Femoral anterior rotational osteotomy is a treatment option for late-onset severe Legg-Calvé-Perthes disease.
Dr. Yoshinobu Oka, Department of Pediatric Orthopaedics, Graduate School of Medical Science, Kyoto Prefectural University of Medicine, Kawaramachi-Hirokoji, Kyoto, Japan. E-mail: y-oka@koto.kpu-m.ac.jp
Introduction: The purpose of treatment for Legg-Calvé-Perthes disease (LCPD) is to regain the sphericity of the femoral head in childhood and prevent degenerative changes in adulthood. Due to the largely unsatisfactory results of conservative treatment for late-onset LCPD (i.e. patient age >9 years.), surgery is generally indicated. Various surgeries have been applied and the reported short-term results are generally good. However, few reports have described the long-term (approximately 30 years) outcomes of femoral anterior rotational osteotomy (ARO). We herein report the long-term results of late-onset LCPD treated by femoral ARO.
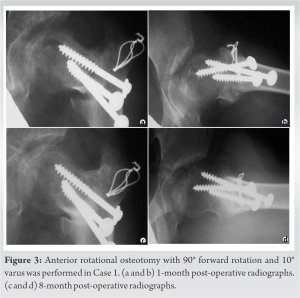
Case Report: This report describes a boy and a girl with LCPD who underwent surgical treatment at the ages of 12 and 11 years, respectively. Conservative treatment with a brace had initially been applied, but the patients subsequently developed hinge abduction; therefore, we performed femoral ARO. Five-year postoperatively, the patients’ Stulberg classification was Class II and Class III, respectively. The clinical results were satisfactory after 27 years of follow-up. Slight anterior residual deformity was seen, but there were no degenerative changes.
Conclusion: In patients with hinge abduction, it is difficult to achieve good containment by conservative treatment, and even by surgical treatment, degenerative changes can occur in the early post-operative period. In severe cases of late-onset LCPD, a femoral ARO is performed, effectively transferring the viable posterior area of the femoral head onto the weight-bearing area. Maintaining good sphericity of the femoral head helps to prevent degenerative change and leads good long-term results. Both patients described in this report were asymptomatic and did not show any signs of degenerative change upon final examination. We did, however, confirm that the anterior head-neck junction exhibited residual deformity. ARO is a proven effective option for treating late-onset severe LCPD.
Keywords: Legg-calvé-perthes disease, anterior rotational osteotomy, hinge abduction, late onset.
Legg-Calvé-Perthes disease (LCPD) is defined as the ischemic necrosis of the proximal femoral epiphysis which typically occurs in children aged 3–10 years old. The principle treatment strategy for LCPD is one of containment. Containing the femoral epiphysis in the acetabulum and non-weight-bearing will prevent or greatly reduce the chance of collapse. The age and disease severity at onset are important in the choice of treatment and affect the prognosis. Poor prognostic factors include an age of >9 years, subluxation of the femoral head, massive necrosis, and severe collapse. For severe cases of late-onset LCPD, operative procedures such as combined osteotomy and triple osteotomy are recommended [1, 2, 3, 4, 5]. Regarding the long-term outlook, degenerative changes occur before the age of 50 years in patients with aspherical incongruency [6]. Femoral anterior rotational osteotomy (ARO) is a surgical technique employed to address extensive necrosis in the femoral head, a condition known as osteonecrosis; it was first reported by Sugioka in 1978 [7, 8]. This is accomplished by rotating the femoral head forward about the axis of the femoral neck, utilizing the posterior viable region as the weight-bearing zone. We performed this technique to treat two patients with late-onset LCPD with hinge abduction. At the last examination, the patients underwent clinical and radiological assessments, with the follow-up period being 27 years. To the best of our knowledge, there are no other reports of the long-term follow-up of ARO for LCPD. The purpose of this report is to present the extended outcomes of two patients who underwent femoral ARO for the treatment of LCPD.
Case 1
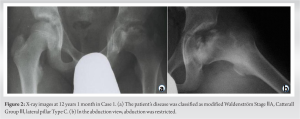
A 9-year-old boy came in for examination due to pain in his left hip. A year later, he was referred and initially diagnosed with LCPD. At the initial examination, the femoral head was found to have collapsed (Stage IIA according to the modified Waldenström classification) (Fig. 1).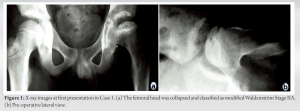
Case 2
A 10-year-old female was assessed for pain in her left hip. She had been diagnosed with LCPD at another hospital 4 months after symptom onset and was referred to us at 11 years 2 months of age. The anterolateral portion of the femoral head displayed flattening, and there was noticeable hinge abduction. Based on these observations, the stage was determined to be modified Waldenström Stage IB (Fig. 5).

