Pellegrini-Stieda syndrome’s pathomechanism is similar to calcification of the rotator cuff and thus can be well managed without surgical procedure, one being an option is using percutaneous lavage.
Dr. Dio Asgira Rizky, Department of Orthopaedic and Traumatology, Faculty of Medicine, Universitas Pelita Harapan, Siloam Hospital Lippo Village, Tangerang, Indonesia. E-mail: dio.risky95@gmail.com
Introduction: Pellegrini-Stieda syndrome is described as pain and restriction at the range of motion caused by calcification in the medial collateral ligament (MCL) around the knee with the recognized radiographic findings of the lesion in the affected site. The pathomechanism of Pellegrini-Stieda is suspected to be similar as calcification of the rotator cuff that is thought to be reactive calcification followed by resorption and tendon remodeling involving four phases (pre-calcific, formative, resorptive, and healing) without any trauma history. Since the calcium deposit in the rotator cuff has been well managed by percutaneous lavage, in this case report, we assumed that the pathomechanism of Pellegrini-Stieda Syndrome is similar to calcification of the rotator cuff, thus can be treated with the same principle using ultrasound-guided percutaneous lavage (UGPL).
Objective: The aim of the study was to discuss UGPL as management for Pellegrini-Stieda with suspected similar pathomechanism to rotator cuff calcification.
Case Report: A 52-year-old woman came to the outpatient clinic with a week of severe pain in her right knee. The patient had difficulty walking due to stiffness and pain that is aggravated by moving her knee. Radiographic examination confirmed calcified lesions located within the MCL on the right knee. In consideration of the acute pain, we opted to perform UGPL procedure. Follow-ups were done 1 week and 1 month after the procedure. The patient reported no pain when walking and bending her knee during the follow-up examination and there was no complication noted. Overall, she was very satisfied with the result. We also interviewed her for the lower extremity functional scale Score which the patient gave 64 points and 72 points out of 80 for week 1 and 1 month, respectively, indicating favorable results.
Conclusion: Based on our case, UGPL can be an option for treating Pellegrini-Stieda Syndrome because it produces the same result as UGPL on rotator cuff calcification. Surgery should be the last resort if this procedure fails. Future high-quality randomized controlled trials were required to determine the reliability of this method.
Keywords: Pellegrini-stieda, pellegrini-stieda syndrome, ultrasound-guided percutaneous lavage.
Calcification of the origin of the medial collateral ligament (MCL) around the knee with the recognized radiographic findings of the lesion is termed the Pellegrini-Stieda sign. However, when the lesion causes pain and restricts the range of motion in the affected site, it is known as Pellegrini-Stieda syndrome, first described by Pellegrini and Stieda in 1905 [1, 2]. This ossification can potentially form a significant bone mass that if left untreated can cause a markedly compromised range of motion [3]. Usually, the lesion is discovered during standard radiography, then completed with magnetic resonance imaging (MRI)/CT scans for further examination [4]. Mendes et al. described four types of ossification: I: Beak-shaped with inferior orientation and union to the femur, II: Drop-shaped with inferior orientation and parallel to the femur, III: Elongated with superior orientation, and IV: With superior orientation and inferior attached to the femur [5]. The exact incidence of Pellegrini-Stieda syndrome remains unknown. Males between the age of 25 and 40 years are more often affected than females, and this syndrome is rarely found in children and older adults [6]. The lesion is usually treated conservatively with rest, anti-inflammatory medication, and physiotherapy. Surgery sometimes was done in patients with significant pain or if conservative treatments fail, usually done with open or arthroscopic excision of the calcification [7]. However, surgery for Rotator Cuff Calcification is gradually being superseded by new minimally invasive options such as ultrasound-guided percutaneous lavage (UGPL). Several researches have reported several advantages of UGPL, such as cost-effectiveness, simplicity of the technique, require no hospitalization, and also significantly reduces pain in the majority of patients resulting in enhanced popularity [8, 9, 10]. The pathomechanism of Pellegrini-Stieda Syndrome is suspected to be similar to rotator cuff calcification, it comes from a variety of causes, degenerative, and reactive causes. Degenerative in the form of dystrophic calcification of the tendon which occurs in the presence of normal calcium metabolism and takes place in presumably damaged or devitalized tissues caused by history of trauma. Usually, it occurs due to damage to the tendon which leads to acute inflammation and triggers the ossification process [11]. Reactive cause in a form of active calcification followed by reabsorption and tendon remodeling involving four phases (pre-calcific, formative, resorptive, and healing) without any trauma history [12]. Since the calcium deposit in the rotator cuff has been well managed by percutaneous lavage, we report a patient who presented with severe medial knee pain and was treated with UGPL, a technique that has returned good results in the management of calcific tendinitis, such as calcific tendinitis of the rotator cuff. The diagnosis was made after X-ray, ultrasound, and MR examinations, which revealed calcified lesions in MCL. We opted to do UGPL rather than arthroscopic surgery due to the acute pain with no prior history of trauma or overuse of the joint, with the suspicion that the pathomechanism resembles that of rotator cuff calcification. The technique is simple, cost-effective, does not require hospitalization, and also significantly reduces pain in the majority of patients.
