Arthroscopic meniscal trephination, a novel surgical technique for the management of symptomatic meniscal degeneration, has shown to have less negative long-term effects compared to a meniscectomy in young patients.
Dr. Muhyeddine Al-Taki, Department of Orthopaedic Surgery, American University of Beirut Medical Center, Beirut, Lebanon. E-mail: altakiortho@gmail.com
Introduction: Meniscal pathology constitutes a major reason for a vast number of patients suffering from knee pain. It is, in general, attributed either to meniscal tearing or degeneration. Debridement and partial meniscectomy, or repair, when possible, is the mainstay surgical approach for refractory knee pain from meniscal degeneration or tears. Sometimes, the patient has clinical symptoms of meniscal pathology, but despite those highly suggestive clinical symptoms, the patient turns out, during knee arthroscopy, to have meniscal degeneration and hardening of the meniscus without frank tearing of the meniscus
Surgical Technique: To initiate meniscal trephination, we first conduct a diagnostic knee arthroscopy to examine the suprapatellar space, the gutters, and the anterior knee space for any pathologies. Following this, both menisci are inspected for any signs of tearing or hardening. For the purposes of our study, the medial meniscus is considered pathological if it shows signs of degeneration or hardening, which then justifies our intervention. An 18-gauge spinal needle, manually bent for the procedure, is inserted through the portal to perform trephination on the hardened menisci. Care is taken to adequately space the needle insertion points to prevent accidental tearing. Our trephination technique aims to soften the meniscus, facilitating its ability to compact and compress when patients ambulate. Additionally, the needle insertion points help attract blood flow to the meniscus, thereby enriching it with growth factors and stem cells that may aid in improving the degenerative condition.
Conclusion: Meniscal trephination is benign and effective for meniscal degenerative pathologies. The procedure allows for a healthier meniscus, free from degeneration, that would otherwise disable patients. The intervention does not have long-term adverse effects. To this end, more comparative trials are required to confirm the effectiveness of the technique and to ensure minimal to no associated side effects.
Keywords: Trephination, Meniscus, Knee, Degeneration
The menisci have a vital role in balancing and securing stability across the knee joint [1]. They work as a shock absorber, distributing load past its surface area and enhancing lubrication to the knee joint. Its complex anatomy, unorthodox chondral structuring, and relatively minimal vascularity render their treatment and repair burdensome. Meniscal pathology is the most common knee injury [2]. The cumulative risk of needing surgery between the ages of 10 and 64 can reach up to 15%, with more than 1 million surgeries performed annually in the United States. [3]. However, many patients who present with chronic knee pain attributed to meniscal injury; where imaging shows a meniscal tear, often turn out to have either degeneration or a false-negative result during diagnostic arthroscopy [4]. For the symptomatic meniscal degeneration/tearing, debridement/partial meniscectomy is the mainstay treatment. Classically, patients who are found to have no meniscal tear during arthroscopy often receive no intervention beyond the diagnostic aspect of the procedure. Postoperatively, they are typically sent for physical therapy and may also be prescribed a short course of non-steroidal anti-inflammatory medications. They may also be offered intra-articular injections to alleviate pain. Many of these patients do not respond well to the treatment and continue to experience knee pain. Some may even undergo partial meniscectomy based on the premise that the meniscus is hardened and degenerative. This puts them at risk of developing osteoarthritis in the years to come. To the best of our knowledge, there is no well-defined treatment for symptomatic meniscal degeneration and hardening. We introduce a new technique, called meniscal trephination, for treating symptomatic meniscal hardening in the absence of obvious tears in the meniscus, as identified during knee arthroscopy. This technique involves puncturing the hardened meniscal tissue with a spinal needle, which helps in softening the meniscus. Additionally, it facilitates the generation of a blood-rich environment containing growth factors and cells with healing potential. We will review the relevant literature to highlight the indications and implications of this technique both for preserving the meniscus and as a treatment for symptomatic degenerated menisci.
