The posterior epidural migrated disc herniation at higher lumbar level may be associated with the fused spine as like adjacent segment disease.
Dr. Takuhei Kozaki, Department of Orthopaedic Surgery, Wakayama Medical University 811-1 Kimiidera, Wakayama City, Wakayama 641-8510, Japan. E-mail: t.kozaki@wakayama-med.ac.jp
Introduction: Disc sequestration is well known as a perforation of the fibrous ring and posterior longitudinal ligament, and migration of the fragment to the epidural space.
Case Report: A 62-year-old man complained of increased pain and hypoesthesia and muscle weakness of the left lower limb that had started 1 month before. Magnetic resonance imaging revealed a tumor-like mass at the L2–3 level on the posterior side of the dura. The fragment was strongly adhered to the dural sac and was resected piece by piece. Disc herniation recognized at L2–3 compressed the left L3 nerve root and was removed. The histopathological diagnosis was consistent with a degenerated intervertebral disc. All symptoms improved after the surgery.
Conclusions: There are few reports about the posterior migrated disc herniation at higher lumbar level. It may be associated with fused segments from L4 to the pelvis due to the previous surgery, which impacted the adjacent segment.
Keywords: Posterior epidural disc fragment, spinal tumor mimic, disc herniation, fused spine.
Disc sequestration is well known as a perforation of the fibrous ring and posterior longitudinal ligament, and migration of the fragment to the epidural space. Free fragments gradually migrate within the spinal canal in superior, inferior, and lateral directions [1, 2]. By contrast, posterior epidural migration away from the site of extrusion has been documented rarely. In addition, this pathology is often misidentified on magnetic resonance imaging (MRI) because it mimics several types of posterior epidural disease. In this report, we present a case of posterior epidural migrated lumbar disc herniation at the L2–3 level and focus on this pathology.
A 62-year-old man was admitted to the hospital with a 4-month history of intermittent pain in his lower back and in both thighs and residual urination. He had a history of prior spinal fusion surgery at L5–6. He complained of increased pain and hypoesthesia and muscle weakness of the left lower limb that had started 1 month before. MRI revealed a tumor-like mass at the L2–3 level on the posterior side of the dura. The lesion was hyperdense on T2-weighted and hypointense on T1-weighted images and showed ring enhancement after administration of gadolinium (Gd) (Fig. 1).
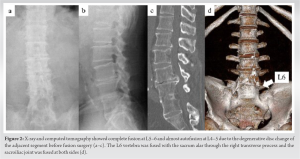
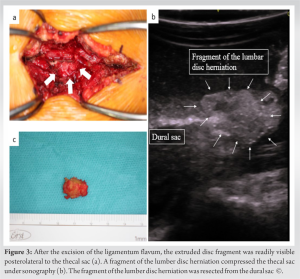
We have experienced a rare case of posterior epidural migrated disc herniation at L2-3, which seemed to be difficult to diagnose before the surgery. We resected them after the hemilaminectomy. The average age of patients with posterior epidural migrated disc fragments, most commonly at L3–L4 and L4–L5 [3-5]. The exact mechanism has not been cleared, but it has been thought as a combination of degeneration, anatomy, and age. The mean age was 54.05 years old [6]. The higher level at L3-4 or above was significantly related to the higher age than that of the herniation at L4-5 or below [7]. It was reported that the risk for degeneration at L3-4 increased with age [5, 8]. The main causative factors are thought to be a larger spinal canal and more activity in the L3–4 and L4–5 levels. in addition to insufficiency of ligaments and other supportive structures. The spinal canal is larger, and the intervertebral disc is more horizontal, and the anatomical relationship between the nerve root and disc space may result in a decrease in the barrier role of the nerve root at the L3-4 level [3]. In this case, the exact mechanism has not been cleared, but previous lumbar fusion and higher age were thought to be related to the posterior epidural migrated lumbar disc herniation occurred at L2–3, which is a higher level than has been reported previously [3-5]. Initially, it was thought that this patient displayed lumbar immobility from L4-pelvis, in addition, which impacted on the disc degeneration as adjacent segment disease at L2–3, together with the patient’s great age. The diagnosis of posteriorly migrated disc fragments is very difficult because the radiological appearance is like other common epidural lesions, such as synovial cysts, ligamentum cysts, cystic neurinomas, tumors, hematomas, and abscesses [9]. It was seemed that the sequestered disc generally causes an inflammatory reaction and neovascularization in its periphery. In general, posterior migrated disc fragments show hypointense on T1-weighted images, hyperintense on T2-weighted images [4, 5, 10], and rim enhancement after taking Gd, which is related to the inflammatory reaction and neovascularization around the migrated tissue [11, 12]. The case we presented also displayed ringlike peripheral contrast enhancement, which was consistent with previous reports [11]. Similarly most cases, we were unable to make a definitive diagnosis before the operation because the L2–3 level is not a frequently affected site, and the MRI appearance mimicked common epidural tumors, such as neurofibroma or meningioma. Our patient experienced posterior migrated epidural disc herniation that was resected surgically. To make a definitive diagnosis and escape the risk of cauda equina syndrome, surgical removal should be the first choice [6]. The several surgical procedures were performed. Laminectomy enables to see the whole of the fragments and remove easily but has the possibility of the instability [12]. Hemilaminectomy and laminotomy were better procedure to decrease the risk of the instability [13]. It has been reported that the minimally invasive procedures have good outcomes as laminectomy, but it has a risk for leftover of the fragments in case the fragments were, for example, tumors or abscesses [5]. In our case, we and the patient are afraid of the leftover of fragments of the tumors, we had chosen the hemilaminectomy to remove all of them and minimize the instability. In addition, we had to be careful of dura tearing due to the adhesions of the inflammation. It is better to prepare several methods to repair the dura before the surgery [14].
