The fracture pattern along with the mechanism of injury is unique here.
Dr. Roop Bhushan Kalia, Department of Orthopaedics, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India. E-mail: roopkalia2003@yahoo.com
Introduction: Medial patellofemoral ligament (MPFL) prevents lateral dislocation of the patella and acts as a major stabilizer. The tear could be associated with osteochondral avulsion fractures; however, intra-articular split fractures are not seen. Here, we present one unusual case of such a presentation.
Case report: A 16-year-old male presented with a history of recurrent patellar dislocation and inability to bear weight following the last episode. The patient was diagnosed with an MPFL tear with an unusual intra-articular femoral condyle split fracture. The case had significant improvement in functional scores post-surgery.
Conclusion: In physically active populations, twisting of the knee could result in an MPFL tear, leading to recurrent patellar dislocation. The treatment remains ligament reconstruction, open, or arthroscopic. Associated intra-articular fractures are very rare with such injuries and need to be addressed due to the high rate of non-union.
Keywords: Medial patella-femoral ligament, MPFL tear, osteochondral fracture, Herbert screw fixation.
The medial patellofemoral ligament (MPFL) is a primary medial stabilizer of the patella, preventing its lateral dislocation [1, 2]. MPFL is responsible for 50% of the restraining force against lateral dislocation. MPFL extends from the medial surface of the patella up to Schottle’s point [3, 4]. MPFL tear may be associated with an osteochondral fracture (OCF) of the femur or patella [5]. OCF is suspected in the presence of an intra-articular hematoma. OCF associated with patellar dislocation ranges from 5% to 39%. OCF in a case of patellar instability may be due to high-velocity trauma, lower resilience of structure in the knee, or anatomical malformation. OCF needs early fixation to avoid loss of articular cartilage and prevent early osteoarthritis [6, 7, 8]. Treatment involves the debridement of fragments or surgical fixation. Surgical techniques include the use of screws or pins, drilling, osteochondral autograft, or allograft transplantation, or recently introduced biodegradable pins. Small osteochondral defects involving <20% of the weight-bearing articular surface can be managed conservatively or proceeded with surgical debridement [9, 10]. This unique case report supports a rare diagnosis of an MPFL tear associated with an intra-articular osteochondral axial split fracture of the lateral femoral condyle (LFC). Available literature supports that MPFL tear associated with any intra-articular fractures is a rare clinical diagnosis; hence, this case remains important. The rare LFC intra-articular axial split OCF is hence being termed a knee “Trapdoor” fracture.
A 16-year-old male presented with complaints of pain in his right knee and difficulty in bearing weight for the past 20 days following a twisting injury of the knee, with an outward dislocation of the patella. The patient had a history of recurrent patellar dislocation, with three episodes in the past year. The first episode was due to sudden stop and twist movement of the knee followed by spontaneous relocation of the patella. The second episode occurred after 9 months while running. After both episodes, the patient could bear weight. However, the patient could not bear weight on his right leg after the last episode. On examination, there was mild wasting of the right quadriceps and tenderness over medial and lateral joint lines. Flexion was mildly restricted compared to the contralateral side. Patellar effusion and patellar tap were negative. The patellar apprehension test was positive without any evidence of hyperlaxity syndrome. Radiograph revealed patella alta with a high Insall-Salvati index and Caton-Deschamps index. An intra-articular osteochondral axial split fracture of the LFC was seen. Computed tomography (CT) scan confirmed the OCF, which was minimally displaced. On CT, the TT-TG distance was 14.4 mm, which was suggestive of an optimal position of the tibial tuberosity. Magnetic resonance imaging (MRI) revealed an MPFL tear with evidence of LFC split fracture (Fig. 1).  The patient was planned for MPFL reconstruction with the fixation of the intra-articular split fracture. The fracture was approached with the lateral parapatellar incision. The fracture was anatomically reduced and fixed with a guide wire in its position and then fixed with 3 headless threaded screws. Semi-tendinosus graft was harvested, and the double-looped graft was noted to be 6 mm, and the medial patellar facet was identified and exposed. Two tunnels were prepared on the medial aspect of the patella using a 4.5 mm drill bit over a 2 mm guide wire, and the graft was looped. On the lateral view under fluoroscopic guidance, Schöttle’s point was identified, and the guide wire was passed. The point of isometry was confirmed through the knee range. This was followed by drilling it with a 4.5 mm drill bit and a 6 mm reamer, and the graft was shuttled through this tunnel and fixed at an adequate tension with a bioabsorbable interference screw (Fig. 2).
