Implantable gait monitoring devices may aid clinicians in detecting poor outcomes following total knee arthroplasty.
Dr. Derek Yocum, South Bend Orthopaedics, 60160 Bodnar Blvd, Mishawaka, IN, 46544 United States. E-mail: dyocum@sbortho.com
Introduction: Although surgical devices and techniques continue to improve, regular post-operative monitoring of patients is required to ensure the best outcomes. New technological advances have allowed physicians to monitor the daily recovery of total knee arthroplasty (TKA) patients. This report is the first to describe the utilization of an implantable gait monitoring device and its capacity to detect poor early post-operative outcomes.
Case Report: Two patients, a 78-year-old male and a 34-year-old female, were assessed post-TKA utilizing remote gait kinematics and clinical evaluations and determined to need manipulation under anesthesia due to severely limited range of motion. One patient, a 51-year-old female, with good clinical outcomes, was used for comparison.
Conclusion: Remote monitoring may provide an earlier indication than clinical evaluations in identification of TKA patients at risk of poor outcomes and may who need intervention. The use of remote kinematic gait data in earlier identification of patients at risk has the potential to help improve outcomes for the broader population of TKA patients.
Keywords: Manipulation under anesthesia, total knee arthroplasty, range of motion.
The primary goals of total knee arthroplasty (TKA) are to improve range of motion (ROM) and reduce pain. Despite advances in surgical devices and techniques, some patients develop arthrofibrosis, a condition characterized by excessive build-up of scar tissue, leading to a painful knee with limited ROM [1]. One method for improving patient outcomes when patients demonstrate poor post-operative ROM is manipulation under anesthesia (MUA). Typical eligibility for MUA is patients who cannot achieve over 90° of flexion by 6–12 weeks post-TKA [2]. Research suggests that earlier interventions may lead to better outcomes [3]. Risk factors for developing arthrofibrosis and requiring MUA include previous ACL reconstruction, young age, female sex, smoking, systemic disease, history of previous knee surgeries, limited preoperative ROM, complexity of the TKA surgery, and poor post-operative rehabilitation [4, 5, 6]. In 513 consecutive primary knees replaced at our institution between November 1, 2021, and July 1, 2022, 11 patients required an MUA. Of these 513 patients, 182 were implanted with Zimmer Biomet’s Persona IQ® The Smart Knee®, two of which required an MUA. Persona IQ includes an embedded 3D accelerometer, 3D gyroscope, and pedometer within the tibial stem extension, allowing for remote collection of daily-living gait kinematics. The purpose of this case study was to identify the potential utility of kinematic data collected by Persona IQ in identifying risk for MUA in the early post-operative period. Specifically, this study will focus on the ROM of the knee during gait, collected by Persona IQ before and following MUA. In this case series, we will refer to this as functional ROM, whereas maximum passive flexion/extension ROM will be referred to as peak ROM.
Patient 1 is a 78-year-old male who underwent a primary left TKA on February 10, 2022, with no complications. Pre-operative X-rays confirmed the presence of osteoarthritis and joint space narrowing (Fig. 1, Top Left).  Postoperatively, the patient participated in outpatient physical therapy 2–3 times per week for 9 weeks, beginning 4-day postoperatively. During physical therapy, a decline in peak ROM was noted at 4 weeks. X-rays taken at this time confirmed proper joint alignment and well-affixed implants (Fig. 1, Top Right). The patient’s medical history includes high cholesterol and sleep apnea, as well as hearing loss and frequent urination. The patient was a former smoker, who ceased over 16 years ago and self-reports a moderate level of alcohol consumption. Preoperatively, the patient had a limited peak ROM of 5–95°. During the first 2 weeks following surgery, the patient averaged a functional ROM of 42°. The recovery curve for this parameter shows that the patient was below the 25th percentile, among men ≥65 years. Peak ROM was 4–83° at 2-weeks post-TKA. Functional ROM averaged 43.5° over weeks 3 and 4, followed by a decrease at week 5, illustrated on the recovery curve as the patient’s functional ROM falling below the 5th percentile. 7-week post-TKA, the peak ROM had increased to 3-115° but the functional ROM was only at the 10th percentile. Although the patient had made progress in their peak knee flexion, they were still unable to reach full extension of the knee, and the patient reported increased pain and swelling. For these reasons, an MUA was performed 9 weeks following surgery. Following the MUA, physical therapy was prescribed 5 times per week for 2 weeks, followed by an additional 2–3 times per week for 6 weeks. Three weeks following MUA, functional ROM increased to an average of 48.5°, while peak ROM was 11–99°. By 7-week post-MUA, approximately 16 weeks after initial TKA, the patient had a functional ROM of 50.3°, and peak ROM was measured at 6–111°. Over the next 4 weeks, the patient averaged 52° of functional ROM (Fig. 2, Top). Patient two is a 34-year-old female who underwent a primary left TKA on June 1, 2022 with no complications. Pre-operative X-rays confirmed severe osteoarthritis and joint space narrowing (Fig. 1, Middle Left). The patient participated in outpatient physical therapy 1–3 times per week for 6 weeks starting 2 days after surgery. Post-operative X-rays confirmed proper joint alignment and well-affixed implants (Fig. 1, Middle Right). The patient’s past medical history consists of a previous ACL and meniscal repair, hypothyroidism, arthritis, and Type 2 diabetes. This patient does not have a history of smoking and self-reports occasional alcohol consumption.
