Acute reconstruction of the forearm interosseous membrane with a Mini TightRope suture button construct is a technique to be considered in the early management of Essex Lopressti injuries.
Dr. Nailah F Mubin, Department of Orthopaedic Surgery, Nassau University Medical Center, 2201 Hempstead Turnpike, East Meadow, NY 11554, USA. E-mail: drnmubin@gmail.com
Introduction: Essex Lopresti fractures are rare injuries of the forearm. Extent of damage to the interosseous membrane (IOM) in this setting is variable and can lead to disabling sequelae when not recognized and managed appropriately. While chronic reconstruction for longitudinal radioulnar dissociation is well studied, acute reconstruction of the membrane is infrequently documented and surgical techniques vary. There are only five documented cases of acute IOM reconstruction for Essex Lopresti injuries (ELIs). This is the first described case using a mini suture-button construct in conjunction with a radial head replacement and distal radioulnar joint (DRUJ) pinning, while also providing long-term radiographic and functional follow-up of 2 years.
Case Report: We present a case of a 40-year-old male who sustained an Essex Lopresti fracture that was acutely recognized and surgically managed with a radial head replacement, DRUJ pinning, and acute reconstruction of the IOM with a Mini TightRope suture button construct. We also provide a post-operative rehabilitation protocol with early range of motion and pin removal. At our final 2-year postoperative follow–up, the patient demonstrated excellent functional outcomes.
Conclusion: This case illustrates that a CMC Mini TightRope can be used for acute reconstruction of the IOM in the setting of ELIs which allows for early range of motion and DRUJ pin removal due to the maintenance of longitudinal radioulnar reduction.
Keywords: Interosseous membrane, essex lopresti, reconstruction, radioulnar joint.
Essex lopresti injuries (ELIs) to the forearm are classically defined as fracture of the radial head, distal radioulnar joint (DRUJ) injury, and disruption of the interosseous membrane (IOM) [1, 2, 3]. The usual mechanism for such an injury is axial compression to the forearm while the elbow is extended [2, 3]. Extent of injury to the IOM is variable and thus contributes to a reported 60% of missed diagnoses at initial presentation [4, 5]. While there is a consensus for IOM reconstruction in chronic cases of longitudinal radioulnar instability [3, 6, 7, 8], there is minimal information regarding support for acute IOM reconstruction and surgical technique for such cases [5]. Prior literature in this area has focused on cadaveric, biomechanic, or chronic reconstruction studies [9, 10, 11, 12]. We found only five documented cases of acute reconstruction with varying surgical techniques with a maximum of 1-year follow-up [8, 13, 14, 15]. Of these, one uses an isolated ankle syndesmosis suture-button construct [13], and the other uses a FiberTape-dog button construct with a radial head replacement [15]. We present a case of early diagnosis of IOM disruption in the setting of ELI, the surgical technique for acute reconstruction of IOM with the CMC Mini TightRope(Arthrex Inc., Naples, FL).
A 40-year-old male presented to the emergency department with complaints of left arm pain after a pedestrian struck incident while walking across the street. Initial radiographs demonstrated a comminuted radial head fracture, radial styloid fracture, and ulnar styloid fracture along with positive ulnar variance (Fig. 1). On physical examination, the patient was neurovascular intact but with tenderness to the elbow, wrist, and along the volar aspect of the forearm. The patient also had a positive piano key test at the wrist. The patient was subsequently diagnosed with an Essex Lopressti Injury, placed into a sugar-tong splint, and indicated for surgical fixation.
On physical examination, the patient was neurovascular intact but with tenderness to the elbow, wrist, and along the volar aspect of the forearm. The patient also had a positive piano key test at the wrist. The patient was subsequently diagnosed with an Essex Lopressti Injury, placed into a sugar-tong splint, and indicated for surgical fixation.
Surgery
A standard Kocher approach to the elbow joint was used to expose the radial head fracture. Comminuted fragments and loose bodies within the joint were removed. At this point, an intraoperative radius pull test [16] demonstrated greater than 3 mm of proximal migration, confirming injury to the IOM. The radial head ostectomy was then completed followed by a radial head replacement. Reconstruction of the IOM was accomplished using a CMC Mini TightRope (Arthrex Inc., Naples, FL) similar to as described by Meals et al. [11]. The ulna was marked at 1/3rd from the ulnar styloid, and the radius was marked at 3/5th from the radial styloid. Blunt dissection at these sites was carried out to the shafts while being careful to protect sensory nerve branches. Then, with the forearm in pronation, a 1.1 mm K wire from the CMC Mini TightRope (Arthrex Inc., Naples, FL) set was advanced obliquely under fluoroscopic guidance through the cortices of the radius and ulna, angling distally. A 2.0 mm cannulated drill was used to overdrill the K-wire. The tightrope was then inserted using a suture passer and the second button was loaded onto the suture and then tensioned against the ulnar shaft under fluoroscopy. Finally, the DRUJ and radial styloid were then close reduced and pinned with three 1.6 mm Kirschner wires. Final intraoperative fluoroscopy images are shown in Fig. 2.