We have experienced the posterior epidural migrated herniation at the L2-3 level. It was a higher level than past reports, which was due to the fusion from L4 to the pelvis. In addition, higher age may have an effect on the disc herniation at L2-3. It was difficult to make the definitive diagnosis before the surgery, so we have chosen to perform the total resection under the hemilaminectomy. The spine surgeon should take into consideration of the possibility of the posterior epidural herniation even if at a higher level in the case who underwent fusion surgery.
This is a rare case of the posterior epidural migrated disc fragment at the L2-3 level. It was a higher level than past reports, which was due to the fusion from L4 to the pelvis. In addition, higher age may have an effect on the disc herniation at L2-3. It may be a kind of adjacent segment disease, which pathology may become more common in aging society.
References
- 1.Bonaroti EA, Welch WC. Posterior epidural migration of an extruded lumbar disc fragment causing cauda equina syndrome. Clinical and magnetic resonance imaging evaluation. Spine (Phila Pa 1976) 1998;23:378-81. [Google Scholar]
- 2.Schellinger D, Manz HJ, Vidic B, Patronas NJ, Deveikis JP, Muraki AS, et al. Disk fragment migration. Radiology 1990;175:831-6. [Google Scholar]
- 3.Akhaddar A, El-Asri A, Boucetta M. Posterior epidural migration of a lumbar disc fragment: A series of 6 cases. J Neurosurg Spine 2011;15:117-28. [Google Scholar]
- 4.Sengoz A, Kotil K, Tasdemiroglu E. Posterior epidural migration of herniated lumbar disc fragment. J Neurosurg Spine 2011;14:313-7. [Google Scholar]
- 5.Dösoğlu M, Is M, Gezen F, Ziyal MI. Posterior epidural migration of a lumbar disc fragment causing cauda equina syndrome: Case report and review of the relevant literature. Eur Spine J 2001;10:348-51. [Google Scholar]
- 6.Elsharkawy AE, Hagemann A, Klassen PD. Posterior epidural migration of herniated lumbar disc fragment: A literature review. Neurosurg Rev 2019;42:811-23. [Google Scholar]
- 7.Iwasaki M, Akino M, Hida K, Yano S, Aoyama T, Saito H, et al. Clinical and radiographic characteristics of upper lumbar disc herniation: Ten-year microsurgical experience. Neurol Med Chir (Tokyo) 2011;51:423-6. [Google Scholar]
- 8.Kanayama M, Togawa D, Takahashi C, Terai T, Hashimoto T. Cross-sectional magnetic resonance imaging study of lumbar disc degeneration in 200 healthy individuals. J Neurosurg Spine 2009;11:501-7. [Google Scholar]
- 9.Robe P, Martin D, Lenelle J, Stevenaert A. Posterior epidural migration of sequestered lumbar disc fragments. Report of two cases. J Neurosurg 1999;90:264-6. [Google Scholar]
- 10.Kuzeyli K, Cakir E, Usul H, Baykal S, Yazar U, Karaarslan G, et al. Posterior epidural migration of lumbar disc fragments: Report of three cases. Spine (Phila Pa 1976) 2003;28:E64-7. [Google Scholar]
- 11.D’Andrea G, Trillò G, Roperto R, Celli P, Orlando ER, Ferrante L. Intradural lumbar disc herniations: The role of MRI in preoperative diagnosis and review of the literature. Neurosurg Rev 2004;27:75-80. [Google Scholar]
- 12.Ba MC, Kleib R, Sy C, Diabang J, Ndoye N, Thiam AB, et al. Lumbar disc hernia migrating to the epidural posterior space: A rare entity. Internet J Neurosurg 2014;10:1-6. [Google Scholar]
- 13.Carvi y Nievas MN, Hoellerhage HG. Unusual sequestered disc fragments simulating spinal tumors and other space-occupying lesions. Clinical article. J Neurosurg Spine 2009;11:42-8. [Google Scholar]
- 14.Shimada Y, Hongo M, Miyakoshi N, Sugawara T, Kasukawa Y, Ando S, et al. Dural substitute with polyglycolic acid mesh and fibrin glue for dural repair: Technical note and preliminary results. J Orthop Sci 2006;11:454-8. [Google Scholar]