Postoperatively, the patient participated in outpatient physical therapy 2–3 times per week for 9 weeks, beginning 4-day postoperatively. During physical therapy, a decline in peak ROM was noted at 4 weeks. X-rays taken at this time confirmed proper joint alignment and well-affixed implants (Fig. 1, Top Right). The patient’s medical history includes high cholesterol and sleep apnea, as well as hearing loss and frequent urination. The patient was a former smoker, who ceased over 16 years ago and self-reports a moderate level of alcohol consumption. Preoperatively, the patient had a limited peak ROM of 5–95°. During the first 2 weeks following surgery, the patient averaged a functional ROM of 42°. The recovery curve for this parameter shows that the patient was below the 25th percentile, among men ≥65 years. Peak ROM was 4–83° at 2-weeks post-TKA. Functional ROM averaged 43.5° over weeks 3 and 4, followed by a decrease at week 5, illustrated on the recovery curve as the patient’s functional ROM falling below the 5th percentile. 7-week post-TKA, the peak ROM had increased to 3-115° but the functional ROM was only at the 10th percentile. Although the patient had made progress in their peak knee flexion, they were still unable to reach full extension of the knee, and the patient reported increased pain and swelling. For these reasons, an MUA was performed 9 weeks following surgery. Following the MUA, physical therapy was prescribed 5 times per week for 2 weeks, followed by an additional 2–3 times per week for 6 weeks. Three weeks following MUA, functional ROM increased to an average of 48.5°, while peak ROM was 11–99°. By 7-week post-MUA, approximately 16 weeks after initial TKA, the patient had a functional ROM of 50.3°, and peak ROM was measured at 6–111°. Over the next 4 weeks, the patient averaged 52° of functional ROM (Fig. 2, Top). Patient two is a 34-year-old female who underwent a primary left TKA on June 1, 2022 with no complications. Pre-operative X-rays confirmed severe osteoarthritis and joint space narrowing (Fig. 1, Middle Left). The patient participated in outpatient physical therapy 1–3 times per week for 6 weeks starting 2 days after surgery. Post-operative X-rays confirmed proper joint alignment and well-affixed implants (Fig. 1, Middle Right). The patient’s past medical history consists of a previous ACL and meniscal repair, hypothyroidism, arthritis, and Type 2 diabetes. This patient does not have a history of smoking and self-reports occasional alcohol consumption. 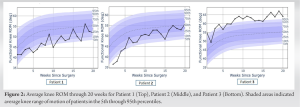 Preoperatively, the patient had a limited peak ROM of 19–71°. During the initial 2 weeks following surgery, the patient averaged only 37° of functional ROM, below the 5th percentile among females ≤65 years (Fig 2, middle). At her 2-week follow-up, the patient’s peak ROM was 17–70°. The functional ROM average between weeks 3 and 6 was 43.75°. At 6 weeks post-TKA the patient’s peak ROM had only improved to 3–86°. The patient underwent MUA at 7-week post-TKA due to arthrofibrosis limiting knee mobility. Following MUA, physical therapy was prescribed 1–3 times per week for 6 weeks. Over the 2 weeks following MUA, the patient averaged 49° of functional ROM and had an improved peak ROM of 6–91°. At 5-week post-MUA, the patient had a peak ROM of 0–107°, and was averaging 51° of functional ROM. The patient continued to be remotely monitored and showed continuous improvements in functional ROM with an average of 54° between 16- and 20-week post-TKA (Fig. 2, Middle). Patient three is a 51-year-old female who underwent primary left TKA on June 1, 2022 with no complications. Pre-operative X-rays confirmed severe osteoarthritis and joint space narrowing (Fig. 1, Bottom Left). The patient began outpatient physical therapy 2 days after surgery and continued 2–3 times per week for 6 weeks. Post-operative X-rays confirmed proper joint alignment and well-affixed implants (Fig. 1, Bottom Right). This patient’s medical history consists of previous left knee ACL reconstruction, knee arthroscopy with partial medial and lateral meniscectomies. This patient does not have a history of smoking and self-reports occasional alcohol consumption. Preoperatively, the patient had a limited peak knee ROM of 13–102°. During the 2 weeks between surgery and the initial clinical visit, the patient averaged 51.5° of functional ROM. At her 2-week follow-up, the patient had a peak ROM of 0–105°. Over the following 4 weeks, the patient averaged 57.8° of functional ROM and had a peak ROM of 0–124°. From week 8 through 20 post-TKA, this patient maintained a relatively stable functional ROM, averaging 63.6° throughout this time period (Fig. 2, Bottom).