Follow-up
The patient was postoperatively placed into a hinged elbow brace locked at 90° of flexion for 1 week. The brace was then unlocked in flexion and limited to 30° of extension for the 2nd week. Extension was increased by 10° each week and subsequently unlocked by the 5th week. Pins were removed at 4 weeks post-operative, and physical therapy was initiated for elbow range of motion (ROM) and forearm pronosupination. Strengthening was initiated at 8 weeks postoperatively, and the brace was discontinued at 3-month post-operative. Table 1 documents DASH scores, and ROM measurements of the wrist, elbow, and forearm.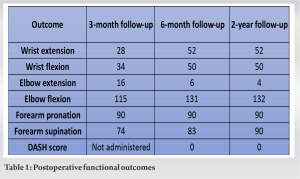 Figs 3 and 4 illustrate radiographic follow-up at 6 months and 2 years.
Figs 3 and 4 illustrate radiographic follow-up at 6 months and 2 years.
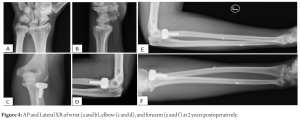
ELIs are complicated and disabling forearm injuries and can lead to poor outcomes if not appropriately managed [4, 7]. Disruption of the IOM in this injury can lead to various symptomatology. Initial presentation may have subtle signs to the extent of the injury such as dorsal forearm tenderness and wrist pain with palpation [5]. Chronic injuries may present with symptoms related to persistent longitudinal instability to the forearm such as lateral elbow pain and ulnar-sided wrist pain due to ulnar abutment [2]. Acute reconstruction of the IOM is seldom documented [8, 13, 14, 15]. This case is unique as it details acute reconstruction of the IOM with the CMC Mini TightRope(Arthrex Inc., Naples, FL), a rehab protocol, and long-term patient outcome. The major function of the IOM is to transmit load from the wrist to elbow, with transfer of load between the radius and ulna while maintaining forearm and DRUJ stability [15, 17]. The anatomical composition of the IOM includes the proximal oblique cord, the dorsal oblique accessory cord, the central band, accessory bands, and the distal oblique bundle [5, 15]. With the central band being the widest and thickest ligament, it is the major load-bearing component [5, 6]. Its approximate position and orientation is a volar origin at 3/5th from the distal radius with dorsal insertion on the ulna 1/3rd from distal ulna with an angle of 21° oblique to the forearm’s longitudinal axis [6]. This allows the fibers of the central band to function to resist both longitudinal dislocation forces and transverse radioulnar splaying during axial loading [18]. Biomechanical studies on the IOM have illustrated the importance of its role in forearm stability. Birkbeck et al. [19] demonstrated that, with a transected IOM, the radius and ulna bore load independently. Hotchkiss et al. [20] found that, with a radial head excised, the IOM bears 90% of axial load through the forearm, 71% from the central band alone. While the radial head functions as the primary restraint to proximal migration of the radius, the IOM and triangular fibrocartilage complex are important secondary stabilizers if the radial head is absent [6, 21]. Rabinowitz et al. [21] demonstrated that proximal migration is minimal under an axial load when both are intact; however, when compromised, proximal migration of the radius occurs with resultant increased radiocapitellar joint forces and load through the radius. Historically, ELIs are addressed with radial head fixation or replacement and DRUJ reduction [6]. When the disruption of the IOM persists beyond the initial injury period, lack of restoration of load transfer leads to longitudinal radioulnar dissociation (LRUD) [17]. There is a strong support for central band reconstruction in the setting of chronic cases of LRUD due to its potential to restore longitudinal stability and decrease the sequelae of LRUD such as distal ulnar impaction and radiocapitellar joint overload [6, 7, 12]. However, the low healing