Bilateral medial Hoffa fractures are rare injuries concerning the orthopaedic trauma field and this is the first case described, that was treated operatively with good functional outcome.
Dr. Evangelia Argyropoulou, Department of Orthopedics, General University Hospital of Patras, Patras 26504, Greece. E-mail: eva.argirop@gmail.com
Introduction: Intra-articular distal femoral fractures in the coronal plane, widely described as Hoffa fractures, are a rare entity. Lateral femoral condyles are mostly affected, while diagnosis can be challenging. Bilateral medial femoral condyle fractures are exceedingly scarce, with only one case being published in recent literature.
Case Report: We present a case of a white 65-year-old man with bilateral medial femoral condyle Hoffa fractures caused by a crush injury. The patient was treated operatively by two different teams operating simultaneously on both sides, with good clinical and radiological outcomes after a follow-up period of 3 months.
Conclusion: A literature review was conducted to analyze the potential mechanism of injury, diagnostic methods, and therapeutic approach. Bilateral medial Hoffa fractures are rare injuries concerning the orthopedic trauma field and this is the first case described, that was treated operatively with good functional outcomes.
Keywords: Hoffa fractures, distal femur fractures, bilateral medial condyles, trauma.
Friedrich Busch in 1869 was the first to describe this fracture pattern, followed by Albert Hoffa in 1904 [1]. Intra-articular distal femoral fractures in the coronal plane are rare, with an occurrence of 0.65% among all femoral fractures and 8.7–13% among distal femoral fractures [2]. Low-energy trauma can lead to Hoffa fractures in children and elderly patients with osteoporotic bone, while in some cases, the cause can be iatrogenic [3]. Lateral condylar fractures are the most frequent among all Hoffa fractures, with an incidence of 78–85%, followed by bilateral condylar fractures and medial condylar fractures. Hoffa fractures are classified as 33B3 according to the AO/OTA classification system [4]. A CT classification system is also used to categorize Hoffa fractures. After a meticulous search of the literature, our report is the second reported case and the first surgically treated case of bilateral medial femoral condyle Hoffa fractures in a 65-year-old man after a motor vehicle accident.
A 65-year-old man was transferred to the Emergency department of our hospital after a motorbike accident. He was a non-smoker, with no medical comorbidities. He was initially managed according to the ATLS guidelines. His vital signs were normal, while he was complaining about bilateral knee pain. A second-degree, partial-thickness burn on the ipsilateral knee was identified. Clinical evaluation revealed a limited, painful range of motion and edema on both patient’s knees. The radiological examination revealed bilateral Hoffa fractures of the medial femoral condyles and an undisplaced medial tibial plateau fracture of his right knee (Fig. 1 and 2).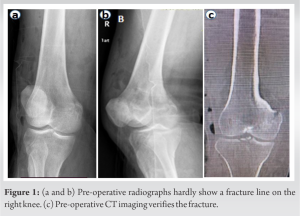 A CT scan was performed for better visualization of the fractures and pre-operative planning. Based on the condition of the soft-tissue envelope, no early surgical intervention was considered.
A CT scan was performed for better visualization of the fractures and pre-operative planning. Based on the condition of the soft-tissue envelope, no early surgical intervention was considered. Ten days after his admission, he was transferred to the operating room. The patient was placed in supine position with bilateral tourniquets applied. Both knees were flexed at 20–30° and hips slightly externally rotated (Fig. 3).
Ten days after his admission, he was transferred to the operating room. The patient was placed in supine position with bilateral tourniquets applied. Both knees were flexed at 20–30° and hips slightly externally rotated (Fig. 3). Two different teams were operating simultaneously on both sides, and a classic medial approach to the distal femur was utilized. Under direct visualization, both fractures were reduced and stabilized using three 3.5 mm countersunk lag screws on each side to prevent rotational instability. A 3.5 mm partially threaded screw was placed though the same incision to stabilize the tibial plateau fracture of the patient’s right knee. Free range of motion was confirmed intraoperatively, while fluoroscopic images were obtained (Fig. 4). Passive range of motion exercises began the 1st post-operative day, and the patient was discharged 4 days postoperatively. At 1-month follow-up, free range of motion was identified bilaterally. A split-thickness skin graft (STSG) from the contralateral thigh was obtained to cover the skin loss on patient’s right knee (Fig. 5).
Two different teams were operating simultaneously on both sides, and a classic medial approach to the distal femur was utilized. Under direct visualization, both fractures were reduced and stabilized using three 3.5 mm countersunk lag screws on each side to prevent rotational instability. A 3.5 mm partially threaded screw was placed though the same incision to stabilize the tibial plateau fracture of the patient’s right knee. Free range of motion was confirmed intraoperatively, while fluoroscopic images were obtained (Fig. 4). Passive range of motion exercises began the 1st post-operative day, and the patient was discharged 4 days postoperatively. At 1-month follow-up, free range of motion was identified bilaterally. A split-thickness skin graft (STSG) from the contralateral thigh was obtained to cover the skin loss on patient’s right knee (Fig. 5). At 2-month follow-up, partial weight bearing was started, while skin graft integration was observed. Finally, at 3-month follow-up, the patient was able to walk without any assistance, an unrestricted range of motion was obtained, skin graft was fully integrated, and the patient was able to return at his pre-injury level of activity.
At 2-month follow-up, partial weight bearing was started, while skin graft integration was observed. Finally, at 3-month follow-up, the patient was able to walk without any assistance, an unrestricted range of motion was obtained, skin graft was fully integrated, and the patient was able to return at his pre-injury level of activity.