Preoperatively, the patient had a limited peak ROM of 19–71°. During the initial 2 weeks following surgery, the patient averaged only 37° of functional ROM, below the 5th percentile among females ≤65 years (Fig 2, middle). At her 2-week follow-up, the patient’s peak ROM was 17–70°. The functional ROM average between weeks 3 and 6 was 43.75°. At 6 weeks post-TKA the patient’s peak ROM had only improved to 3–86°. The patient underwent MUA at 7-week post-TKA due to arthrofibrosis limiting knee mobility. Following MUA, physical therapy was prescribed 1–3 times per week for 6 weeks. Over the 2 weeks following MUA, the patient averaged 49° of functional ROM and had an improved peak ROM of 6–91°. At 5-week post-MUA, the patient had a peak ROM of 0–107°, and was averaging 51° of functional ROM. The patient continued to be remotely monitored and showed continuous improvements in functional ROM with an average of 54° between 16- and 20-week post-TKA (Fig. 2, Middle). Patient three is a 51-year-old female who underwent primary left TKA on June 1, 2022 with no complications. Pre-operative X-rays confirmed severe osteoarthritis and joint space narrowing (Fig. 1, Bottom Left). The patient began outpatient physical therapy 2 days after surgery and continued 2–3 times per week for 6 weeks. Post-operative X-rays confirmed proper joint alignment and well-affixed implants (Fig. 1, Bottom Right). This patient’s medical history consists of previous left knee ACL reconstruction, knee arthroscopy with partial medial and lateral meniscectomies. This patient does not have a history of smoking and self-reports occasional alcohol consumption. Preoperatively, the patient had a limited peak knee ROM of 13–102°. During the 2 weeks between surgery and the initial clinical visit, the patient averaged 51.5° of functional ROM. At her 2-week follow-up, the patient had a peak ROM of 0–105°. Over the following 4 weeks, the patient averaged 57.8° of functional ROM and had a peak ROM of 0–124°. From week 8 through 20 post-TKA, this patient maintained a relatively stable functional ROM, averaging 63.6° throughout this time period (Fig. 2, Bottom).
The purpose of this study was identifying the potential utility of kinematic data collected by Persona IQ in identifying risk for MUA in the early post-operative period. To this affect, we provided two case reports in which daily-living kinematic data, specifically functional ROM during gait, can assist in determining MUA candidacy of patients due to suboptimal performance early in the post-operative period. Evaluating patient satisfaction and recovery has typically relied on patient-reported outcomes (PROMS) and physical examination at discrete time points following surgery [7, 8, 9, 10, 11, 12, 13]. These early post-operative visits are critical in determining the potential need for MUA and rely on patients’ compliance with their follow-up visits. Lack of compliance with follow-up visits can have serious consequences on functional recover, as the optimal window for an MUA is <3 months following surgery [3]. The patients presented in this case series followed the usual standard-of-care follow-up regimen, where they were seen for their initial post-operative appointment 2 weeks after surgery, where it was first noted that an MUA may be required to regain an adequate range of knee ROM. During the first 3 weeks of patients’ recovery, their functional ROMs were below the 25th and the 5th percentiles for patients one and two, respectively. The knee kinematics of the patients’ daily-living gait were the first indication that the patients were potential candidates for an MUA. As shown in Fig. 2, a low functional ROM is clearly visible during the first 3 weeks of recovery, and improvement in functional ROM can be clearly seen following the successful MUA procedures. By week 20 after surgery, both patients reached the 50th percentile of functional ROM, illustrating the MUA allowed both patients to achieve an “average” knee recovery. When used in conjunction with clinical examination, we may be able to utilize daily-living kinematic data to predict poor outcomes earlier, which would lead to earlier intervention and improved long-term knee function. Furthermore, the implanted nature of the device promotes near 100% of compliance from patients, whereas compliance for in-person visits, PROMS completion and wearable technology is as low as 35% following surgery [14, 15, 16]. An additional promising capability of the Persona IQ is the ability to remotely follow-up patients long-term, daily throughout the 1st year after their surgery, and periodically throughout the following years.
