Understanding the different types of disc pathologies is important in deciding treatment options for the patient. A retained disc is the one left at the adjacent level during the index surgery as part of watchful neglect by the surgeon; recurrence is reherniation at the same level as primary discectomy , and residual disc is the remaining disc material after the primary discectomy.
Dr. Shailesh Hadgaonkar, Spine and Neuroscience Unit, Sancheti Hospital, Pune, Maharashtra, India. E-mail: drshadgaonkar@gmail.com
Discectomy is a standard surgery for disc herniation performed by senior, experienced as well as young trainee spine surgeons. Yet, they both have patients returning with radicular pain. Sometimes, it is attributed to insufficient decompression in the primary surgery, sometimes to re-herniation at the same level, and sometimes thought as new disc herniation at a different level. The primary surgery is often blamed for the recurrence of the pain, without an assessment of the clinical condition of the patient. Surgeons use the terms recurrent, residual, and retained disc interchangeably as per their convenience without understanding the actual disc pathology. This causes errors in further treatment and dissatisfaction in patients. In this short review, we intend to clear the baffling terminologies pertaining to discectomy and help the readers to identify the exact nodus of the patient’s plight. The optimal extent of disc excision for a satisfactory outcome is not strictly defined [1]. Two main types of discectomy are subtotal discectomy, in which the annulus is opened and all accessible disc material is removed by curettage of the endplate; and limited discectomy, in which only the loose fragments are removed [1]. Patients who undergo subtotal discectomy experience progressive degeneration and back pain at the operated level compared with patients who undergo limited discectomy, which may eventually require spinal fusion at that level [2, 3] The problem with limited discectomy, on the other hand, is the higher recurrence rate due to the remaining disc material herniating later [2]. The surgical method may also have a bearing on the results. Open discectomy is based on direct visualization of decompression of the nerve root, whereas newer techniques such as microscopic and percutaneous endoscopic discectomy use indirect methods to confirm the adequacy of decompression, such as checking the free mobility of the traversing nerve root, the free mobility of the probe in the epidural space, and the removal of loose fragments which were identified on pre-operative magnetic resonance imaging (MRI) [1]. Percutaneous endoscopic discectomy allows for smaller incisions, less soft-tissue trauma, and faster recovery, resulting in greater relief of back pain and allowing an earlier return to work [4]. However, studies have shown that up to 2.8–15% of patients treated with limited discectomy using percutaneous endoscopic disc removal had residual disc material on immediate post-operative MRI examination [5]. Therefore, these techniques are subjective and dependent on the surgeon’s experience and skill and may result in inadequate decompression. Post-operatively, these patients may not experience the expected pain relief and continue to have radicular symptoms. In some patients, pain may be relieved for a short period of time, after which the same symptoms may recur, either due to re-herniation at the same level or at adjacent levels. Hence, it is very important to know the types of inefficiencies in disc removal, namely recurrence, retained, residual, and relapsed disc. Distinguishing the causes of pain after surgery can help surgeons do better pre-operative planning and make better intraoperative decisions, thereby helping them to choose a clear endpoint for decompression. This can also help patients by preventing the need for reoperation and achieving better functional outcomes after surgery.
Recurrent Disc
A disc recurrence is defined as a re-herniation of disc material at the previously operated level with the recurrence of similar pain after a period of relief of minimum 6 months and MRI confirmation, which may occur on the same or contralateral side (Fig. 1) [6-9]. In up to 5–15% patients, disc herniation can recur [10]. However, if stricter definition of recurrence is used, with cases restricted to recurrence at the same level and side as previous operation, the recurrence rate was found to be 2–5%. [9, 10] Risk factors for recurrence of a lumbar disc prolapse include disc degeneration, modic changes in the endplate, trauma to back, advanced age, and smoking [11] Radiological features such as increased disc height, lumbosacral transitional vertebrae, and segmental instability may also predict recurrence [4, 12]. It has been suggested that contralateral nucleus pulposus herniation may occur if the annulus on the opposite side is damaged during primary discectomy and only limited fragments are removed. In the case of a recurrent disc herniation on the opposite side, removal of the opposite annulus and disc material may damage the posterior longitudinal ligament and affect lumbar biomechanics and spinal stability. The average time between primary surgery and recurrent disc herniation symptoms was reported to be 17 ± 21 months by Eun et al. [4]. Surgical management of recurrence is debatable due to a need for high-level evidence [8]. Repeat discectomy remains the main procedure for it, with only minimal improvement often reported in the patient’s clinical condition as compared to the primary surgery [13]. There also remains risk of further instability. Therefore, many authors advocate the use of instrumented spinal fusion with repeat discectomy, despite the absence of instability at the time of recurrence [14].