The goal of treatment for LCPD is to maintain the sphericity of the femoral head and prevent future hip osteoarthritis. However, according to Herring et al. [3], children who experienced the onset of symptoms at the age of 9 or older are resistant to various treatments, their condition is difficult to manage, and late onset is associated with poorer outcomes. Because of the natural history of severe LCPD, aspherical incongruency tends to remain after maturation. In such patients, degenerative changes occur around 50 years of age. Therefore, it is essential to conduct long-term follow-up to accurately evaluate the treatment outcomes of LCPD. In the cases described here, femoral ARO was performed for late-onset LCPD. These cases are particularly valuable because the patients were followed up until middle age. Femoral varus osteotomy (FVO) is a common surgical procedure for LCPD. In general, the indication for FVO is an age of >6 years and involvement of >50% of the epiphysis [9]. FVO is a simple procedure, but it has limitations in severe cases of LCPD. Rotational open wedge osteotomy is effective and relatively simple to perform, but it is fundamentally different from ARO in that there is a limit to the forward rotation. Pelvic osteotomy has also been indicated for LCPD. Salter innominate osteotomy is an effective procedure with good long-term results [10]. However, some reports have indicated a risk of pressure on the necrotic femoral head, and achieving sufficient acetabular coverage is difficult [10, 11]. In severe cases, Salter innominate osteotomy or triple innominate osteotomy (TIO) combined with FVO (combined osteotomy) is recommended. Combined osteotomy improves both coverage and containment, but the procedure is highly invasive. Javid and Wedge [1] performed combined osteotomy at an average of 9.7 years for lateral pillar Type C or B/C. And according to the modified Stulberg classification, they reported a favorable or acceptable outcome for 67% of the patients treated. The results of TIO for severe LCPD have also recently been reported. Stepanovich et al. [2] found that TIO proves effective in younger patients with milder cases of LCPD. The advantage of TIO is its large coverage; however, it is invasive for children. Although various surgical procedures have been reported for patients with severe LCPD, there is no consensus regarding the ideal operative procedure. Herring reported that there was no association between the treatment modality and outcomes at any age in patients with lateral pillar Type C LCPD [5]. Thus, treatment tends to be chosen according to the surgeon’s experience [12]. ARO has been performed in severe cases of femoral head necrosis in adults. Dean and Cabanela evaluated 18 hips of 17 adults at a mean of 5 years after ARO for avascular necrosis [13]. Only three hips exhibited satisfactory results with respect to the application of ARO in children, Nakashima et al. [14] evaluated children aged over 9 years who had extensive necrotic lesions in the femoral head, subluxation, and/or hinge abduction. To undergo ARO for LCPD, it was necessary to have evidence of a previously healed or intact region in either the posterior or anterior femoral head. In this report, the average age for surgical intervention in cases of severe LCPD was 12 years. The results were acceptable and half of hips were class II or III according to the modified Stulberg classification [14]. Sugioka [8] reported that in seven cases (including six cases with hinge abduction) with mean age at the time of ARO of over 10 years, the results were good beyond 1-year postoperatively. Hotokebuchi et al. [15] performed ARO in patients with severe LCPD at an average age of 10 years. The results were satisfactory; no hips were classified as Stulberg Class IV or V. However, all of these reports involved only short-term follow-up. Our indications for ARO are an age >9 years, subluxation, and hinge abduction. Both of our patients in this report had severe collapse, were older than 9 years at the time of surgery, and exhibited hinge abduction. Our results support the hypothesis that ARO provides good containment. We added slight femoral varus, and a more concentric position of the femoral head was achieved. It is thought that the intact area is subjected to more mechanical stress, reducing the stress on the involved area and promoting quick repair. However, drawbacks of ARO include possible nonunion and a high greater trochanter in patients in cases in which the physis remains intact. Another problem in our cases is that a slight (1-cm) leg length difference remained. The protrusion of the head-neck junction remained in our patients and there was little modeling outside the acetabulum. The Tönnis classification grades of the hip joint were not advanced along the course and the dispersion of weight-bearing stress in the acetabulum was sufficient. In patients presenting with hinge abduction, asphericity and incongruency tend to remain. Residual deformity was present only in the anterior head-neck junction of both of our patients. There are concerns regarding future symptoms of femoroacetabular impingement, and we plan to perform bumpectomy if such symptoms appear.
