Importance of mastering distal locking of humerus nail by free hand technique and showing its consequences if not done meticulously resulting in loss of daily living years of patient. This article enlights follow up and management of non-union of traumatic humerus shaft fracture with bony defect with implant in-situ.
Dr. Yash N Thakkar, Department of Orthopaedic Surgery, Seth Gordhandas Sunderdas Medical College and King Edward Memorial Hospital, Mumbai, Maharashtra, India. E-mail: thakkaryashn@gmail.com
Introduction: Humerus shaft fractures account for 3% of all adult fractures. Union rate after surgical management is around 84–97% with no difference between compression plating and intramedullary (IM) nailing. Non-union of humeral shaft fracture is not unusual complication of both conservative and operative treatment. IM nailing has been known to have several benefits from its relative stability with minimal soft-tissue dissection but with drawbacks such as less perfect reduction with higher risk of distraction, inability to take down interpositional tissue, risk of radial nerve injury and technical difficulty to pass guide wire and locking of nail. Many methods have been described for nonunion of humeral fracture with good results. However, treatment of a long-standing nonunion of the humerus with bone defect is challenging, as it may be complicated by broken implants. Very less research documented for long standing nonunion of humeral bone with diaphyseal bone defect.
Case Report: We report a case report of middle-aged female who suffered a closed traumatic humeral shaft fracture which was managed with open reduction and fixation with IM nailing with some distraction and distal locking screw missing the nail making it an unstable construct traditionally called Wind shield, wiper effect was noticed in this patient and was the cause of nonunion in this case at some other institute 5 years back lending up in to nonunion with diaphyseal bone defect showing peri-implant expansile benign lesion treated at our institute with implant removal, excision of lytic lesion, and stabilized with extra articular distal humerus locking plate after strut fibular auto bone grafting.
Conclusion: Humerus shaft non-union in a middle-aged patient is heterogeneous entity and has to be managed after ruling out neoplastic (metastasis) as well as infective etiology, and locking plate is the gold standard for its management along with strut grafting being osteoporotic bone with some bony defect.
Keywords: Nonunion, windshield wiper, humerus, peri-implant lytic lesion, disabilities of arm shoulder and hand score.
Humeral shaft nonunion occurs in 3% of all surgically treated fractures [1]. Fixation with unstable construct can lead to macro-motion at the fracture site leading to nonunion. It presents pain and difficulty in the involved upper extremity while performing day-to-day activities. Instability in fracture fixation can also lead to macro-motion at bone-implant interface. Intramedullary (IM) interlock nailing is widely used for the primary fixation of diaphyseal fracture of long bones with good result [1, 2]. A large series of cases has been published in which screw-locking mistakes such as nail and screw failure, loosening of screws, delayed or non-unions were the most common reported complications [3, 4, 5]. Various treatments modalities such as fixation by IM nailing, plating, augmentation plating after nailing, and external fixation [6, 7, 8]. Long-standing humeral shaft nonunion treatment is more challenging as compared to recently diagnosed nonunion as it can present with larger bone defect and implant breakage. We present a case of humerus shaft nonunion operated with 2nd generation IM interlock nailing with unstable construct complicated with peri-implant benign diaphyseal expansile lesion managed with implant removal curettage of lesion and stabilized with extra articular distal humerus locking plate after strut fibular auto bone grafting. The result was evaluated based on disabilities of arm shoulder and hand score (DASH) questionnaire [9].