Residual Disc
A residual disc is defined as the disc material that remains at the symptomatic operated level after the extruded fragment has been removed and enough decompression has been achieved (Fig. 2). 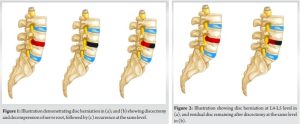
The residual disc material may cause painful radicular symptoms to persist post-operatively, with patients complaining of inadequate relief. Such patients require re-operation. Discectomy usually involves removal of only the herniated disc material and decompression of the nerve roots, leaving the remaining disc in situ. However, this may cause more disc material to come out and recompress or inflame the nerve roots [15]. To deal with this, Aoyama et al. used intraoperative ultrasound to differentiate between nerve roots and disc material in 30 patients. By this method, they were able to confirm the adequacy of decompression in all 30 patients and also identified residual disc material in 2 patients which they were able to remove satisfactorily [15]. However, it was found to be more useful for patients with a large surgical field undergoing procedures such as removal of spinal tumors or arachnoid cysts to check the remaining fragments [16]. In 2.8–15% of patients undergoing percutaneous endoscopic lumbar discectomy (PELD), residual disc fragments were observed on immediate post-operative MRI [5]. Although the presence of a residual disc fragment with persistent compression is a reason for reoperation, not all residual disc fragments observed on immediate post-operative MRI are symptomatic (i.e., they are clinically silent). Only 1.3% of patients with residual disc tissue had to go for repeat discectomy [17]. In a retrospective study by Baek et al., the long-term clinical outcomes of PELD patients in whom complete disc fragment removal was achieved (complete group) were compared with those in whom residual fragments were detected on post-operative MRI (residual group). Early reoperation (within the first 3 post-operative months) was performed in 3 patients in the residual group (7.9%) and 4 patients in the complete group (2.1%). They concluded that in patients with asymptomatic disc remnants, “watchful waiting” can be performed instead of immediate re-exploration [17]. Careful examination of post-operative MRI findings (within 24 h of surgery) revealed that some of the disc-like material was actually edematous tissue due to the fluid used during surgery. Therefore, analysis of T1-weighted MRI images is preferable, before taking up the patient for an unnecessary repeat surgery [18].
Retained Disc
Retained disc is the one at same level where only nerve root decompression or deroofing was considered assuming that it should give symptomatic relief. Also retained disc can be dealing with two level discs where only one level disc is removed or decompressed and the other disc is kept as it assuming it will not create symptoms. (Fig. 3)
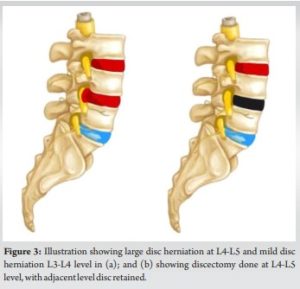 In both the above mentioned scenarios, the discs which were untreated/ retained creates symptoms after a while because of worsening of disc or extrusion. Though this was thought to be uncommon, this entity is seen at many instances which is the Retained disc variation. Therefore, supervised neglect of the retained disc carries its risks. Careful clinical examination is important to differentiate retained disc from recurrence.
In both the above mentioned scenarios, the discs which were untreated/ retained creates symptoms after a while because of worsening of disc or extrusion. Though this was thought to be uncommon, this entity is seen at many instances which is the Retained disc variation. Therefore, supervised neglect of the retained disc carries its risks. Careful clinical examination is important to differentiate retained disc from recurrence.
.
Clinical examination of the patient plays a crucial role in identifying the level of radiculopathy. Dermatomal pain in the same region after discectomy often indicates recurrence, whereas pain in an adjacent or new dermatomal distribution could be due to the retained disc. MRI findings help to confirm the pathological level and differentiate between a recurrent and retained disc. Understanding the different types of disc re-herniations is important in deciding treatment options such as physiotherapy, nerve root block, and surgical modalities.