The patient was planned for MPFL reconstruction with the fixation of the intra-articular split fracture. The fracture was approached with the lateral parapatellar incision. The fracture was anatomically reduced and fixed with a guide wire in its position and then fixed with 3 headless threaded screws. Semi-tendinosus graft was harvested, and the double-looped graft was noted to be 6 mm, and the medial patellar facet was identified and exposed. Two tunnels were prepared on the medial aspect of the patella using a 4.5 mm drill bit over a 2 mm guide wire, and the graft was looped. On the lateral view under fluoroscopic guidance, Schöttle’s point was identified, and the guide wire was passed. The point of isometry was confirmed through the knee range. This was followed by drilling it with a 4.5 mm drill bit and a 6 mm reamer, and the graft was shuttled through this tunnel and fixed at an adequate tension with a bioabsorbable interference screw (Fig. 2).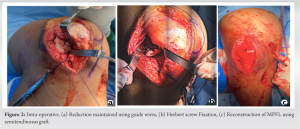 Wounds were closed, and post-operative radiographs were obtained showing adequately fixed OCF (Fig. 3). The patient was kept on non-weight-bearing mobilization on a walking frame, and isometric quadriceps training and closed chain knee range of motion exercises were started immediately.
Wounds were closed, and post-operative radiographs were obtained showing adequately fixed OCF (Fig. 3). The patient was kept on non-weight-bearing mobilization on a walking frame, and isometric quadriceps training and closed chain knee range of motion exercises were started immediately. 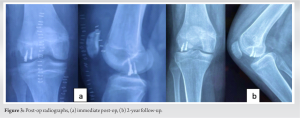 Postoperatively, the surgical wounds healed without any complications, and he was allowed partial weight-bearing beyond 6 weeks with open chain exercises and strength training. He started to fully weight bear without any support at post-operative 3 months. Final follow-up at 2 years showed an increase in Lysholm-Tegner score from 68 to 94, and IKDC score from 60 to 92, suggesting higher functional and post-surgery excellent clinical outcomes. The radiograph obtained at the final follow-up was satisfactory (Fig. 3).
Postoperatively, the surgical wounds healed without any complications, and he was allowed partial weight-bearing beyond 6 weeks with open chain exercises and strength training. He started to fully weight bear without any support at post-operative 3 months. Final follow-up at 2 years showed an increase in Lysholm-Tegner score from 68 to 94, and IKDC score from 60 to 92, suggesting higher functional and post-surgery excellent clinical outcomes. The radiograph obtained at the final follow-up was satisfactory (Fig. 3).
The present case reports a unique fracture pattern where the MPFL tear is associated with an intra-articular LFC axial split fracture. We hypothesized that the mechanism of injury could be a sudden shearing force over the LFC with an inward twisting of the knee in terminal degrees of flexion simultaneously with a high-intensity valgus force. This caused the patella to be suddenly entrapped at the lateral femoral gutter in front of the LFC, resulting in an intra-articular axial split fracture. We termed this unique fracture a knee “Trap door” fracture of the LFC. Our reconstruction technique was standard and highlights an excellent surgical outcome. In an MRI study done by Guerrero et al., MPFL was found torn at patellar attachment in 93/195 (47%), femoral attachment in 50/195 (6%), both in 26/195 (3%), and MPFL attenuation without rupture in 26/195 (13%). Furthermore, this study concluded that MPFL tear was associated with osteochondral lesions in 96/195 knees (49%) [11]. MPFL is a major patella-femoral joint stabilizer, and it acts as a medial check rein for the patella during the early knee flexion before it engages in the trochlea, thereby inhibiting its lateral translation and mal-tracking [12]. Inherent weakness or traumatic rupture can lead to recurrent and habitual patellar dislocation. If not addressed at the right time, traumatic lesions to this ligament can lead to recurring dislocation in 14–44% of cases, osteochondral lesions, and eventually, early osteoarthritis. MPFL reconstruction has become popular day by day by restoring the passive medial restraint of the patellofemoral joint [13, 14, 15, 16]. The basket weave technique for the reconstruction of MPFL is used without implants or anchors and has good surgical outcomes. No tunnels are made in the femur or patella, thus no tunnel-related complications or physical disruptions [17]. In our case, the MPFL was reconstructed with a semi-tendinosus graft and suture anchor, and the osteochondral fragment was fixed by Herbert’s screw. A suture technique of MPFL repair was described in 18 patients enrolled from January 2011 and December 2015 where the OCF was repaired by polydioxanone suture, and MPFL was either repaired or reconstructed with semi-tendinosus autograft. There was no recurrent dislocation after surgery. 6 patients were able to perform activities of daily living independently and 12 patients returned to physical activity. At a mean follow-up of 36 months, the Lysholm score and Kujala Sacore increased from a mean of 37.6 and 45.9 preoperatively to 80.9 and 89.4 postoperatively, respectively [18]. In our case, the Lysholm and IKDC scores improved from 68 and 60 to 94 and 92, respectively.
