The pre-operative assessment should not be neglected by any member of the surgical team and conducting it in a haphazard way may result in unforeseen complications for the patient.
Mr. John P Avendano, Department of Orthopaedic Surgery, Robert Wood Johnson University Hospital, 125 Paterson Street, New Brunswick, New Jersey 08901. E-mail: ja1145@rwjms.rutgers.edu
Introduction: The available literature underscores the importance of optimizing surgical outcomes through a pre-operative checklist, which includes a review of the medical records and recent test results, changes in medical history, and a physical examination of the cardiovascular system, pulmonary system, and airway.
Case Report: We report a case of a 47-year-old man who decompensated during an outpatient wrist procedure and needed to remain intubated requiring transfer to a hospital. On follow-up with the patient, laboratory work revealed a positive HIV test and CD4 count of 11 cells/mm3, along with a pneumonia consistent with pneumocystis pneumonia, which was unbeknownst to the surgical team before the procedure.
Conclusion: This case emphasizes the importance of a thorough history and physical update and pre-operative assessment before operating.
Keywords: Pre-operative assessment, evaluation, anesthesiology, PCP, CD4, Sauvé-Kapandji procedure, physical examination, ASA.
In the following case, we find a patient who decompensated mid-surgery and was found to have active bilateral basilar pneumonia, which was unbeknownst to the surgical team before beginning the procedure. The severity of this patient’s outcome during surgery underscores the importance of a meticulous approach when evaluating pre-operative patients. Early studies evaluating the utility of standard pre-operative testing for cataract surgery revealed intra-and post-operative morbidity did not improve with routine testing. The potential utility of the pre-operative assessment to yield pre-symptomatic diagnoses was recognized but raised the issue of how to cater testing to patient needs and what do when the workup is unexpectedly normal [1]. Ultimately, the study suggests that the American College of Cardiology and the American Heart Association should not only focus on pre-operative preparation in the immediate perioperative period, but also on the long-term health care needs that have been previously neglected.
A 47-year-old man presented with a left extra-articular comminuted distal radius fracture and an associated displaced ulnar styloid fracture and gross dislocation of the distal radioulnar joint. He underwent multiple procedures to address the fracture and ulnar dislocation which was complicated by an infection necessitating hardware removal. Once the infection was eradicated with treatment of 6 weeks of IV antibiotics and fixation, the distal radius had healed. Ten months later, the patient returned with ongoing symptoms of distal radial ulnar joint pain and instability. His distal radius fracture had healed with arthritis was present in the distal radioulnar joint. The patient underwent a left distal radioulnar joint fusion with an ulnar osteotomy (Sauvé-Kapandji procedure). The patient underwent regional block and had a laryngeal mask airway placed before the procedure, which was done at an outpatient surgery center. Near the end of the procedure, the anesthesiologist had difficulty maintaining oxygen saturation above 90%. When attempts were made to prepare for extubation, the patient’s oxygenation failed to improve. Therefore, the decision was made to intubate the patient in the OR. As the patient began to decompensate, the laryngeal mask airway was removed and replaced with a general endotracheal tube. Fluid was suctioned out of the tube and the patient remained intubated. The patient was placed into a sugar-tong splint and transferred to the hospital while remaining intubated. At the hospital, a chest X-ray and a CT scan was done. Figs. 1 and 2 show a post-operative chest X-ray and axial and coronal computed tomography (CT) images which show bibasilar consolidation. Laboratory work revealed a positive HIV test and CD4 count of 11 cells/mm3. Sputum culture later confirmed PCP. While intraoperative aspiration and subsequent pneumonitis were briefly considered based on the CT findings, our X-ray findings, the patient’s CD4 count, and the sputum culture were ultimately more consistent with PCP. There was no pulmonary embolus identified, and the patient was COVID-negative. The patient was placed on broad-spectrum antibiotics and weaned off the ventilator on hospital day 2.