Patient selection
Preoperatively, patients who present with knee pain and clinical signs of meniscal pathology typically undergo magnetic resonance imaging (MRI) to diagnose a potential meniscal tear. If a diagnosis is made, the decision to proceed with arthroscopic trephination is taken intraoperatively for patients already scheduled for knee arthroscopy. If a meniscal tear is identified during the arthroscopy, repair is performed for reparable tears, while debridement and partial meniscectomy are carried out for non-reparable tears. However, if no tear is found during arthroscopy and the meniscus shows signs of degeneration and hardening, then trephination is indicated and performed. Indicators of meniscal degeneration include a yellowish discoloration of the meniscus, hardening of the meniscus when tested with a hook probe, and a convex surface appearance as opposed to the normal concave surface of the meniscus.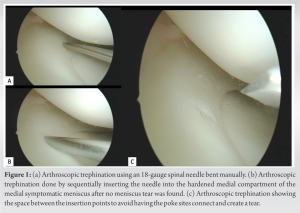
Surgical Technique
Under tourniquet control, diagnostic knee arthroscopy is done using the standard anterolateral and anteromedial portals. The suprapatellar space, the gutters, and the anterior knee space are checked. Both menisci are inspected and probed checking for any tear. If no meniscal tear is found, the meniscus on the symptomatic side which is the medial meniscus in our series is checked for any signs of degeneration and hardening. If the meniscus is deemed pathologic, we proceed with trephination. This novel technique of trephination is performed using an 18-gauge spinal needle which we bend manually and insert through the portal (Fig. 1a). Using this needle, targeted trephination is performed on the hardened areas of the meniscus. The procedure involves sequentially inserting the needle into the meniscus (Fig. 1b). Care is taken to space the insertion points sufficiently apart to avoid having the poke sites connect and create a tear (Fig. 1c). The rationale behind the technique is that trephination will soften the meniscus and help the degenerated and thickened meniscal tissue to compact and compress when patients move around in the early post-operative period. Moreover, the holes created are likely to recruit blood from the peripheral aspects of the meniscus, bringing with it growth factors and mesenchymal stem cells that may improve the degenerated areas of the meniscus. If parapatellar plicae are found, they are divided using a shaver, followed by a coblator for hemostasis.
Post-operative management
No specific physical therapy protocol is required for meniscal trephination. However, similar to meniscectomies, it is advised to initiate physical therapy immediately postoperatively. The focus should be on strengthening the hamstrings and quadriceps, improving the knee’s range of motion, and encouraging full weight-bearing ambulation as tolerated. This approach ensures that the patient maintains full range of motion and adequate muscular strength. Patients are typically discharged on the same day of the surgery or one day postoperatively. They are sent home with prescriptions for pain medication and physical therapy. If tolerated, patients are also prescribed a 10-day course of non-steroidal anti-inflammatory drugs. Upon suture removal two weeks post-operation, and during the follow-up examination six weeks post-operation, patients generally report the absence of knee pain and indicate significant improvements and positive outcomes. A prospective study would be valuable for assessing the long-term outcomes of meniscal trephination compared to meniscectomies.
The exact criteria for determining which type of meniscal tear are amenable to meniscal preservation remain unclear. Additionally, there is no consensus on when to opt for meniscal repair versus meniscectomy [5]. Shelbourne et al. argued that meniscal removal is equivalent to repair [6]. Conversely, trephination of peripheral, non-degenerative, vertical posterior horn tears has shown good functional outcomes when performed alongside anterior cruciate ligament (ACL) reconstruction, compared to controls [6]. Older descriptions note that trephination of the bed of torn menisci induces bleeding and promotes healing [7]. Among patients who underwent meniscal trephination during meniscal repair, 6% needed subsequent arthroscopy, compared to 10.6% when the tear was left untreated and 13.6% when the tear was repaired [8]. This evidence prompted a shift towards more frequent use of meniscal trephination in managing meniscal tears. Trephination creates vascular access channels by removing a core of tissue from the periphery of the meniscus tear, connecting avascular lesions to the peripheral blood supply [7]. This initiates bleeding and promotes healing. Despite the beneficial functional outcomes discussed in the literature, no study, to the best of our knowledge, has investigated the benefits of trephination on degenerated, hardened, but non-torn menisci. Patients sometimes exhibit clinical symptoms of meniscal pathology, such as medial or lateral-sided pain, joint line tenderness, pain with deep flexion, and antalgic gait, despite arthroscopic findings of meniscal degeneration rather than tears. Trephination of degenerative menisci provides the significant advantage of relieving patient pain while preserving the meniscus and potentially preventing accelerated arthritis, which is often seen in patients undergoing partial meniscectomy. Our technique aims to induce injury using a needle on the degenerated peripheral sites of the meniscus, creating vascular channels that accelerate the recruitment of blood vessels and establish a regenerative niche. This process helps to recruit growth factors and mesenchymal stem cells to the site of degeneration, redirecting the body’s healing mechanisms to these induced sterile injuries. The technique also softens the hardened meniscus. Patients report immediate pain relief without signs of inflammation such as joint redness. Importantly, meniscal function is preserved without the need for partial meniscectomy. Studies by Kaminski et al. and Shelbourne et al. have explored the role of trephination in different contexts but lack comprehensive control groups and long-term follow-ups [1, 6]. Fox et al. demonstrated the efficacy of meniscal trephination in treating incomplete meniscal tears, with a majority of patients reporting excellent or good results [7]. Our experience supports these findings, as none of our patients who underwent meniscal trephination had limitations in range of motion or weight-bearing postoperatively. This is consistent with other studies showing that trephination doesn’t compromise functional outcomes, unlike other repair strategies that require braces and restrictions on movement and weight-bearing [9, 10, 11].