MPFL injury is associated with an avulsion fracture of the patella and OCF involving the articular surface and medial facet of the patella. The LFC osteochondral knee trap door fracture experienced by us is a rare entity and fixation of the OCF with headless screws while maintaining the articular congruity, and reconstruction of MPFL is a reliable option and is associated with improved clinical and radiological outcome.
This case report describes a unique fracture pattern seen along with the medial-patellofemoral ligament tear and how a timely and appropriate treatment could gain back functionality in these patients. The fracture pattern is hypothesized to be due to the patella getting entrapped in front of the LFC during sudden valgus force in a flexed knee; hence, we would like to coin this as a “knee trap-door fracture”.
References
- 1.Vitale TE, Mooney B, Vitale A, Apergis D, Wirth S, Grossman MG. Physical therapy intervention for medial patellofemoral ligament reconstruction after repeated lateral patellar subluxation/dislocation. Int J Sports Phys Ther 2016;11:423-35. [Google Scholar]
- 2.Krebs C, Tranovich M, Andrews K, Ebraheim N. The medial patellofemoral ligament: Review of the literature. J Orthop 2018;15:596. [Google Scholar]
- 3.Burrus MT, Werner BC, Cancienne JM, Gwathmey FW, Diduch DR. MPFL graft fixation in low degrees of knee flexion minimizes errors made in the femoral location. Knee Surg Sports Traumatol Arthrosc 2017;25:3092-8. [Google Scholar]
- 4.Kyung HS, Kim HJ. Medial patellofemoral ligament reconstruction: A comprehensive review. Knee Surg Relat Res 2015;27:133-40. [Google Scholar]
- 5.Aitchison AH, Perea SH, Schlichte LM, Green DW. Medial patellofemoral ligament reconstruction with simultaneous osteochondral fracture fixation is an effective treatment for adolescent patellar dislocation with osteochondral fractures. J Child Orthop 2022;16:393-400. [Google Scholar]
- 6.Li J, Chen C, Zhou H, Zhai J, Zhao H, Li L. Anatomic risk factors for osteochondral fracture of acute first-time patellar dislocation in adolescents: A retrospective magnetic resonance imaging study. Evid Based Complement Alternat Med 2022;2022:6723326. [Google Scholar]
- 7.Małecki K, Pruchnik-Witosławska K, Gwizdała D, Grzelak P, Flont P, Niedzielski KR. Clinical results and MRI evaluation of patellar osteochondral fracture fixation following patellar dislocation. Biomed Res Int 2019;2019:7943636. [Google Scholar]
- 8.Repo JP, Uimonen MM, Nevalainen MT, Nurmi H, Ponkilainen VT, Tuominen A, et al. Outcomes following the operative treatment of intra-articular fracture combined with medial patellofemoral ligament reconstruction after patellar dislocation. Knee Surg Relat Res 2022;34:21. [Google Scholar]
- 9.Howell M, Liao Q, Gee CW. Surgical management of osteochondral defects of the knee: An educational review. Curr Rev Musculoskelet Med 2021;14:60-6. [Google Scholar]
- 10.Winthrop Z, Pinkowsky G, Hennrikus W. Surgical treatment for osteochondritis dessicans of the knee. Curr Rev Musculoskelet Med 2015;8:467-75. [Google Scholar]
- 11.Guerrero P, Li X, Patel K, Brown M, Busconi B. Medial patellofemoral ligament injury patterns and associated pathology in lateral patella dislocation: An MRI study. Sports Med Arthrosc Rehabil Ther Technol 2009;1:17. [Google Scholar]
- 12.Loeb AE, Tanaka MJ. The medial patellofemoral complex. Curr Rev Musculoskelet Med 2018;11:201-8. [Google Scholar]
- 13.Batra S, Arora S. Habitual dislocation of patella: A review. J Clin Orthop Trauma 2014;5:245-51. [Google Scholar]
- 14.Migliorini F, Marsilio E, Cuozzo F, Oliva F, Eschweiler J, Hildebrand F, et al. Chondral and soft tissue injuries associated to acute patellar dislocation: A systematic review. Life 2021;11:1360. [Google Scholar]
- 15.Bruns J, Werner M, Habermann C. Osteochondritis dissecans: Etiology, pathology, and imaging with a special focus on the knee joint. Cartilage 2018;9:346-62. [Google Scholar]
- 16.Reddy KR, Reddy NS. Trochleoplasty and medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Indian J Orthop 2012;46:242-5. [Google Scholar]
- 17.Kodkani PS. Basket-Weave technique for medial patellofemoral ligament reconstruction. Arthrosc Tech 2015;4:e279-86. [Google Scholar]
- 18.Li ZX, Song HH, Wang Q, Guo DM. Clinical outcomes after absorbable suture fixation of patellar osteochondral fracture following patellar dislocation. Ann Transl Med 2019;7:173. [Google Scholar]