Tibial tuberosity avulsion fractures are one of the rare physeal injury seen in adolescent age group. Adequate knowledge of the pathology along with judicious evaluation and timely management is a key for a successful outcome in these rare injuries.
Dr. Gopinath Venunathan, Department of Orthopaedics, Military Hospital Roorkee, Roorkee, Uttarakhand, India. E-mail: gopiblue90@gmail.com
Introduction: Tibial tuberosity avulsion fractures in adolescents are one of the rare physeal injuries. Sudden powerful contraction of quadriceps muscle leads to avulsion fractures and varying degrees of disruption of extensor mechanism.
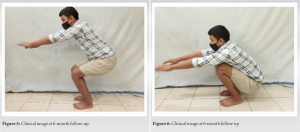
Case Report: A 16-year-old boy sustained tibial tuberosity avulsion fracture while playing football and presented with sudden onset of pain, massive swelling, and loss of active extension of the left knee along with inability to bear weight on the left leg. Due to imminent risk of development of compartment, patient was taken for surgical correction immediately. Open reduction and internal fixation were done using 02 × 4 mm partially threaded cannulated cancellous screws. Patient was immobilized with above knee cast and kept non-weight bearing for 6 weeks. Later, gradual weight bearing ambulation was allowed and ROM and strengthening of knee was carried out. Patient had regained complete ROM of knee and returned to sporting activities by end of 6 months.
Conclusion: Tibial tuberosity avulsion fractures are a rare occurrence and even rarer is them getting complicated by compartment syndrome. A high index of suspicion for development of compartment syndrome in an avulsion fracture of tibial tuberosity and a timely management can avert such potential complications and enables to achieve an optimal results.
Keywords: Avulsion, fracture, tibia, adolescents, tuberosity.
Tibial tuberosity avulsion fracture is an uncommon fracture with reported incidence rates of 0.4–2.7% of all epiphyseal injuries and <1% of all physeal injuries [1]. Demorgan was first to report a case of an acute tibial tubercle avulsion fracture (TTAF) in an adolescent in 1853. Tibial tuberosity avulsion fractures predominantly occur in an adolescent male typically in well-developed, muscular, and athletic individual nearing skeletal maturity (age 14–17 years). High jumping and basketball are the sport’s most commonly associated with this injury; however, it is also reported in other sports such as springboard diving, football, and gymnastics [2, 3].
A 16-year-old boy while playing football suddenly developed acute onset of pain in the left knee and inability to bear weight on the left leg while he ran and kicked the ball in his right foot. Patient was brought to emergency immediately. On presentation, patient had massive swelling of the left knee mainly at infrapatellar region along with tenderness and loss of active extension. Proximal half of the leg was swollen and tense in anterior aspect with no open injuries and neurovascular deficit. X-ray shown an Ogden Type IV fracture of tibial tuberosity (Fig. 1).
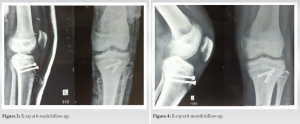
TTAF is a rare condition accounting for <1% of all physeal injuries frequently occurring in adolescent male [4]. Commonly, the mechanism of injury is due to a violent contraction of quadriceps during extension when jumping or instant knee flexion opposed to quadriceps contraction during landing on the ground [5]. Ehrenborg and Engfeldt divided tibial tubercle development into four stages: Cartilaginous, apophyseal, epiphyseal, and bony [6]. Ogden et al. showed the existence of three histologic zones in the tibial tubercle growth plate. Before physeal closure, there is a progressive change from fibrocartilage to columnar cartilage from proximal to distal in the tubercle physis creating a weakened zone. Moreover, also the proximal tibial physis closure begins in the center and extends centrifugally and then distally to involve the tubercle [7]. These characteristic changes predispose to avulsion injury of the tibial tuberosity just before or during the later stages of physiologic epiphysiodesis. Watson-Jones was first to present the classification system for acute fractures of the tibial tuberosity which was later modified by Ogden et al. into three types along with sub types A and B. Type I consists of a separation through the distal physis under the tubercle through the secondary ossification center of the tubercle. In Type II, the separation extends anteriorly through the area bridging the ossification centers of the tubercle and proximal tibial epiphysis. In Type III, the separation beneath the tubercle propagates proximally through the tibial epiphysis into the knee joint. Subtype A fractures are un displaced whereas Subtype B are displaced or comminuted [3]. Later, Type IV fracture was suggested by Ryu and Debenham to describe an avulsion fracture of the entire proximal tibial physis [8]. Frankl et al. described fractures associated with avulsions of the patellar tendon as Type 1C [9]. Recently McKoy and Stanitski added the Type V fractures which consists Type IIIB fracture with an associated Type IV fracture making a Y shaped configuration [10]. Fracture pattern in our case is an unique variant of Type IV of Ogden classification as the fracture exits through posterior metaphysis representing a Salter-Harris Type II pattern. The presence of posterior metaphyseal fragment also increases the incidence of complication rates as described by Brey et al. [11]. Restoration of extensor mechanism and maintenance of congruency of the tibial articular surface forms the goals of management. Non-operative treatment in the form of closed reduction and cylinder cast immobilization is recommended for Types IA, IB, and IIA tibial tubercle fractures [10]. Open reduction and internal fixation is recommended for Types IIB, IIIA, IIIB, and IV avulsion fractures of the tibial tuberosity along with repair of associated quadriceps or patellar tendon avulsions. Tension band wiring or cannulated screw fixation are most commonly recommended methods of fixation [2, 3, 12]. Periosteal suture fixation is advised in less mature patients (Tanner stage 1 or 2) for fear of premature physeal closure and resultant genu recurvatum or coronal plane deformity. Compartment syndrome one of a dreaded complication following this fractures was reported in <5% of patients hypothesized due to tearing of the anterior tibial recurrent vessels [13] However, an incidence as high as 20% was reported by Frey et al. [14]. Other complications includes genu recurvatum, loss of flexion, non-union, malunion, skin necrosis, patella baja, saphenous nerve neuroma, and deep venous thrombosis with pulmonary embolism [8, 15].