Motor vehicle collisions are mostly associated with Hoffa injuries due to the flexed knee position of the driver. The application of force on the posterior femoral condyle, in the vertical plane, corresponding to varying degrees of a flexed knee has been suggested as a potential mechanism of injury [5]. Diagnosis of Hoffa fractures can be demanding. Trauma history, physical examination, and imaging, along with a high index of suspicion, can be useful diagnostic tools. However, missed diagnosis renders among 30% of all cases, since fracture lines often overlap the lateral femoral condyle [2, 4]. Oblique views should be used routinely since they can reveal undisplaced Hoffa fractures more efficiently compared to anteroposterior and lateral views. CT scan is considered the gold standard in the diagnosis of Hoffa fractures, while MRI should be performed if ligamentous injury is suspected [6]. Koné et al. were the first to describe a case of bilateral medial condyle Hoffa fracture to a 44-year-old man who sustained a direct blow while working with his knees flexed in 20°. The patient was treated conservatively, and after a follow-up period of 8 months, fracture union was identified, with a normal range of motion and an absence of laxity and pain [7]. Open reduction and internal fixation is the first choice for the treatment of Hoffa fractures. Treatment goals include anatomic reduction, stable fixation, and early mobilization, as they refer to intra-articular fractures [8]. Conservative treatment with cylindrical plaster cast immobilization with the knee in 10° of flexion is associated with higher complication rates, including nonunion, post-traumatic arthritis, and knee dysfunction since the intra-articular fragment can be displaced by the popliteal and gastrocnemius muscles [9]. A least 2–3.5-mm-diameter screws are required to prevent rotational instability [10]. Screws placed from anterior to posterior cause minimal soft-tissue dissection, while biomechanically, posteroanterior screw has an advantage when the load is directed vertically [11]. Our case highlights a rare occurrence of bilateral medial femoral condyle Hoffa fractures after a motorbike collision. Diagnosis was confirmed using simple anteroposterior and lateral radiographs. A CT scan was obtained to clarify fracture patterns. The patient was treated operatively with three screws placed on both sides to prevent rotational instability. An anterior-to-posterior screw direction was selected due to its ease of application with minimal damage to the adjacent soft tissues. After a follow-up period of 3 months, good clinical outcomes were observed and the patient was able to return to his pre-injury level of activity.
Bilateral medial Hoffa fractures are rare injuries and easy to be misdiagnosed. High clinical suspicion combined with proper imaging, including oblique radiographs and CT scans, is of great significance. Open reduction and internal fixation is the proper treatment option for these fracture patterns, associated with good functional outcomes. However, more studies are required to determine the best diagnostic and therapeutic algorithm.
Bilateral medial Hoffa fractures are infrequent, accounting for 0.13% of all femoral fractures, and easy to be misdiagnosed. This is the second case report presenting bilateral fracture and the first using surgical treatment. Although the treatment can be either conservative or operative, we strongly support the open reduction and internal fixation due to the involvement of the articular surface and the exceptional functional outcomes of our patient in the 3-month follow-up.
References
- 1.Patel PB, Tejwani NC. The hoffa fracture: Coronal fracture of the femoral condyle a review of literature. J Orthop 2018;15:726-31. [Google Scholar]
- 2.Bartoníček J, Rammelt S. History of femoral head fracture and coronal fracture of the femoral condyles. Int Orthop 2015;39:1245-50. [Google Scholar]
- 3.Dhillon MS, Mootha AK, Bali K, Prabhakar S, Dhatt SS, Kumar V. Coronal fractures of the medial femoral condyle: A series of 6 cases and review of literature. Musculoskelet Surg 2012;96:49-54. [Google Scholar]
- 4.Zhou Y, Pan Y, Wang Q, Hou Z, Chen W. Hoffa fracture of the femoral condyle; Injury mechanism, classification, diagnosis, and treatment. Medicine 2019;98:e14633. [Google Scholar]
- 5.Kapoor C, Merh A, Shah M, Golwala P. A case of distal femur medial condyle hoffa type II(C) fracture treated with headless screws. Cureus 2016;8:e802. [Google Scholar]
- 6.Singh R, Singh RB, Mahendra M. Functional outcome of isolated hoffa fractures treated with cannulated cancellous screw. Malays Orthop J 2017;11:20-4. [Google Scholar]
- 7.Koné S, Bana A, Touré SA, Koné S, Allou AS, Kouassi AN, et al. Hoffa fracture of medial unicondylar and bilateral in a man: A rare case. Pan Afr Med J 2015;20:382. [Google Scholar]
- 8.Orapiriyakul W, Apivatthakakul T, Phornphutkul C. Relationships between Hoffa fragment size and surgical approach selection: A cadaveric study. Arch Orthop Trauma Surg 2018;138:1679-89. [Google Scholar]
- 9.Gao M, Tao J, Zhou Z, Liu Q, Du L, Shi J. Surgical treatment and rehabilitation of medial Hoffa fracture fixed by locking plate and additional screws: A retrospective cohort study. Int J Surg 2015;19:95-102. [Google Scholar]
- 10.Jarit GJ, Kummer FJ, Gibber MJ, Egol KA. A mechanical evaluation of two fixation methods using cancellous screws for coronal fractures of the lateral condyle of the distal femur (OTA type 33B). J Orthop Trauma 2006;20:273-6. [Google Scholar]
- 11.Kurahatti A, Seenappa H, Shanthappa AH, Nagakumar JS. The functional and radiological outcome of hoffa’s fracture treated with cannulated cancellous screws. Cureus 2022;14:e23829. [Google Scholar]