Knee arthrodesis along with Ilizarov ring fixator and limb lengthening surgery is a distinctive way to treat infected non-union of distal femur with severe arthritic changes.
Dr. Shivam Mehra, Department of Orthopaedics, Padmashree Dr. D.Y. Patil School of Medicine, Navi Mumbai - 400 706, Maharashtra, India. E-mail: drshivammehra@gmail.com
Introduction: Femoral fractures in adults are around 3 –6% and 0.4% of all the fractures are usually distal femoral fractures, frequently consisting of high-energy injuries which are associated with compound trauma. Conventionally, femoral–tibial fusion remains one of the last treatment choices for the recurrent septic failure.
Case Report: We report a unique case where a 52-year-old male had presented with a post-operative infected non-union of distal femur and patella with discharging sinus and distal femur plate in situ. The patient presented to our outpatient department with complaints of pain and swelling over right knee with discharging sinus with fixed flexion deformity of 20° for 1-year post trauma and post-surgery. The discharging sinus was over lateral aspect of knee with purulent discharge. His blood parameters were suggestive of high erythrocyte sedimentation rate, and C-reactive protein levels and a Gram staining were suggestive of Gram-negative bacilli. X-ray showed non-union of distal femur and osteomyelitic changes and knee subluxation with distal femur plate and encirclage with K-wire for patella in situ. The patient underwents three-stage procedure of debridement with implant removal, followed by knee arthrodesis and ultimately limb lengthening surgery.
Conclusion: Our case report is unique and distinctive as it shows that, when a case of infected non-union of distal femur comes with stiff and non-salvageable knee with severe arthritic changes and financial constraints, we should consider for knee arthrodesis with ilizarov ring fixator and limb lengthening surgery. Although it yielded stiff knee but with functioning limb without limb length discrepancy.
Keywords: Osteomyelitis, distal femur, knee arthrodesis, limb lengthening, ilizarov ring fixator.
Osteomyelitis is a major bone infection that can be acute or chronic. The condition involves an inflammatory process that affects the bone occurring due to pyogenic organisms that spread through surgery, fractures, or bloodstream [1, 2, 3]. Open contaminated fractures can lead to the development of osteomyelitis of the fractured bone in 3–25% of cases, depending on fracture type, degree of soft-tissue injury, degree of microbial contamination, and whether systemic and/or local antimicrobial therapies have been administered [4, 5, 6, 7]. Bacteria are inoculated directly on the bone surface at the time of trauma, at the time of surgery, and/or in the early postoperative period; early microbial contamination can eventually lead to the development of osteomyelitis at the fracture site. Untreated, infection will ultimately lead to non-union, chronic osteomyelitis [4]. Here, we present a unique case of a 52-year-old male who had an infected non-union of distal femur with knee subluxation treated with knee arthrodesis along with ilizarov ring fixator and limb lengthening surgery.
We report a unique case where a 52-year-old male had presented with a post-operative infected non-union of distal femur with knee subluxation with discharging sinus and distal femur plate in situ. The patient presented to our outpatient department with the complaints of pain and swelling over the right knee with discharging sinus with fixed flexion deformity of 20° for 1-year post-trauma and post-surgery. The discharging sinus was with purulent discharge over lateral aspect of knee. The patient was admitted, and a routine blood investigation was done and a base value of erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) was recorded. Furthermore, a culture swab was sent for the patient from the discharging sinus. Primary X-ray was done. X-ray showed sequestered bone in the distal femur and osteomyelitic changes with distal femur plate and encirclage with K-wire for patella in situ (Fig. 1). His blood parameters were suggestive of high ESR, and CRP levels and a Gram staining were suggestive of Gram-negative bacilli. Broadly, the patient underwent a three-stage procedure, first debridement and implant removal, after 1 month, the second definitive procedure in the form of knee arthrodesis with ring fixator was done followed, which 2 months later, limb lengthening surgery was performed. Post–operatively, the patient was kept on analgesics and an antibiotic (found to be sensitive in culture sensitivity). The patient underwent a post-operative dressing on Day 2 and Day 5, and ESR and CRP values were recorded after 1-week post-surgery to check for prognosis. Once the infection subsided in a course of time, a second definitive procedure in the form of knee arthrodesis with ring fixator was done. At first stage, the patient was taken under spinal anesthesia followed by previous implant removal (Fig. 2) and then debridement. Fracture margins were freshened, and tissue was sent for culture and sensitivity testing. The intra-operative findings showed non-union, diffuse infection, adherent patella, and complete articular cartilage erosion. Thus, in the second stage, arthrodesis was planned in view of infection, non-union, severe arthritic, subluxated knee, stiff knee, non-salvage knee joint (Fig. 3 shows X-ray post knee arthrodesis).