Only a few reports to date have described femoral ARO for the treatment of LCPD and no reports have included a follow-up of more than 27 years. The reported cases demonstrate that ARO is an optimal treatment option for severe LCPD.
This report presents the extended outcomes of LCPD with hinge abduction treated using ARO. The findings strongly support ARO as the preferred treatment option for severe cases of LCPD.
References
- 1.Javid M, Wedge JH. Radiographic results of combined Salter innominate and femoral osteotomy in Legg-Calvé-Perthes disease in older children. J Child Orthop 2009;3:229-34. [Google Scholar]
- 2.Stepanovich M, Upasani VV, Bomar JD, Wenger DR. Advanced containment with triple innominate osteotomy in Legg-Calve-Perthes disease: A viable option even in severe cases. J Pediatr Orthop 2017;37:563-9. [Google Scholar]
- 3.Herring JA, Kim HT, Browne R. Legg-Calve-Perthes disease. Part II: Prospective multicenter study of the effect of treatment on outcome. J Bone Joint Surg Am 2004;86:2121-34. [Google Scholar]
- 4.Wiig O, Terjesen T, Svenningsen S. Prognostic factors and outcome of treatment in Perthes' disease: A prospective study of 368 patients with five-year follow-up. J Bone Joint Surg Br 2008;90:1364-71. [Google Scholar]
- 5.Herring JA. Legg-Calvé-Perthes disease at 100: A review of evidence-based treatment. J Pediatr Orthop 2011;31:S137-40. [Google Scholar]
- 6.Stulberg SD, Cooperman DR, Wallensten R. The natural history of Legg-Calvé-Perthes disease. J Bone Joint Surg Am 1981;63:1095-108. [Google Scholar]
- 7.Sugioka Y. Transtrochanteric anterior rotational osteotomy of the femoral head in the treatment of osteonecrosis affecting the hip: A new osteotomy operation. Clin Orthop Relat Res 1978;130:191-201. [Google Scholar]
- 8.Sugioka Y. Transtrochanteric rotational osteotomy in the treatment of idiopathic and steroid-induced femoral head necrosis, Perthes' disease, slipped capital femoral epiphysis, and osteoarthritis of the hip. Indications and results. Clin Orthop Relat Res 1984;184:12-23. [Google Scholar]
- 9.Leroux J, Abu Amara S, Lechevallier J. Legg-Calvé-Perthes disease. Orthop Traumatol Surg Res 2018;104:S107-12. [Google Scholar]
- 10.Park KS, Cho KJ, Yang HY, Eshnazarov KE, Yoon TR. Long-term results of modified salter innominate osteotomy for Legg-Calvé-Perthes disease. Clin Orthop Surg 2017;9:397-404. [Google Scholar]
- 11.Rab GT. Theoretical study of subluxation in early Legg-Calvé-Perthes disease. J Pediatr Orthop 2005;25:728-33. [Google Scholar]
- 12.Hefti F, Clarke NM. The management of Legg-Calvé-Perthes' disease: Is there a consensus? A study of clinical practice preferred by the members of the European paediatric orthopaedic society. J Child Orthop 2007;1:19-25. [Google Scholar]
- 13.Dean MT, Cabanela ME. Transtrochanteric anterior rotational osteotomy for avascular necrosis of the femoral head. Long-term results. J Bone Joint Surg Br 1993;75:597-601. [Google Scholar]
- 14.Nakashima Y, Kubota H, Yamamoto T, Mawatari T, Motomura G, Iwamoto Y. Transtrochanteric rotational osteotomy for late-onset Legg-Calve-Perthes disease. J Pediatr Orthop 2011;31:S223-8. [Google Scholar]
- 15.Hotokebuchi T, Kubota H, Mohtai M, Jingushi S, Fukuoka S, Iwamoto Y . et al. Transtrochanteric rotational osteotomy for Legg-Calvé-Perthes disease. J Orthop Sci 1997;2:396-404. [Google Scholar]