potential of the central band and documentation of poorer outcomes in the setting of delayed diagnosis support a role for acute IOM reconstruction [4, 7]. In current literature, there is no consensus regarding acute reconstruction of the IOM in such injuries. Options for reconstruction based on cadaveric studies or chronic cases include suture button construct, bone tendon bone autograft, achilles allograft, or autograft with various tendons such as palmaris or flexor carpi radialis [2, 7, 12, 22]. Direct repair can also be considered in cases where the central band is torn from its ulnar border [3, 23]. In previously documented cases of acute reconstruction of the IOM, surgeons have used ankle Syndesmosis TightRope (Arthrex Inc., Naples, FL) [13], Fiber-Tape (Arthrex Inc., Naples, FL) [15], pronator teres autograft [14], cadaveric tendon allograft [8], and Ultratape (Smith and Nephew, Watford, UK) [8]. To our knowledge, our case is the first to document the use of the CMC Mini TightRope (Arthrex Inc., Naples, FL) for IOM reconstruction with a longer term outcome of 2 years postoperatively. The CMC Mini TightRope (Arthrex Inc., Naples, FL) is classically indicated for thumb suspension after resection of the trapezium in thumb CMC joint arthroplasty [24]. In our case, however, we used it to provide a tensioned reduction of the radius and ulna and to reinforce their longitudinal stability. This allowed us to remove pins earlier at 4 weeks postoperatively and begin ROM ultimately contributing to improved patient functional outcomes. A similar suture button construct has previously been investigated in cadaveric studies. Drake et al. [9] compared forearms with excised radial heads and a sectioned IOM found that a Mini TightRope restored stability equal to that of an intact IOM. Kam et al. [10] found that Mini TightRope reconstruction significantly reduced distal ulnar impaction forces and radioulnar displacement when tested without a radial head replacement. Further reduction was obtained when used in conjunction with a radial head implant. Limitations of this case include that, despite our attempt to recreate the anatomic orientation of the central band, our oblique axis was closer to 40° rather than 20°. In addition, as seen in follow-up radiographs, slight increase in ulnar variance was observed as compared to intraoperative images, demonstrating mild loss of longitudinal radioulnar reduction. However, variations in radiographic technique, patient positioning, and subsequent dynamic ulnar variance [25] make it difficult to accurately quantify the difference. Despite this, with the long-term follow up obtained, we are able to show minimal change between the 6 months and 2-year time points, confirming the overall maintained stability of the forearm with the surgical technique and rehab protocol employed and as compared to the time of injury. This was further reflected in the patient’s functional measurements and asymptomatic presentation. Randomized controlled studies regarding the use of acute IOM reconstruction would be beneficial to further support the findings of this case presentation.
This case demonstrates the importance of early diagnosis of IOM damage in the setting of ELI and the benefits of early ROM and pin removal with acute reconstruction of IOM using a suture button construct. Excellent ROM, decent maintenance of longitudinal radioulnar reduction, and painless function were observed at the final follow-up of 2-year postoperatively.
Chronic effects of persistent radioulnar dissociation after ELI can lead to poor outcomes. Acute reconstruction of the forearm IOM in the setting of ELIs with a Mini TightRope suture button construct can allow for early DRUJ pin removal and ROM due to maintained radioulnar longitudinal stability with subsequent great functional outcomes.