References
- 1.Heo JH, Kim CH, Chung CK, Choi Y, Seo YG, Kim DH, et al. Quantity of disc removal and radiological outcomes of percutaneous endoscopic lumbar discectomy. Pain Physician 2017;20:E737-46. [Google Scholar]
- 2.McGirt MJ, Ambrossi GL, Datoo G, Sciubba DM, Witham TF, Wolinsky JP, et al. Recurrent disc herniation and long-term back pain after primary lumbar discectomy: Review of outcomes reported for limited versus aggressive disc removal. Neurosurgery 2009;64:338-44; discussion 344-5. [Google Scholar]
- 3.Carragee EJ, Han MY, Suen PW, Kim D. Clinical outcomes after lumbar discectomy for sciatica: The effects of fragment type and anular competence. J Bone Joint Surg Am 2003;85:102-8. [Google Scholar]
- 4.Eun SS, Lee SH, Sabal LA. Long-term follow-up results of percutaneous endoscopic lumbar discectomy. Pain Physician 2016;19:E1161-6. [Google Scholar]
- 5.Choi KC, Lee JH, Kim JS, Sabal LA, Lee S, Kim H, et al. Unsuccessful percutaneous endoscopic lumbar discectomy: A single-center experience of 10,228 cases. Neurosurgery 2015;76:372-80; discussion 380-1; quiz 381. [Google Scholar]
- 6.Hao L, Li S, Liu J, Shan Z, Fan S, Zhao F. Recurrent disc herniation following percutaneous endoscopic lumbar discectomy preferentially occurs when Modic changes are present. J Orthop Surg Res 2020;15:176. [Google Scholar]
- 7.Guo J, Li G, Ji X, Wu X, Zhang G, Zhou C, et al. Clinical and radiological risk factors of early recurrent lumbar disc herniation at six months or less: A clinical retrospective analysis in one medical center. Pain Physician 2022;25:E1039-45. [Google Scholar]
- 8.Dower A, Chatterji R, Swart A, Winder MJ. Surgical management of recurrent lumbar disc herniation and the role of fusion. J Clin Neurosci 2016;23:44-50. [Google Scholar]
- 9.Acharya KN, Nathan TS, Kumar JR, Menon KV. Primary and revision lumbar discectomy: A three-year review from one center. Indian J Orthop 2008;42:178-81. [Google Scholar]
- 10.Swartz KR, Trost GR. Recurrent lumbar disc herniation. Neurosurg Focus 2003;15:E10. [Google Scholar]
- 11.Kim JM, Lee SH, Ahn Y, Yoon DH, Lee CD, Lim ST. Recurrence after successful percutaneous endoscopic lumbar discectomy. Minim Invasive Neurosurg 2007;50:82-5. [Google Scholar]
- 12.Axelsson P, Karlsson BS. Intervertebral mobility in the progressive degenerative process. A radiostereometric analysis. Eur Spine J 2004;13:567-72. [Google Scholar]
- 13.Palma L, Carangelo B, Muzii VF, Mariottini A, Zalaffi A, Capitani S. Microsurgery for recurrent lumbar disk herniation at the same level and side: Do patients fare worse? Experience with 95 consecutive cases. Surg Neurol 2008;70:619-21; discussion 621. [Google Scholar]
- 14.El Shazly AA, El Wardany MA, Morsi AM. Recurrent lumbar disc herniation: A prospective comparative study of three surgical management procedures. Asian J Neurosurg 2013;8:139-46. [Google Scholar]
- 15.Aoyama T, Hida K, Akino M, Yano S, Iwasaki Y. Detection of residual disc hernia material and confirmation of nerve root decompression at lumbar disc herniation surgery by intraoperative ultrasound. Ultrasound Med Biol 2009;35:920-7. [Google Scholar]
- 16.Bonsanto MM, Metzner R, Aschoff A, Tronnier V, Kunze S, Wirtz CR. 3D ultrasound navigation in syrinx surgery-a feasibility study. Acta Neurochir (Wien) 2005;147:533-40; discussion 540-1. [Google Scholar]
- 17.Baek J, Yang SH, Kim CH, Chung CK, Choi Y, Heo JH, et al. Postoperative longitudinal outcomes in patients with residual disc fragments after percutaneous endoscopic lumbar discectomy. Pain Physician 2018;21:E457-66. [Google Scholar]
- 18.Yang JS, Liu KX, Fan H. Re: Baek et al postoperative longitudinal outcomes in patients with residual disc fragments after percutaneous endoscopic lumbar discectomy. Pain Physician 2019;22:E238-40. [Google Scholar]