Recognition of a tibial tuberosity avulsion fracture along with a high index of suspicion for development of complications like compartment syndrome and a timely management can avert such potential complications and enables to achieve an optimal results.
Tibial tuberosity avulsion fracture is a relatively uncommon fracture seen mostly in adolescent age group. However, an early recognition of associated injuries and complications and timely management can provide excellent outcomes in these fractures.
References
- 1.Sibley SW. Fracture of the tubercle of the tibia by the muscular action of the rectus femoris. In: Medical Times & Gazette. Vol. 6,p. 268-9,1853. [Google Scholar]
- 2.Hand WL, Hand CR, Dunn AW. Avulsion fractures of the tibial tubercle. J Bone Joint Surg Am 1971;53:1579-83. [Google Scholar]
- 3.Ogden JA, Tross RB, Murphy MJ. Fractures of the tibial tuberosity in adolescents. J Bone Joint Surg Am 1980;62:205-15. [Google Scholar]
- 4.Shelton WR, Canale ST. Fractures of the tibia through the proximal tibial epiphyseal cartilage. J Bone Joint Surg Am 1979;61:167-73. [Google Scholar]
- 5.Abalo A, Akakpo-numado KG, Dossim A, Walla A, Gnassingbe K, Tekou AH. Avulsion fractures of the tibial tubercle. J Orthop Surg (Hong Kong) 2008;16:308-11. [Google Scholar]
- 6.Ehrenborg G, Engfeldt B. The insertion of the ligamentum patellae on the tibial tuberosity. Some views in connection with the Osgood-Schlatter lesion. Acta Chir Scand 1961;121:491-9. [Google Scholar]
- 7.Ogden JA, Hempton RJ, Southwick WO. Development of the tibial tuberosity. Anat Rec 1975;182:431-45. [Google Scholar]
- 8.Ryu RK, Debenham JO. An unusual avulsion fracture of the proximal tibial epiphysis. Case report and proposed addition to the Watson-Jones classification. Clin Orthop Relat Res 1985 Apr;(194):181-4. [Google Scholar]
- 9.Frankl U, Wasilewski SA, Healy WL. Avulsion fracture of the tibial tubercle with avulsion of the patellar ligament. Report of two cases. J Bone Joint Surg Am 1990;72:1411-3. [Google Scholar]
- 10.McKoy BE, Stanitski CL. Acute tibial tubercle avulsion fractures. Orthop Clin North Am 2003;34:397-403. [Google Scholar]
- 11.Brey JM, Conoley J, Canale ST, Beaty JH, Warner WC Jr., Kelly DM, et al. Tibial tuberosity fractures in adolescents: Is a posterior metaphyseal fracture component a predictor of complications? J Pediatr Orthop 2012;32:561-6. [Google Scholar]
- 12.Chow SP, Lam JJ, Leong JC. Fracture of the tibial tubercle in the adolescent. J Bone Joint Surg Br 1990;72:231-4. [Google Scholar]
- 13.Wiss DA, Schilz JL, Zionts L. Type III fractures of the tibial tubercle in adolescents. J Orthop Trauma 1991;5:475-9. [Google Scholar]
- 14.Frey S, Hosalkar H, Cameron DB, Heath A, David Horn B, Ganley TJ. Tibial tuberosity fractures in adolescents. J Child Orthop 2008;2:469-74. [Google Scholar]
- 15.Pesl T, Havranek P. Acute tibial tubercle avulsion fractures in children: Selective use of the closed reduction and internal fixation method. J Child Orthop 2008;2:353-6. [Google Scholar]