The ability to monitor patients’ functional knee remotely with a smart implant as they complete their daily activities could become a valuable asset to orthopedic surgeons performing TKAs. Patients discussed in this case series had different demographic characteristics for gender, age, smoking status, and other medical histories. However, further research utilizing a larger population of patients will be necessary to demonstrate the value of providing early alerts to clinicians for patients at risk of severely limited ROM and potential MUA. The short-term benefit allows for an earlier intervention, such as MUA as in this case series, or other modalities (PT intensification for instance). A mid-term benefit of the technology, also illustrated in this case series, is the ability to monitor patients’ recovery after MUA and beyond the global period. Further research is necessary to confirm and expand on these early signals and demonstrate that this technology ultimately results in better outcomes.
This article demonstrates the clinical utility of an emerging technology that will permeate orthopedics in the future. This novel device not only monitors recovery but detects complications in the early post-operative period.
References
- 1.Abdul N, Dixon D, Walker A, Horabin J, Smith N, Weir DJ, et al. Fibrosis is a common outcome following total knee arthroplasty. Sci Rep 2015;5:16469. [Google Scholar]
- 2.Baum KS, Luo TD, Comadoll S, Marois A, Langfitt M, Shields J. Alternative technique for knee manipulation under anesthesia. Arthroplast Today 2018;4:452-3. [Google Scholar]
- 3.Fitzsimmons SE, Vazquez EA, Bronson MJ. How to treat the stiff total knee arthroplasty?: A systematic review. Clin Orthop Relat Res 2010;468:1096-106. [Google Scholar]
- 4.Cheuy VA, Foran JR, Paxton RJ, Bade MJ, Zeni JA, Stevens-Lapsley JE. Arthrofibrosis associated with total knee arthroplasty. J Arthroplasty 2017;32:2604-11. [Google Scholar]
- 5.Sharkey PF, Lichstein PM, Shen C, Tokarski AT, Parvizi J. Why are total knee arthroplasties failing today--has anything changed after 10 years? J Arthroplasty 2014;29:1774-8. [Google Scholar]
- 6.Arthrofibrosis Risk After ACL Reconstruction may not be Linked to Insurance Status n.d. Available from: https://www.healio.com/news/orthopedics/20180427/arthrofibrosis-risk-after-acl-reconstruction-may-not-be-linked-to-insurance-status [Last accessed on 2022 Oct 26]. [Google Scholar]
- 7.Anderson JG, Wixson RL, Tsai D, Stulberg SD, Chang RW. Functional outcome and patient satisfaction in total knee patients over the age of 75. J Arthroplasty 1996;11:831-40. [Google Scholar]
- 8.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: Who is satisfied and who is not? Clin Orthop Relat Res 2010;468:57-63. [Google Scholar]
- 9.Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L. Patient satisfaction after knee arthroplasty: A report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand 2000;71:262-7. [Google Scholar]
- 10.Hawker G, Wright J, Coyte P, Paul J, Dittus R, Croxford R, et al. Health-related quality of life after knee replacement. J Bone Joint Surg Am 1998;80:163-73. [Google Scholar]
- 11.Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: Patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res 2006;452:35-43. [Google Scholar]
- 12.Gunaratne R, Pratt DN, Banda J, Fick DP, Khan RJ, Robertson BW. Patient dissatisfaction following total knee arthroplasty: A systematic review of the literature. J Arthroplasty 2017;32:3854-60. [Google Scholar]
- 13.Ghomrawi HM, Lee LY, Nwachukwu BU, Jain D, Wright T, Padgett D, et al. Preoperative expectations associated with postoperative dissatisfaction after total knee arthroplasty: A cohort study. J Am Acad Orthop Surg 2020;28:e145-50. [Google Scholar]
- 14.Barrack TN, Abu-Amer W, Schwabe MT, Adelani MA, Clohisy JC, Nunley RM, et al. The burden and utility of routine follow-up at one year after primary arthroplasty. Bone Joint J 2020;102-B:85-9. [Google Scholar]
- 15.Constantinescu D, Pavlis W, Rizzo M, Vanden Berge D, Barnhill S, Hernandez VH. The role of commercially available smartphone apps and wearable devices in monitoring patients after total knee arthroplasty: A systematic review. EFORT Open Rev 2022;7:481-90. [Google Scholar]
- 16.Ramkumar PN, Haeberle HS, Ramanathan D, Cantrell WA, Navarro SM, Mont MA, et al. Remote patient monitoring using mobile health for total knee arthroplasty: Validation of a wearable and machine learning-based surveillance platform. J Arthroplasty 2019;34:2253-9. [Google Scholar]