In the following case report, the patient was 50-year-old female who was referred to our hospital for treatment of left-sided humeral nonunion having difficulties in doing day-to-day activities and decreased range of motion at left shoulder and elbow joint. She had a history of significant trauma 5 years back leading to left humerus shaft fracture with no distal neurovascular deficit and was managed with open antegrade 2nd generation IM interlock humerus nailing 5 years back elsewhere (Fig. 1). Currently patient is disabled with debilitating pain and functional impairment. Shoulder movement is restricted with elbow flexion arc of 0–80°, shoulder abduction 0–45°, and shoulder forward flexion of 0–60° with fracture site mobility in both sagittal and coronal planes (Fig. 2). The DASH was 65. X-ray of left full-length arm with two orthogonal views suggestive of humerus shaft fracture nonunion with peri-implant expansile osteolytic lesion at middle and distal third junction of humerus just at the tip of nail with distal locking screw outside the screw hole of nail leading to an construct as well as there was some distraction at the fracture site which might be the possible cause of nonunion of fracture, other can be infective etiology but it was ruled out as blood parameters were within normal range and there was no wound and suture site were healed (Fig. 1). Blood parameters for infective etiology were within normal limits.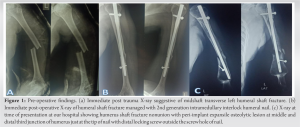
Surgical management
Patient was operated under general anesthesia in the right lateral position as shown in (Fig. 3a). Implant removal done using Deltoid splitting approach over previous incision scar marks. Using posterior approach-Triceps splitting approach dissection carried out and radial and ulnar nerve isolated and protected. Fracture site identified and cystic bony lesion exposed as shown in (Fig. 3b). All the fibrous tissue, pseudo-capsule and sclerotic bone at the fracture site were excised and sent histopathology and culture sensitivity. Posterior cortex of lytic lesion nibbled out and curettage done (Fig. 3c) and sent for . Distal medullary canal opened up using small reamer. 12 cm avascular strut fibular graft harvested from ipsilateral leg (Fig. 3d) and prepared. Fibular graft placed in the medullary canal and fracture site docked and stabilized with 10-hole titanium extraarticular distal humerus locking plate (Fig. 3e). Histopathology report was suggestive off dead necrotic bone tissue with fibrous tissue without any infective cells with some callus tissue in all the samples.
Post-operative rehabilitation protocol
Patient elbow was kept in universal shoulder immobilization till surgical pain subsides following which passive and active assisted range of motion of elbow and shoulder were started. Post-operative course was uneventful. Intraoperative culture was negative for any growth and histopathological report was showing dead cortical bone with fibrous tissue. Patient followed up routinely every monthly. Active range of motion of elbow at 12 months’ post-operative is 0–135° flexion arc and shoulder abduction is 0–170° shoulder forward flexion is 0–170° (Fig. 5) DASH score at 12-month follow-up is 10 (Improved from 65). 12-month follow-up X-ray (Fig. 6) shows absorption and consolidation of bone graft and fracture shows union. There is no local tenderness at fracture site with active range of motion of elbow and shoulder.
Predictably successful fracture healing depends on the development and maintenance of biological and mechanical conditions that favor new bone formation. Traditional concepts of rigid internal fixation seek to control the mechanical environment at and around the fracture site on the basis that excessive interfragmentary motion delays bone healing. However, it has also been shown and proven that controlled micromotion stimulates new bone formation and enhances the healing of long bone fractures [10]. Completely rigid fixation might not therefore always provide the optimal biological environment for healing and subsequent remodeling. Biologic fracture repair focuses on engaging the patient’s innate reparative potential with the goal of accelerating bone healing. However, concerns remain about the potential for fatigue damage, implant failure and improper implantation. Clinical reports highlight the potential significance of fatigue failure mechanisms, particularly with respect to failures of the locking screws or failures at the screw-nail interface of interlock nail [11]. As far as nonunion of humeral bone was concerned traditionally several fixation techniques have been described including IM nailing [5], external fixation [6] and locking compression plating [14]. Nailing if done meticulously can provide stability at the fracture site without jeopardizing soft tissue, but with such kind of long standing nonunion with sclerotic edges and bony lytic lesion, achieving