The importance of early intervention in patients who present with persistent symptoms – of unknown etiology – after primary total knee arthroplasty.
Dr. Naem A Mufarreh, Department of Orthopedic Surgery, Kettering Health-Grandview, Dayton, Ohio, United States. E-mail: mufarreh.med@gmail.com
Introduction: Oxidized Zirconium (OXINIUM™) is a metal alloy with a ceramic surface, utilized to increase the longevity of knee and hip implantations and reduce polyethylene wear. Polyethylene-based spacers are effective in infection control and prosthetic stability. Therefore, understanding the interactions between the polyethylene spacer and metallic counterparts is essential in surgical decision-making. Furthermore, understanding how patients may present when catastrophic failure of these components arises is imperative. Herein, we present a unique case of atraumatic OXINIUM™ wear in a middle-aged female after uneventful primary total knee arthroplasty (TKA), highlighting atypical clinical features and addressing the surgical management of this unexpected implant failure.
Case Report: A 51-year-old African American female presented from an outside facility with persistent left knee pain after undergoing a TKA with a Smith and Nephew OXINIUM™ coated knee. The patient presented to the senior author’s clinic with worsening symptoms 2-year postoperatively from her primary left TKA by another surgeon. After a thorough work-up which was essentially unremarkable–3 years from her initial surgery – the recommendation was made for surgical revision given clinical concern for instability. During the initial surgical approach, significant sparking of the tissue was noted on the use of electrocautery. Once the capsule was dissected, black synovial fluid with soft tissue involvement was noted. Intraoperative analysis of the polyethylene spacer revealed disintegration in the medial compartment with loss of the zirconium coating along the femoral component. There was no evidence of polyethylene spacer wear within the lateral compartment. The primary components were explanted and replaced with a nickel-free implant. Following revision, the patient reported complete resolution of her symptoms with improvement in active range of motion.
Conclusion: This case illustrates a unique presentation of atraumatic prosthetic surface coating failure after an uneventful primary TKA with well-aligned post-operative radiographs. Instability in the posterior stabilized total knee caused the polyethylene liner to come out of place, causing articulation of femoral and tibial components, creating the metal debris. Patients who present with persistent symptoms–of unknown etiology – after primary TKA should be considered for enhanced screenings and early surgical intervention.
Keywords: OXINIUM™, total knee arthroplasty, metallosis, prosthetic failure.
Innovations in total joint arthroplasty have aimed to reduce frictional wear while extending implant lifespan. This has led to the development of several new joint materials in an effort to move past traditional ones such as cobalt and ceramic, which have had significant adverse events such as metallosis and high failure rates [1,2,3]. Total knee arthroplasty (TKA) is a common and consistently successful procedure that provides reliable outcomes for patients generally suffering from osteoarthritis, fracture, dysplasia, malignancy, etc. Patients tend to experience alleviation of pain, restoration of function, and an overall improvement in their quality of life. Multiple categories of TKA prosthetic designs have different indications and numerous complications that can present in a patient post-operatively. General complications that can arise consist of periprosthetic fracture, aseptic loosening, wound complications, periprosthetic joint infections, and metallosis, as well as many others [4]. Often, these complications arise due to trauma, which can be assessed on imaging, or these patients can present with dermatologic or abnormal laboratory findings. In this case report; however, the patient had no underlying abnormalities suggesting hardware failure other than experiencing pain. This led to the decision to undergo a total knee revision in which metallosis was discovered. Metallosis, although uncommon, is a well-understood complication following total arthroplasties of high-wear joints. Clinical manifestations include pain, swelling, dislocation, and instability. When considering the differential diagnosis, metallosis commonly presents distinctly on radiological imaging [5]. These findings include a curvilinear radiodensity (bubble sign), a cloudy density within soft tissue (cloud sign), and increased linear density surrounding a portion of the joint capsule (metal-line sign) [6]. Metallosis is routinely treated with a synovectomy and standard two-stage revision arthroplasty. The failure rate of revision surgery is attributed to the need for early intervention, as prevention of joint destruction is vital for successful revisions. Prevention of metallosis has led to the development of newer alternative materials for improved patient outcomes. Oxidized zirconium (OXINIUM™) based joint replacements have become more popular than their cobalt predecessors in recent years due to their biomechanical properties; specifically, their low friction coefficient, lighter weight, and reduced wearing of the polyethylene spacer [7]. Smith and Nephew, the creators of OXINIUM™ joint replacement report that it has a surface hardness and lifetime duration that is 2 times stronger than original cobalt-chrome or ceramic predecessors [8]. Interestingly, unlike its predecessors, OXINIUM™ itself is highly flammable; however, the processing method to coat joint replacements allegedly reduces the flammability to a negligible amount [2, 9]. Despite these advances, there appears to be an annual increase in the number of cases involving catastrophic failure of the implant with wearing of the OXINIUM™ components. Although the coating may be stronger than its predecessors. OXINIUM™ coating failure may lead to the exposure of soft zirconium alloy. This ultimately results in periprosthetic soft tissue, synovial, and bone infiltration by the metallic debris which contributes to prosthetic joint failure as well as metallosis of the surrounding tissue, secondary to coating failure [6, 10]. There is limited literature on the effects of OXINIUM™ after TKA and only a few cases have been reported in total hip arthroplasty, which tend to be associated with trauma. Thus, we present a case of atraumatic OXINIUM™ wear after TKA.