Meniscal trephination appears to be a safe and effective approach for treating degenerative meniscal pathologies. This technique offers the benefit of treating a degenerated or hardened meniscus without hindering functional activities. It also has the advantage of potentially avoiding the long-term negative consequences often associated with meniscectomy, especially in younger patients. However, it is essential to conduct comparative trials to robustly establish the effectiveness of meniscal trephination as a treatment for painful, degenerative, and hard menisci. Additional research is also needed to assess the long-term implications of this technique, particularly concerning pain relief and the overall structural integrity of the knee and meniscus. Such studies would offer a more comprehensive understanding and validation of this innovative approach in the treatment of degenerative meniscal conditions.
Treat degenerated meniscus using arthroscopic meniscal trephination, a novel surgical technique, which avoids the unfavored long-term effects of meniscectomy in young patients.
References
- 1.Kaminski R, Maksymowicz-Wleklik M, Kulinski K, Kozar-Kaminska K, Dabrowska-Thing A, Pomianowski S. Short-term outcomes of percutaneous trephination with a platelet rich plasma intrameniscal injection for the repair of degenerative meniscal lesions. A prospective, randomized, double-blind, parallel-group, placebo-controlled study. Int J Mol Sci 2019;20:856. [Google Scholar]
- 2.Howell R, Kumar NS, Patel N, Tom J. Degenerative meniscus: Pathogenesis, diagnosis, and treatment options. World J Orthop 2014;5:597-602. [Google Scholar]
- 3.Jones JC, Burks R, Owens BD, Sturdivant RX, Svoboda SJ, Cameron KL. Incidence and risk factors associated with meniscal injuries among active-duty US military service members. J Athl Train 2012;47:67-73. [Google Scholar]
- 4.Mohan BR, Gosal HS. Reliability of clinical diagnosis in meniscal tears. Int Orthop 2007;31:57-60. [Google Scholar]
- 5.Mordecai SC, Al-Hadithy N, Ware HE, Gupte CM. Treatment of meniscal tears: An evidence based approach. World J Orthop 2014;5:233-41. [Google Scholar]
- 6.Shelbourne KD, Benner RW, Nixon RA, Gray T. Evaluation of peripheral vertical nondegenerative medial meniscus tears treated with trephination alone at the time of anterior cruciate ligament reconstruction. Arthroscopy 2015;31:2411-6. [Google Scholar]
- 7.Fox JM, Rintz KG, Ferkel RD. Trephination of incomplete meniscal tears. Arthroscopy 1993;9:451-5. [Google Scholar]
- 8.Shelbourne KD, Carr DR. Meniscal repair compared with meniscectomy for bucket-handle medial meniscal tears in anterior cruciate ligament-reconstructed knees. Am J Sports Med 2003;31:718-23. [Google Scholar]
- 9.Kimura M, Shirakura K, Hasegawa A, Kobuna Y, Niijima M. Second look arthroscopy after meniscal repair. Factors affecting the healing rate. Clin Orthop Relat Res 1995;314:185-91. [Google Scholar]
- 10.Morgan CD, Wojtys EM, Casscells CD, Casscells SW. Arthroscopic meniscal repair evaluated by second-look arthroscopy. Am J Sports Med 1991;19:632-7. [Google Scholar]
- 11.Rockborn P, Messner K. Long-term results of meniscus repair and meniscectomy: A 13-year functional and radiographic follow-up study. Knee Surg Sports Traumatol Arthros 2000;8:2-10. [Google Scholar]