stable fixation can be challenging but. Exchange nailing or nailing in post-implant failure cases is not successful in humeral non-union [4] because of absence of cyclical loading due to weight bearing and higher amount of distractive and torsional loads on the humerus. In addition, IM nailing has been reported to carry higher complication rates including persistent shoulder pain, subacromial impingement, rotator cuff injury, iatrogenic fracture comminution or progression, and higher rates of delayed and non-union. Unreliability of exchange nailing for management of non-union humeral fractures has further been documented by several authors. Although many reports have been documented good outcome with the use of IM nailing and bone grafting for humeral nonunion [15]. Ilizarov external fixation or using limb reconstruction system has shown good outcome [16], but time commitment, complexity of procedures, and non-compliance of the patients make it an unreliable and rather unnecessarily complex option in non-infected non-union. However, it has distinct advantage in case of infected non-union. Biomechanically double plating as compared to single plating has exhibited rigid fixation but fracture nonunion and bony defect being at distal third diaphyseal area one can achieve stability at the fracture site even with single locking anatomical plate [17]. Neural structure should be dissected and protected meticulously especially in cases with non-union because of fibrous tissue around the fracture site. Bone grafting in the form of iliac crest bone graft, fibular strut graft either vascularized or non-vascularized, and autologous or allograft have been described in the management of non-union of humeral shaft fractures post curettage with devoid of posterior cortex. The role of vascularized fibular graft in humeral non-union with bone defect has been described by several authors with successful union rate. However, technically demanding nature of the surgery need for micro-vascular surgical procedure and increased cost of surgery make it an unreliable option in developing countries with less hospital infrastructure. Moreover, it has been associated with risk of thrombosis of vascular pedicle. In elderly people with atherosclerotic disease vascularized fibular graft is contraindicated [18]. The non-vascularized fibular graft is easy to harvest with least possible tissue trauma and least graft site morbidity. The cortical bone gives immediate structural stability at fracture site. It also acts as an internal splint giving stability at fracture site and also increases screw purchase as described by et al [19]. Several authors have shown successful results with the non-vascularized fibular graft. The drawbacks to this technique are possibility of disruption of both endosteal and periosteal blood supply, iatrogenic fracture during insertion of graft and possible nerve palsy while harvesting [20, 21]. With the use of above research studies, we planned for using autologous non-vascularized IM fibular strut graft for cortical support and stabilized with single extraarticular distal humerus anatomical plate. Over the period of time, patient elbow and shoulder range were drastically improved and bone graft shows consolidation with fracture getting united.
We present you a case report to describe uncommon radiographic findings related to the use of interlocking nails fixation with unstable fixation – Radiolucency located around the distal tip of the nail observed in our case. This radiographic sign was similar to one described as “windshield-wiper effect” and observed around the tip of the screw used for slipped capital femoral epiphysis in children, and also in association with IM nail treatment. This effect is also observed in animal bones post fracture fixation with interlock nailing. Windshield-wiper effect in bone develops as a result of toggling of implant inside the bone in unstable fixation resulting in formation of osteolytic lesion around the tip of it. Our report shows that revision locking plating with autologous non-vascularized fibular graft acting as osteoconductive as well as osteoinductive, is a reliable option in humeral diaphyseal non-unions with failed osteosynthesis with relative stability and significant cortical defect to achieve adequate screw purchase, stability at fracture site and high chance of union following good functional outcome.
Humerus shaft fracture being a common fracture if not being managed appropriately can lead to catastrophic complications, one of such complication Non-union resulting in to peri- implant lytic lesion s/o windshield wiper effect which was also seen in animal bone fracture. To prevent windshield wiper effect and non-union mastering the insertion of free hand distal interlocking screw is mandatory. It is appropriate management in osteoporotic bone after 5 years of index surgery is Enlightened in this article.