His blood parameters were suggestive of high ESR, and CRP levels and a Gram staining were suggestive of Gram-negative bacilli. Broadly, the patient underwent a three-stage procedure, first debridement and implant removal, after 1 month, the second definitive procedure in the form of knee arthrodesis with ring fixator was done followed, which 2 months later, limb lengthening surgery was performed. Post–operatively, the patient was kept on analgesics and an antibiotic (found to be sensitive in culture sensitivity). The patient underwent a post-operative dressing on Day 2 and Day 5, and ESR and CRP values were recorded after 1-week post-surgery to check for prognosis. Once the infection subsided in a course of time, a second definitive procedure in the form of knee arthrodesis with ring fixator was done. At first stage, the patient was taken under spinal anesthesia followed by previous implant removal (Fig. 2) and then debridement. Fracture margins were freshened, and tissue was sent for culture and sensitivity testing. The intra-operative findings showed non-union, diffuse infection, adherent patella, and complete articular cartilage erosion. Thus, in the second stage, arthrodesis was planned in view of infection, non-union, severe arthritic, subluxated knee, stiff knee, non-salvage knee joint (Fig. 3 shows X-ray post knee arthrodesis).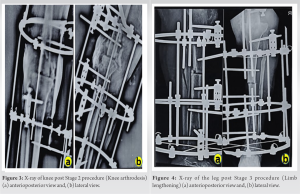 Excision of distal femur was done, and tibia articular surface was shaved and acute docking was done and ilizarov ring fixator was applied maintaining the alignment in frontal and sagittal plane. 2 rings on tibia and 1 full ring with Italian arch on femur were applied. Gradual compression over the fixator was done till a good contact was seen on the X-ray in arthrodesis site, excision of distal femoral condyle, and compression at arthrodesis site had led to a 3-inch shorting. The wound healed in 6 weeks completely without the sinus and there was good radiographic osteogenesis at knee arthrodesis site, as we had arthrodesed the knee, so limb lengthening surgery by tibial osteotomy was planned to overcome the limb length discrepancy as tibial osteotomy was simpler, the ilizarov frame was less cumbersome (Fig. 4).
Excision of distal femur was done, and tibia articular surface was shaved and acute docking was done and ilizarov ring fixator was applied maintaining the alignment in frontal and sagittal plane. 2 rings on tibia and 1 full ring with Italian arch on femur were applied. Gradual compression over the fixator was done till a good contact was seen on the X-ray in arthrodesis site, excision of distal femoral condyle, and compression at arthrodesis site had led to a 3-inch shorting. The wound healed in 6 weeks completely without the sinus and there was good radiographic osteogenesis at knee arthrodesis site, as we had arthrodesed the knee, so limb lengthening surgery by tibial osteotomy was planned to overcome the limb length discrepancy as tibial osteotomy was simpler, the ilizarov frame was less cumbersome (Fig. 4). 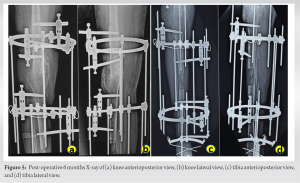 Distraction was started and followed up for 5 months. Results were seen with sound knee arthrodesis and good osteogenesis at the osteotomy site followed by achieving the limb length just 1-inch short from the normal side to achieve ground clearance while walking. Patients last followed up until frame removal and was fully satisfied; he was able to do all these basic daily activities expect while travelling in local transportation was a little difficult and was not able to sit on Indian style toilet (Figs. 5-9).
Distraction was started and followed up for 5 months. Results were seen with sound knee arthrodesis and good osteogenesis at the osteotomy site followed by achieving the limb length just 1-inch short from the normal side to achieve ground clearance while walking. Patients last followed up until frame removal and was fully satisfied; he was able to do all these basic daily activities expect while travelling in local transportation was a little difficult and was not able to sit on Indian style toilet (Figs. 5-9).