Once the infection was eradicated with treatment of 6 weeks of IV antibiotics and fixation, the distal radius had healed. Ten months later, the patient returned with ongoing symptoms of distal radial ulnar joint pain and instability. His distal radius fracture had healed with arthritis was present in the distal radioulnar joint. The patient underwent a left distal radioulnar joint fusion with an ulnar osteotomy (Sauvé-Kapandji procedure). The patient underwent regional block and had a laryngeal mask airway placed before the procedure, which was done at an outpatient surgery center. Near the end of the procedure, the anesthesiologist had difficulty maintaining oxygen saturation above 90%. When attempts were made to prepare for extubation, the patient’s oxygenation failed to improve. Therefore, the decision was made to intubate the patient in the OR. As the patient began to decompensate, the laryngeal mask airway was removed and replaced with a general endotracheal tube. Fluid was suctioned out of the tube and the patient remained intubated. The patient was placed into a sugar-tong splint and transferred to the hospital while remaining intubated. At the hospital, a chest X-ray and a CT scan was done. Figs. 1 and 2 show a post-operative chest X-ray and axial and coronal computed tomography (CT) images which show bibasilar consolidation. Laboratory work revealed a positive HIV test and CD4 count of 11 cells/mm3. Sputum culture later confirmed PCP. While intraoperative aspiration and subsequent pneumonitis were briefly considered based on the CT findings, our X-ray findings, the patient’s CD4 count, and the sputum culture were ultimately more consistent with PCP. There was no pulmonary embolus identified, and the patient was COVID-negative. The patient was placed on broad-spectrum antibiotics and weaned off the ventilator on hospital day 2.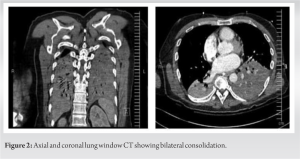 The patient initially denied new symptoms before his procedure since his last office visit, but further questioning of his wife after his post-operative admission to the hospital revealed that he had a productive cough, fever, and chills in the day leading up to the surgery. Preoperatively, the patient was hemodynamically stable, afebrile, showed no signs of infection, and denied any new symptoms to the nursing staff and anesthesiologist. Further, while the anesthesiologist evaluated the patient preoperatively, he noted he did not listen to the patient’s lungs. The patient was ultimately discharged from the hospital on day 4 in stable condition. Pre and post operative imaging can be referred to in attached figures below.
The patient initially denied new symptoms before his procedure since his last office visit, but further questioning of his wife after his post-operative admission to the hospital revealed that he had a productive cough, fever, and chills in the day leading up to the surgery. Preoperatively, the patient was hemodynamically stable, afebrile, showed no signs of infection, and denied any new symptoms to the nursing staff and anesthesiologist. Further, while the anesthesiologist evaluated the patient preoperatively, he noted he did not listen to the patient’s lungs. The patient was ultimately discharged from the hospital on day 4 in stable condition. Pre and post operative imaging can be referred to in attached figures below.
With up to 234 million surgical procedures performed worldwide, there is a wide variation in both reported incidences of adverse events, ranging from 3 to 16%, and mortality rates, estimated at 0.4–0.8% at different intervals from 1990 to 2010 [2]. With such a high volume of surgeries, these incidences, while seemingly low, constitute a deceivingly high number of adverse operative complications. As such, patients admitted for elective surgery often undergo a range of routine pre-operative tests that usually include chest radiographs, ECGs, full blood count, biochemistry, and coagulation screening to minimize the occurrence of such outcomes [3]. Common conditions which can affect perioperative care include but are not limited to ischemic heart disease, congestive cardiac failure, chronic respiratory disease, diabetes mellitus, and liver or renal dysfunction. Anesthetic drugs can also have pronounced adverse effects on cardiovascular and respiratory systems, which merit asking about symptoms of heart or respiratory failure such as chest pain, dyspnea, ankle swelling, palpitations, cough, increased sputum production, and airway obstruction. While the literature does not provide a “standard” definition for what constitutes the pre-operative evaluation, the assessment performed often considers information from multiple sources that may include the patient’s medical records, interview, physical examination, and findings from their medical tests and evaluations [4]. The American Society of Anesthesiologists’ physical status (ASA physical status) currently acts as our best tool in addressing various surgical procedures and their risks when it comes to morbidity and mortality [5]. Grading patients on a scale of I-VI (with I being a normal, healthy patient and VI being a brain-dead patient), the scale is best used to assess and communicate a patient’s functional limitations, while predicting perioperative risks [6]. Abnormal physical findings may affect a patient’s ASA score, deeming a patient unfit to undergo surgery. As such, abnormally sounding lungs could have then prompted the team to further investigate the patient’s medical history and ultimately discover their low CD4 count, suspicious imaging results, and undisclosed pre-operative symptoms, thereby cancelling the patient’s surgery. This being said, a recent meta-analysis above indicates that the ASA score is much more predictive of risk in lower risk settings when compared to higher risk settings due to its simplicity and inability to adjust surgical risk based on the setting of the procedure [2]. As such, a call for the standardization of the overall pre-operative assessment for surgery across all subspecialties is certainly of high importance.