References
- 1.Rommens PM, Kuechle R, Bord T, Lewens T, Engelmann R, Blum J. Humeral nailing revisited. Injury 2008;39:1319-28. [Google Scholar]
- 2.Li XK, Wang HQ, Wei YY, Wu ZX. Treatment of nonunions of humeral fractures with interlocking intramedullary nailing. Chin J Traumatol 2008;11:335-40. [Google Scholar]
- 3.McKee MD, Miranda MA, Riemer BL, Blasier RB, Redmond BJ, Sims SH, et al. Management of humeral nonunion after the failure of locking intramedullary nails. J Orthop Trauma 1996;10:492-9. [Google Scholar]
- 4.Flinkkilä T, Ristiniemi J, Hämäläinen M. Nonunion after intramedullary nailing of humeral shaft fractures. J Trauma 2001;50:540-4. [Google Scholar]
- 5.Farragos AF, Schemitsch EH, McKee MD. Complications of intramedullary nailing for fractures of the humeral shaft: A review. J Orthop Trauma 1999;13:258-67. [Google Scholar]
- 6.Lavini F, Brivio LR, Pizzoli A, Giotakis N, Bartolozzi P. Treatment of non-union of the humerus using the Orthofix external fixator. Injury 2001;32 Suppl 4:SD35-40. [Google Scholar]
- 7.Allende C, Vanoli F, Gentile L, Gutierrez N. Minimally invasive plate osteosynthesis in humerus nonunion after intramedullary nailing. Int Orthop 2018;42:2685-9. [Google Scholar]
- 8.Zhao JG, Wang J, Wang C, Kan SL. Intramedullary nail versus plate fixation for humeral shaft fractures: A systematic review of overlapping meta-analyses. Medicine (Baltimore) 2015;94:e599 [Google Scholar]
- 9.De Smet L. The DASH questionnaire and score in the evaluation of hand and wrist disorders. Acta Orthop Belg 2008;74:575-81. [Google Scholar]
- 10.Goodship AE, Kenwright J. The influence of induced micromovement upon the healing of experimental tibial fractures. J Bone Joint Surg Br 1985;67:650-5. [Google Scholar]
- 11.Durall I, Diaz-Bertrana MC, Puchol JL, Franch J. Radiographic findings related to interlocking nailing: Windshield-wiper effect and locking screw failure. Vet Comp Orthop Traumatol 2003;16:217-22. [Google Scholar]
- 12.Maletis GB, Bassett GS. Windshield-wiper loosening: A complication of in situ screw fixation of slipped capital femoral epiphysis. J Pediatr Orthop 1993;13:607-9. [Google Scholar]
- 13.Pastor T, Pastor T, Kastner P, Souleiman F, Knobe M, Gueorguiev B, et al. Validity of a novel digitally enhanced skills training station for freehand distal interlocking. Medicina (Kaunas) 2022;58:773. [Google Scholar]
- 14.Kumar MN, Ravindranath VP, Ravishankar M. Outcome of locking compression plates in humeral shaft nonunions. Indian J Orthop 2013;47:150-5. [Google Scholar]
- 15.De Carolis O, Mori CM, Vicenti G, Carrozzo M, Abate A, Caiaffa V. A lifelong story: Case report of a humeral shaft nonunion successfully treated after 30 years. Injury 2018;49 Suppl 4:S43-7. [Google Scholar]
- 16.Patel VR, Menon DK, Pool RD, Simonis RB. Nonunion of the humerus after failure of surgical treatment. Management using the Ilizarov circular fixator. J Bone Joint Surg Br 2000;82:977-83. [Google Scholar]
- 17.Meloy GM, Mormino MA, Siska PA, Tarkin IS. A paradigm shift in the surgical reconstruction of extra-articular distal humeral fractures: Single-column plating. Injury 2013;44:1620-4. [Google Scholar]
- 18.Kerfant N, Valenti P, Kilinc AS, Falcone MO. Free vascularised fibular graft in multi-operated patients for an aseptic non-union of the humerus with segmental defect: Surgical technique and results. Orthop Traumatol Surg Res 2012;98:603-7. [Google Scholar]
- 19.Wright TW, Miller GJ, Vander Griend RA, Wheeler DO, Dell PC. Reconstruction of the humerus with an intramedullary fibular graft. A clinical and biomechanical study. The Journal of Bone and Joint Surgery. British volume. 1993 Sep;75(5):804-7. [Google Scholar]
- 20.Kashayi-Chowdojirao S, Vallurupalli A, Chilakamarri VK, Patnala C, Chodavarapu LM, Kancherla NR, et al. Role of autologous non-vascularised intramedullary fibular strut graft in humeral shaft nonunions following failed plating. J Clin Orthop Trauma 2017;8:S21-30. [Google Scholar]
- 21.Shetty K, Cheppalli N, Kaki D. Autologous nonvascularized fibula graft and locking compression plating for failed fixation of humeral shaft with atrophic gap nonunion. Cureus 2022;14:e24293. [Google Scholar]