A 52-year-old woman came to the outpatient clinic with a week of severe pain in her right knee. The pain appeared after excessive walking and is aggravated when the patient stands up from sitting. The patient also had difficulty walking due to pain and stiffness when moving her knee in the morning but reported no clicking sensation. The NRS score was nine out of 10. Systemic diseases such as gout, or any metabolic or endocrine disorders such as diabetes mellitus were denied. There was no past injury recorded. Physical examination showed effusion, limited range of motion, and tenderness in the medial joint line of the right knee. The patient was unable to flex her knee due to pain. A knee ultrasound revealed calcification on the medial retinacular, suggesting a calcifying lesion within the MCL. X-ray and MRI without a contrast agent of the knee confirmed the presence of calcified lesions located around the medial condyle of the femur and MCL hence confirming the diagnosis of Pellegrini-Stieda Syndrome (Fig. 1). 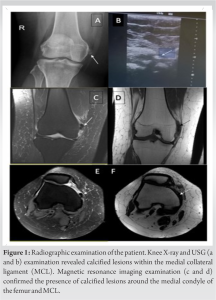

Pellegrini-Stieda syndrome is a rare phenomenon that is the calcification of the origin of the MCL which causes discomfort to the patient [3]. The exact pathomechanism of Pellegrini-Stieda Syndrome remains unclear. There are several mechanisms suspected of causing Pellegrini-Stieda Syndrome, including degenerative and reactive cause, which are suspected as the same as rotator cuff calcification [11]. In this case report, we present the simple method to treat Pellegrini-Stieda Syndrome based on the assumption that the etiology is the same as rotator cuff calcification. Like most previous studies, our patient does not have any history of trauma or overuse of the joint. History of metabolic or systemic diseases was also denied. As far as we know, there is insufficient research to determine the gold standard treatment for Pellegrini-Stieda Syndrome. From the research we collected, we found that the treatment of Pellegrini-Stieda Syndrome was done in four open resections surgery, one arthroscopic removal, and one open resection followed by MCL reconstruction. One case report from Siddiq et al. uses intralesional steroid injection for treating Pellegrini-Stieda syndrome. Although the patient was satisfied with the treatment result, the use of steroid injection may damage the MCL, since it increases the risk of tendon/ligament rupture [13]. In recent case reports, UGPL became a popular treatment for Pellegrini-Stieda syndrome. Three case reports showed good results and patient satisfaction after undergoing the UGPL procedure to break down the calcific formation. We opted to do UGPL because we assumed the Pellegrini-Stieda syndrome in this case has similar patho-mechanics as the rotator cuff calcification. It is also a less-invasive and relatively easy procedure to do with a higher success probability based on the early calcific rotator cuff tendinitis studies compared to other treatments [14, 15, 16]. Moreover, the results of the UGPL that we did reveal the same results as the UGPL treatment of calcification of the rotator cuff. The recent Pellegrini-Stieda case treated with UGPL reports also showed good results.
Based on our case, UGPL can be an option for treating Pellegrini-Stieda syndrome, especially during the inflammatory phase. Surgery should be the last resort if this procedure fails. Future high-quality randomized controlled trials were required to determine the reliability of this method.
Pellegrini-Stieda syndrome’s pathomechanism is similar to calcification of the rotator and thus can be well managed without surgical procedure, one being an option is using percutaneous lavage.