A 51-year-old patient presented to the senior author’s (SB) Orthopaedic clinic with persistent left knee pain. On presentation, the patient was 286 lbs at 5’ 2” with a body mass index (BMI) of 52.3. The patient underwent a Smith and Nephew left OXINIUM™ coated TKA at an outside hospital (OSH) in 2016. At the 6-month follow-up at the OSH the patient was informed that there was some slight tilting of the prosthesis; however, there were no complaints of pain until 2018–2 years after the index procedure. Her symptoms continued to worsen in 2018 and began impacting her activities of daily living. The patient underwent extensive testing for aseptic loosening, infection, and metallosis over the course of a year which was essentially unremarkable. At this point, the patient was 3 years from her primary procedure and the recommendation was made for surgical exploration/revision by the original surgeon. At this point, she presented to the senior author’s orthopedic clinic for a second opinion. During evaluation, the patient exhibited an active range of motion 0–100° with increased anterior-posterior translocation. Metal-on-metal grinding was noted at approximately 90° during provocative testing. Imaging obtained during her evaluation confirmed this suspicion with a cloud sign noted on plain radiographs (Fig. 1).
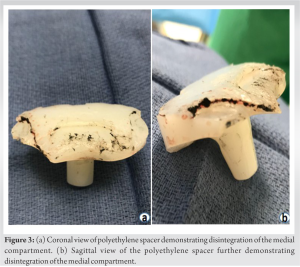

We find this to be a unique patient presentation of zirconium coating failure in both the medial and lateral compartments with isolated medial polyethylene wear and without a correlated cause such as component loosening. While there are documented cases of catastrophic prosthetic failures secondary to trauma such as dislocation, this patient’s history is unremarkable. Furthermore, her atypical presentation, of insidious onset of pain and inability to perform activities of daily living–without a history of trauma, loosening, or infection–2 years after her index procedure was perplexing. While there was an audible click on the physical examination – radiographic imaging was remarkable for what appeared to be heterotopic bone formation along the lateral aspect of the femur. Laboratory testing for heavy metals as well as infectious etiologies for her complaints was unremarkable. It was later made evident that what we believed to be heterotopic bone was actual metal impregnated within the capsular and surrounding tissues which radiologic literature refers to as a “cloud sign” [1]. This is significant as we have yet to identify a case that informed readers about the dangers of the use of electrocautery during revision arthroplasty, even if the suspicion for metallosis is low. Thus, we recommend sharp dissection through a capsule to explore the soft tissues before using the electrocautery to avoid a potential fire risk. Moreover, Zirconium from implant wear appears to be flammable, despite the manufacturer’s reports of stability once processed onto an implant. Aside from the safety implications, it is important to reflect upon the biomechanical principles specifically that of isolated medial compartment wear. Literature review of this topic is also limited given the isolated nature of the polyethylene wearing without traditional signs or symptoms of loosening/trauma. Ultimately, we could not identify any literature that discussed femoral component wear of both the lateral and medial compartments secondary to isolated wearing of the medical polyethylene component. This led us to speculate that there was an issue with the polyethylene component as it had disassociated from the tibial locking mechanism and caused the femoral and tibial components to articulate in a metal-on-metal manner – resulting in zirconium debris throughout the synovium, bone, and surrounding soft tissues. While it is worth noting that the original surgeon was concerned about the position of the tibial component, it does not appear to be the main cause of the prosthetic failure as both the tibial and femoral components were stable on intraoperative examination during revision surgery. Thus, the novelty in this case lies in the patient’s presentation. While her symptomatology was consistent with prosthetic failure, there was no apparent cause that we identified that can account for our intraoperative examination of the primary components. She denied any history of trauma, she was not overly active, nor did she have a strenuous job that required a significant amount of walking or standing. While her BMI could be a contributing factor, this in and of itself, is not enough in our opinion to result in unicompartmental wear. However, we do believe that her wound dehiscence after revision arthroplasty was directly correlated to BMI [11]. It is also important to mention possible confounding variables aside from BMI such as the positioning of the original TKA implants and the integrity of the prosthesis itself – which may be to blame for the resultant implant failure. Therefore, it is the opinion of the senior surgeon that the catastrophic failure of this implant –resulting in the direct articulation of the metallic femoral and tibial components – which allowed zirconium debris to be released into the synovium, bone, and surrounding soft tissues is secondary to a failure of the tibial locking mechanism. This theory is based upon the isolated wearing of the medial polyethylene component which cannot be correlated to intraoperative findings of both medial and lateral compartments as previously noted.
