy, maintain the reduction, and allow early range of motion of the digits, with the long-term aim to reduce the chance of post-traumatic arthritis, particularly in this child. Varieties of treatment options exist which range from free mobilization to open reduction and internal fixation. There is published literature which has looked into a comparison of various treatment modalities including K-wire fixation and plate fixation. Bao et al. [6] compared plate fixation to K-wire fixation utilizing the Michigan Hand Outcomes Questionnaire (MHQ score) and also the disabilities of arm, shoulder, and hand (DASH score), however this study was not focused on the pediatric population or volar dislocations specifically. This study found that the average DASH and MHQ scores in the K-wire group were superior to the plate fixation group. K-wire fixation has also been the preferred modality of treatment choice in other literature describing these injuries [10, 11]. There have been multiple studies which have investigated the non-operative outcomes of CMCJ dislocations. Zhang et al. [11] managed patients with CMCJ dislocations with closed reduction and if reduction was not able to be achieved, proceeding to open reduction and internal fixation. In general, older injuries were more difficult to achieve closed reduction; however, there were cases of patients with 6–7- week-old injuries managed purely non- operatively. However, patients with subacute injuries that were managed non-operatively had worse MHQ scores than those that were managed operatively. In this case, closed reduction of the dislocation was achieved and then maintained effectively using K-wire fixation. After a period of immobilization and post-operative recovery, the functional outcome was excellent. In summary, the literature is clear that diagnosis at initial presentation is paramount to minimize the likelihood of poorer functional outcomes [11]. Management with early initial reduction maintained with effective immobilization is required. Inability to achieve closed reduction or the degree of associated soft tissue and bony injuries may indicate that more definitive fixation is necessary with either K-wires or plate fixation. K-wires seem to result in better functional outcomes than plate fixation [6]. Volar CMCJ dislocations are an uncommon injury pattern and there are no studies or case reports that we could find that look at this injury in the pediatric population. This case highlights the decision-making orthopedist encounter when faced with an injury that has no clear guidance on treatment in a specific population. It is clear that more research and investigation are required into the outcomes of treatment strategies for CMCJ dislocation in pediatric patients to be able to provide patients and their families a better understanding of potential functional capacity following various management options.
This case demonstrates a treatment strategy for a rare orthopedic condition which has resulted in a fantastic functional outcome for the patient. These management decisions were made by applying principles of fracture dislocation management to this specific injury without availability of any published literature which describes this injury in detail. This is the first report of a volar CMCJ dislocation in the pediatric population and will provide guidance on future treatment of this presentation.
A volar CMCJ dislocation in children is extremely rare. Anatomical closed reduction and percutaneous K-wire fixation resulted in a great functional and cosmetic outcome for this patient and have been well demonstrated in this case.
References
- 1.Reinsmith LE, Garcia-Elias M, Gilula LA. Traumatic axial dislocation injuries of the wrist. Radiology 2013;267:680-9. [Google Scholar]
- 2.Pundkare GT, Deshpande SS. Proposal for a radiological classification system for carpo-metacarpal joint dislocations with or without fractures. Malays Orthop J 2018;12:42-6. [Google Scholar]
- 3.Yadav SK, Nayak B, Mittal S. New approach to second metacarpophalangeal joint dislocation management: The SKY needling technique. Eur J Orthop Surg Traumatol 2021;31:189-92. [Google Scholar]
- 4.Light TR, Ogden JA. Complex dislocation of the index metacarpophalangeal joint in children. J Pediatr Orthop 1988;8:300-5. [Google Scholar]
- 5.Jilani LZ, Abbas M, Goel S, Akhtar MN. Multiple volar dislocations of the carpometacarpal joints with an associated fracture of the first metacarpal base. Chin J Traumatol 2014;17:38-40. [Google Scholar]
- 6.Bao B, Zhu H, Zheng X. Plate versus Kirschner wire fixation in treatment of fourth and fifth carpometacarpal fracture-dislocations: A retrospective cohort study. Int J Surg 2018;52:293-6. [Google Scholar]
- 7.Karl JW, Olson PR, Rosenwasser MP. The epidemiology of upper extremity fractures in the United States, 2009. J Orthop Trauma 2015;29:e242-4. [Google Scholar]
- 8.Banerjee M, Bouillon B, Shafizadeh S, Paffrath T, Lefering R, Wafaisade A, et al. Epidemiology of extremity injuries in multiple trauma patients. Injury 2013;44:1015-21. [Google Scholar]
- 9.Gurland M. Carpometacarpal joint injuries of the fingers. Hand Clin 1992;8:733-44. [Google Scholar]
- 10.Kleinman WB, Grantham SA. Multiplevolar carpometacarpal joint dislocation. Case report of traumatic volar dislocation of the medial four carpometacarpal joint in a child and review of the literature. J Hand Surg Am 1978;3:377-82. [Google Scholar]
- 11.Zhang C, Wang H, Liang C, Yu W, Li Y, Shang R, et al. The effect of timing on the treatment and outcome of combined fourth and fifth carpometacarpal fracture dislocations. J Hand Surg Am 2015;40:2169-75.e1. [Google Scholar]