References
- 1.Somford MP, Lorusso L, Porro A, Loon CV, Eygendaal D. The Pellegrini-Stieda lesion dissected historically. J Knee Surg 2018;31:562-7. [Google Scholar]
- 2.Wiegerinck J, Somford M. Review of Stieda’s article (1908) on the Pellegrini-Stieda lesion. J ISAKOS 2016;1:214-8. [Google Scholar]
- 3.Theivendran K, Lever CJ, Hart WJ. Good result after surgical treatment of Pellegrini-Stieda syndrome. Knee Surg Sports Traumatol Arthrosc 2009;17:1231-3. [Google Scholar]
- 4.Elhend S, Doulhousne H, Rokhssi R, Hamoune N. Pellegrini-Stieda syndrome. PAMJ Clin Med 2020;2:21099 [Google Scholar]
- 5.Mendes LF, Pretterklieber ML, Cho JH, Garcia GM, Resnick DL, Chung CB. Pellegrini-Stieda disease: A heterogeneous disorder not synonymous with ossification/calcification of the tibial collateral ligament-anatomic and imaging investigation. Skeletal Radiol 2006;35:916-22. [Google Scholar]
- 6.Restrepo J, Molina M. Pellegrini-Stieda syndrome: More than a radiological sign. Rev Colomb Reumatol (Engl Ed) 2016;23:210-2. [Google Scholar]
- 7.Jacobs R, Debeer P. Calcifying tendinitis of the rotator cuff: Functional outcome after arthroscopic treatment. Acta Orthop Belg 2006;72:276-81. [Google Scholar]
- 8.Zhang T, Duan Y, Chen J, Chen X. Efficacy of ultrasound-guided percutaneous lavage for rotator cuff calcific tendinopathy: A systematic review and meta-analysis. Medicine (Baltimore) 2019;98:e15552. [Google Scholar]
- 9.De Boer FA, Mocking F, Nelissen EM, van Kampen PM, Huijsmans PE. Ultrasound guided needling versus radial shockwave therapy in calcific tendinitis of the shoulder: A prospective randomized trial. J Orthop 2017;14:466-9. [Google Scholar]
- 10.Kim YS, Lee HJ, Kim YV, Kong CG. Which method is more effective in treatment of calcific tendinitis in the shoulder? Prospective randomized comparison between ultrasound-guided needling and extracorporeal shock wave therapy. J Shoulder Elbow Surg 2014;23:1640-6. [Google Scholar]
- 11.Refior HJ, Krödel A, Melzer C. Examinations of the pathology of the rotator cuff. Arch Orthop Trauma Surg (1978) 1987;106:301-8. [Google Scholar]
- 12.Uhthoff HK, Loehr JW. Calcific tendinopathy of the rotator cuff: Pathogenesis, diagnosis, and management. J Am Acad Orthop Surg 1997;5:183-91. [Google Scholar]
- 13.Brinks A, Koes BW, Volkers AC, Verhaar JA, Bierma-Zeinstra SM. Adverse effects of extra-articular corticosteroid injections: A systematic review. BMC Musculoskelet Disord 2010;11:206. [Google Scholar]
- 14.de Witte PB, Selten JW, Navas A, Nagels J, Visser CP, Nelissen RG, et al. Calcific tendinitis of the rotator cuff: A randomized controlled trial of ultrasound-guided needling and lavage versus subacromial corticosteroids. Am J Sports Med 2013;41:1665-73. [Google Scholar]
- 15.del Cura JL, Torre I, Zabala R, Legórburu A. Sonographically guided percutaneous needle lavage in calcific tendinitis of the shoulder: Short- and long-term results. AJR Am J Roentgenol 2007;189:W128-34. [Google Scholar]
- 16.de Zordo T, Ahmad N, Ødegaard F, Girtler MT, Jaschke W, Klauser AS, et al. US-guided therapy of calcific tendinopathy: Clinical and radiological outcome assessment in shoulder and non-shoulder tendons. Ultraschall Med 2011;32 Suppl 1:S117-23. [Google Scholar]
- 17.Muschol M, Müller I, Petersen W, Hassenpflug J. Symptomatic calcification of the medial collateral ligament of the knee joint: A report about five cases. Knee Surg Sports Traumatol Arthrosc 2005;13:598-602. [Google Scholar]
- 18.Chang WC, Huang GS, Lee CH, Kao HW, Chen CY. Calcification of medial collateral ligament of the knee: An uncommon cause of medial knee pain. J Clin Rheumatol 2006;12:204-5. [Google Scholar]
- 19.Vampertzis T, Agathangelidis F, Gkouliopoulou E, Papastergiou S. Massive non-traumatic calcification of the medial collateral ligament of the knee. BMJ Case Rep 2016;2016:bcr2016217743. [Google Scholar]
- 20.Kamawal Y, Steinert AF, Holzapfel BM, Rudert M, Barthel T. Case report – Calcification of the medial collateral ligament of the knee with simultaneous calcifying tendinitis of the rotator cuff. BMC Musculoskelet Disord 2016;17:283. [Google Scholar]
- 21.Song K, Dong J, Zhang Y, Chen B, Wang F, Zhao J, et al. Arthroscopic management of calcific tendonitis of the medial collateral ligament. Knee 2013;20:63-5. [Google Scholar]
- 22.Siddiq MA, Jahan I. Medial collateral ligament calcification: A rare knee pain entity with literature review. Acta Radiol Open 2017;6:2058460117738549. [Google Scholar]
- 23.Del Castillo-González F, Ramos-Álvarez JJ, González-Pérez J, Jiménez-Herranz E, Rodríguez-Fabián G. Ultrasound-guided percutaneous lavage of calcific bursitis of the medial collateral ligament of the knee: A case report and review of the literature. Skeletal Radiol 2016;45:1419-23. [Google Scholar]
- 24.Galletti L, Ricci V, Andreoli E, Galletti S. Treatment of a calcific bursitis of the medial collateral ligament: A rare cause of painful knee. J Ultrasound 2019;22:471-6. [Google Scholar]
- 25.Greidanus BD. A novel treatment of painful medial collateral ligament calcification (Pellegrini-Stieda syndrome): A case report. Clin J Sport Med 2022;32:e441-2. [Google Scholar]