In orthopedic surgery, individuals may often neglect routine parts of a medical physical examination preoperatively, such as listening to a patient’s heart and lungs, based on assumptions that the rest of the surgical team has medically cleared the patient for surgery. In fact, literature currently suggests that pre-operative assessments from an orthopedic standpoint often focus more on pre-operative templating to plan ahead of surgery for the best possible alignment, confirming imaging results to rule out any newfound peripheral nerve deficits, and confirming the accuracy of the patient’s past orthopedic surgical history [7, 8, 9]. Both an awareness of the surgical plan and any changes in the patient’s history found preoperatively are important in the orthopedic surgeon’s assessment of their patients’ likelihood of successfully undergoing surgery [7, 8, 9]. Nonetheless, a dearth of literature exists that has sufficiently investigated a specific way of going about the pre-operative assessment with regard to upper extremity surgery, let alone general orthopedics. This topic should be considered for future studies. Our case highlights the importance of being meticulous as a physician – that despite orthopedic surgery’s emphasis on care of the musculoskeletal system, that basic components of a physical examination, especially preoperatively, do not deserve to be neglected. A meticulous and thorough preoperative evaluation, while at times seemingly inefficient or excessively slow, will never harm the patient. Had the cRNA, the anesthesiologist, and the orthopedic surgeon all listened to our patient’s lungs, perhaps this intraoperative complication could have been prevented. The available literature has emphasized the role pre-operative assessments play in performing surgery successfully and mitigating perioperative morbidity [10, 11, 12, 13]. While potentially seen as a burden for orthopedic surgeons, especially on busy, long OR days, the pre-operative assessment is always important, and catering it to the patient helps optimize outcomes while diminishing unnecessary risks and complications.
The importance of pre-operative assessments before elective surgery is illustrated in this case report. These checkups ensure that the patient is fit to undergo surgery. Oftentimes, such assessments may be rushed preoperatively.
References
- 1.Guirguis-Blake J. Preoperative testing for patients undergoing cataract surgery. Am Fam Physician 2009;80:1228. [Google Scholar]
- 2.Koo CY, Hyder JA, Wanderer JP, Eikermann M, Ramachandran SK. A meta-analysis of the predictive accuracy of postoperative mortality using the American Society of Anesthesiologists’ physical status classification system. World J Surg 2015;39:88-103. [Google Scholar]
- 3.Zambouri A. Preoperative evaluation and preparation for anesthesia and surgery. Hippokratia 2007;11:13-21. [Google Scholar]
- 4.Committee on Standards and Practice Parameters, Apfelbaum JL, Connis RT, Nickinovich DG, American Society of Anesthesiologists Task Force on Preanesthesia Evaluation, Pasternak LR, et al. Practice advisory for preanesthesia evaluation: An updated report by the American Society of Anesthesiologists task force on preanesthesia evaluation. Anesthesiology 2012;116:522-38. [Google Scholar]
- 5.Davenport DL, Bowe EA, Henderson WG, Khuri SF, Mentzer RM Jr. National Surgical Quality Improvement Program (NSQIP) risk factors can be used to validate American Society of Anesthesiologists physical status classification (ASAPS) levels. Ann Surg 2006;243:636-41. [Google Scholar]
- 6.Committee on Economics. ASA physical status classification system. Guidelines, Statements, Clinical Resource. Illinois, USA American Society of Anesthesiologists; 2020. p. 1. [Google Scholar]
- 7.Silvera J, Masmejean E. Preoperative imaging assessment of the paralytic upper limb. Hand Surg Rehabil 2022;41S:S16-22. [Google Scholar]
- 8.Shah NS, Figueras JH, Foote AM, Steele CA, Sabbagh RS, Woods OA, et al. Recall bias in retrospective assessment of preoperative American shoulder and elbow surgeons scores after reverse total shoulder arthroplasty. J Am Acad Orthop Surg 2022;30:e1051-7. [Google Scholar]
- 9.Mensel C, Gundtoft PH, Brink O. Preoperative templating in orthopaedic fracture surgery: The past, present and future. Injury 2022;53 Suppl 3:S42-6. [Google Scholar]
- 10.Kivrak S, Haller G. Scores for preoperative risk evaluation of postoperative mortality. Best Pract Res Clin Anaesthesiol 2021;35:115-34. [Google Scholar]
- 11.De Hert S, Staender S, Fritsch G, Hinkelbein J, Afshari A, Bettelli G, et al. Pre-operative evaluation of adults undergoing elective noncardiac surgery: Updated guideline from the European Society of Anaesthesiology. Eur J Anaesthesiol 2018;35:407-65. [Google Scholar]
- 12.American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Practice advisory for preanesthesia evaluation: A report by the American Society of Anesthesiologists task force on preanesthesia evaluation. Anesthesiology 2002;96:485-96. [Google Scholar]
- 13.Wijeysundera DN. Predicting outcomes: Is there utility in risk scores? Can J Anaesth 2016;63:148-58. [Google Scholar]