This case highlights the importance of enhanced screenings and early surgical intervention in patients who present with persistent symptoms – of unknown etiology – after primary TKA. In addition, it illustrates the importance of sharp dissection in revision arthroplasty, even if the suspicion of metallosis is low, as the sparks from the electrocautery demonstrate a significant fire risk.
This case report highlights a relatively uncommon presentation of a TKA failure that used an OXINIUM-coated knee prosthetic in which metallosis was noted upon revision. The lack of typical presenting symptoms should warrant enhanced screenings and early surgical intervention in future, similar cases. Relieving such symptoms through revision surgery is imperative in improving patient outcomes and enhancing standard of living.
References
- 1.Romesburg JW, Wasserman PL, Schoppe CH. Metallosis and metal-induced synovitis following total knee arthroplasty: Review of radiographic and CT findings. J Radiol Case Rep 2010;4:7-17. [Google Scholar]
- 2.Lützner J, Dinnebier G, Hartmann A, Günther KP, Kirschner S. Study rationale and protocol: Prospective randomized comparison of metal ion concentrations in the patient’s plasma after implantation of coated and uncoated total knee prostheses. BMC Musculoskelet Disord 2009;10:128. [Google Scholar]
- 3.Galetz MC, Fleischmann EW, Konrad CH, Schuetz A, Glatzel U. Abrasion resistance of oxidized zirconium in comparison with CoCrMo and titanium nitride coatings for artificial knee joints. J Biomed Mater Res B Appl Biomater 2010;93:244-51. [Google Scholar]
- 4.Varacallo M, Luo TD, Johanson NA. Total knee arthroplasty techniques. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499896/?report=classic [Last accessed on 2022 May 01]. [Google Scholar]
- 5.Frye BM, Laughery KR, Klein AE. The oxinium arthrogram: A sign of oxidized zirconium implant failure. Arthroplast Today 2021;8:103-9. [Google Scholar]
- 6.Vivegananthan B, Shah R, Karuppiah AS, Karuppiah SV. Metallosis in a total knee arthroplasty. BMJ Case Rep 2014;2014:bcr2013202801. [Google Scholar]
- 7.Chang Y, Lee MS, Liau JJ, Liu YL, Chen WC, Ueng SW. Polyethylene-based knee spacer for infection control: Design concept and pre-clinical in vitro validations. Polymers (Basel) 2020;12:2334. [Google Scholar]
- 8.Jonsson BA, Kadar T, Havelin LI, Haugan K, Espehaug B, Indrekvam K, et al. Oxinium modular femoral heads do not reduce polyethylene wear in cemented total hip arthroplasty at five years: A randomised trial of 120 hips using radiostereometric analysis. Bone Joint J 2015;97-B:1463-9. [Google Scholar]
- 9.Tribe H, Malek S, Stammers J, Ranawat V, Skinner JA. Advanced wear of an Oxinium™ femoral head implant following polyethylene liner dislocation. Ann R Coll Surg Engl 2013;95:e133-5. [Google Scholar]
- 10.Sharareh B, Phan DL, Goreal W, Schwarzkopf R. Metallosis presenting as knee pain 26 years after primary total knee arthroplasty. J Orthop Case Rep 2015;5:62-5. [Google Scholar]
- 11.Wilson JA, Clark JJ. Obesity: Impediment to postsurgical wound healing. Adv Skin Wound Care 2004;17:426-35. [Google Scholar]