The management and treatment of distal femur fractures have improved in the recent past with treatment options that include open reduction and internal fixation with periarticular locking plates, intramedullary nails, or distal femur replacement. Despite these innovations, there have been a number of challenges in the management of distal femur fractures that include high rates of non-union, malunion, and implant failure [8]. For instance, in a study by Henderson et al. where locked plate was used as an implant, non-union was observed in 19% of the patients, and implant failure was as high as 20% [9]. In addition to malunion or failure, implant-associated infections are very common [10, 11]. These bacterial infections can cause chronic osteomyelitis, non-union of fracture, and amputation [10, 11, 12, 13]. Another factor that adds to these challenges is an osteoporotic small distal femoral fragment, with multiple holes in the femoral condyle due to previous implant, with lead to knee stiffness and patellar adhesion. In this case of a 52-year-old male, financial constraints along with non-union and osteomyelitis were the driving factors to implement a unique procedure involving debridement with ilizarov ring fixator followed by limb lengthening surgery. Debridement of the infected bone leads to union of the bone and arthrodesis. Ilizarov ring fixator is an external fixator that provides support and this followed by limb lengthening surgery avoids limb length discrepancy and achieves limb length just one-inch shot of the normal limb.
Arthrodesis was planned in view of infection, non-union, severe arthritic, subluxated knee, stiff knee, non-salvage knee joint, and financial constraints. Results were seen with sound knee arthrodesis and good consolidation of regenerate, followed by achieving the limb length just 1-inch short from the normal side to achieve ground clearance while walking. To conclude, our case report is unique and distinctive as it shows that when a case of infected non-union of distal femur comes with stiff and non-salvage knee with severe arthritic changes, with knee subluxation and financial constraints, we should consider for knee arthrodesis with Ilizarov ring fixator followed by limb lengthening surgery.
Distal femur infected non-union usually ends up stiff knee after healing. Hence, when presented with a case of infected non-union, the illizarov ring fixator can achieve arthrodesis and lengthening of distal femur, which is difficult to treat with other techniques. Therefore, it should be considered a treatment modality.
References
- 1.Lew DP, Waldvogel FA. Osteomyelitis. Lancet 2004;364:369-79. [Google Scholar]
- 2.Lew DP, Waldvogel FA. Osteomyelitis. N Engl J Med 1997;336:999-1007. [Google Scholar]
- 3.Hatzenbuehler J, Pulling TJ. Diagnosis and management of osteomyelitis. Am Fam Physician 2011;84:1027-33. [Google Scholar]
- 4.Sia IG, Berbari EF. Osteomyelitis. Best Pract Res Clin Rheumatol 2006;20:1065-81. [Google Scholar]
- 5.Merritt K. Factors increasing the risk of infection in patients with open fractures. J Trauma Acute Care Surg 1988;28:823-7. [Google Scholar]
- 6.DeLong WG, Born CT, Wei SY, Petrik ME, Ponzio R, Schwab CW. Aggressive treatment of 119 open fracture wounds. J Trauma Acute Care Surg 1999;46:1049-54. [Google Scholar]
- 7.Ostermann PA, Seligson D, Henry SL. Local antibiotic therapy for severe open fractures. A review of 1085 consecutive cases. J Bone Joint Surg 1995;77:93-7. [Google Scholar]
- 8.Hake ME, Davis ME, Perdue AM, Goulet JA. Modern implant options for the treatment of distal femur fractures. J Am Acad Orthop Surg 2019;27:e867-75. [Google Scholar]
- 9.Henderson CE, Lujan T, Bottlang M, Fitzpatrick DC, Madey SM, Marsh JL. Stabilization of distal femur fractures with intramedullary nails and locking plates: Differences in callus formation. Iowa Orthop J 2010;30:61. [Google Scholar]
- 10.Trampuz A, Zimmerli W. Diagnosis and treatment of implant-associated septic arthritis and osteomyelitis. Curr Infect Dis Rep 2008;10:394-403. [Google Scholar]
- 11.Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infections. N Engl J Med 2004;351:1645-54. [Google Scholar]
- 12.Steckelberg JM, Osmon DR. Prosthetic joint infections. In: Infections Associated with Indwelling Medical Devices. Belgium: American Society for Microbiology; 2000. p. 173-209. [Google Scholar]
- 13.Trampuz A, Zimmerli W. Diagnosis and treatment of infections associated with fracture-fixation devices. Injury 2006;37: S59-66. [Google Scholar]