References
- 1.Essex-Lopresti P. Fractures of the radial head with distal radio-ulnar dislocation; report of two cases. J Bone Joint Surg Br 1951;33B:244-7. [Google Scholar]
- 2.Matson AP, Ruch DS. Management of the Essex-Lopresti injury. J Wrist Surg 2016;5:172-8. [Google Scholar]
- 3.Adams JE, Culp RW, Osterman AL. Interosseous membrane reconstruction for the Essex-Lopresti injury. J Hand Surg Am 2010;35:129-36. [Google Scholar]
- 4.Trousdale RT, Amadio PC, Cooney WP, Morrey BF. Radio-ulnar dissociation. A review of twenty cases. J Bone Joint Surg Am 1992;74:1486-97. [Google Scholar]
- 5.Masouros PT, Apergis EP, Babis GC, Pernientakis SS, Igoumenou VG, Mavrogenis AF, et al. Essex-Lopresti injuries: An update. EFORT Open Rev 2019;4:143-50. [Google Scholar]
- 6.Adams JE, Steinmann SP, Osterman AL. Management of injuries to the interosseous membrane. Hand Clin 2010;26:543-8. [Google Scholar]
- 7.Marcotte AL, Osterman AL. Longitudinal radioulnar dissociation: Identification and treatment of acute and chronic injuries. Hand Clin 2007;23:195-208, vi. [Google Scholar]
- 8.Fontana M, Cavallo M, Bettelli G, Rotini R. Diagnosis and treatment of acute Essex-Lopresti injury: Focus on terminology and review of literature. BMC Musculoskelet Disord 2018;19:312. [Google Scholar]
- 9.Kam CC, Jones CM, Fennema JL, Latta LL, Ouellette EA, Evans PJ. Suture-button construct for interosseous ligament reconstruction in longitudinal radioulnar dissociations: A biomechanical study. J Hand Surg Am 2010;35:1626-32. [Google Scholar]
- 10.Drake ML, Farber GL, White KL, Parks BG, Segalman KA. Restoration of longitudinal forearm stability using a suture button construct. J Hand Surg Am 2010;35:1981-5. [Google Scholar]
- 11.Meals CG, Forthman CL, Segalman KA. Suture-button reconstruction of the interosseous membrane. J Wrist Surg 2016;5:179-83. [Google Scholar]
- 12.Gaspar MP, Kane PM, Pflug EM, Jacoby SM, Osterman AL, Culp RW. Interosseous membrane reconstruction with a suture-button construct for treatment of chronic forearm instability. J Shoulder Elbow Surg 2016;25:1491-500. [Google Scholar]
- 13.Brin YS, Palmanovich E, Bivas A, Sagiv P, Kotz E, Nyska M, et al. Treating acute Essex-Lopresti injury with the TightRope device: A case study. Tech Hand Up Extrem Surg 2014;18:51-5. [Google Scholar]
- 14.Adams JE, Culp RW, Osterman AL. Central band interosseous membrane reconstruction for forearm longitudinal instability. J Wrist Surg 2016;5:184-7. [Google Scholar]
- 15.Matthias R, Wright TW. Interosseous membrane of the forearm. J Wrist Surg 2016;5:188-93. [Google Scholar]
- 16.Smith AM, Urbanosky LR, Castle JA, Rushing JT, Ruch DS. Radius pull test: Predictor of longitudinal forearm instability. J Bone Joint Surg Am 2002;84-A:1970-6. [Google Scholar]
- 17.Rozental TD, Beredjiklian PK, Bozentka DJ. Longitudinal radioulnar dissociation. J Am Acad Orthop Surg 2003;11:68-73. [Google Scholar]
- 18.Pfaeffle HJ, Fischer KJ, Manson TT, Tomaino MM, Woo SL, Herndon JH. Role of the forearm interosseous ligament: Is it more than just longitudinal load transfer? J Hand Surg Am 2000;25:683-8. [Google Scholar]
- 19.Birkbeck DP, Failla JM, Hoshaw SJ, Fyhrie DP, Schaffler M. The interosseous membrane affects load distribution in the forearm. J Hand Surg Am 1997;22:975-80. [Google Scholar]
- 20.Hotchkiss RN, An KN, Sowa DT, Basta S, Weiland AJ. An anatomic and mechanical study of the interosseous membrane of the forearm: Pathomechanics of proximal migration of the radius. J Hand Surg Am 1989;14 2 Pt 1:256-61. [Google Scholar]
- 21.Rabinowitz RS, Light TR, Havey RM, Gourineni P, Patwardhan AG, Sartori MJ, et al. The role of the interosseous membrane and triangular fibrocartilage complex in forearm stability. J Hand Surg Am 1994;19:385-93. [Google Scholar]
- 22.Masouros PT, Apergis EP, Mavrogenis AF, Babis GC, Artemi DK, Nikolaou VS. Reconstruction of the forearm interosseous membrane: A biomechanical study of three different techniques. J Hand Surg Eur Vol 2020;45:360-8. [Google Scholar]
- 23.Failla JM, Jacobson J, van Holsbeeck M. Ultrasound diagnosis and surgical pathology of the torn interosseous membrane in forearm fractures/dislocations. J Hand Surg Am 1999;24:257-66. [Google Scholar]
- 24.Mini Tightrope® CMC Technique. United States: Arthrex. Available from: https://www.arthrex.com/hand-wrist/mini-tightrope-cmc-technique [Last accessed on 2023 Apr 06]. [Google Scholar]
- 25.Epner RA, Bowers WH, Guilford WB. Ulnar variance--the effect of wrist positioning and roentgen filming technique. J Hand Surg Am 1982;7:298-305. [Google Scholar]









