Recognizing a unique peri-implant fracture pattern associated with an orthopedic implant with a successful treatment option avoiding the need for conversion to hemiarthroplasty.
Dr. Roy Small, Department of Orthopedic Surgery, Michigan State University, McLaren Macomb Medical Center, Mount Clemens, Michigan, USA. E-mail: roy.small@mclaren.org
Introduction: Peri-implant fractures (PIF) reported after cannulated screw and dynamic hip screw fixation historically occur distal to the implant within the subtrochanteric region secondary to the development of a stress riser. Newer implant designs for femoral neck fractures have attempted to combine the benefits of minimally invasive techniques without forgoing rigid angular stability but bring new potential complications.
Case Report: We present a case of an intertrochanteric PIF in the setting of a non-displaced femoral neck fracture treated with the DePuy Synthes Femoral Neck System (FNS).
Conclusion: We present this case of a unique PIF pattern with the hope of identifying a potential complication associated with the novel FNS. Furthermore, we present a successful treatment option avoiding the need for conversion to hemiarthroplasty.
Keywords: Femoral neck fracture, intertrochanteric fracture, femoral neck system, peri-implant fracture.
Newer implant designs for femoral neck fractures have attempted to combine the benefits of minimally invasive cannulated screw fixation with the rigid angular stability seen with dynamic hip screws (DHS) [1]. The femoral neck system (FNS) (Fig. 1) is one such design (DePuy Synthes, West Chester, Pennsylvania, USA). Fixation of femoral neck fractures is associated with a higher incidence of complications than any other fracture [2]. Complications following the fixation of non-displaced femoral neck fractures include non-union, avascular necrosis, implant cutout, varus collapse, and subtrochanteric peri-implant fracture (PIF) [3]. Subtrochanteric PIFs associated with cannulated screw fixation and DHS constructs lead to additional reoperation risks, particularly in the immunocompromised and osteoporotic elderly patient [4]. In this article, we present a case of an intertrochanteric PIF in the setting of a non-displaced femoral neck fracture treated with the FNS. This case report is the first of its kind highlighting an unexpected fracture pattern associated with a novel implant system utilized in the treatment of femoral neck fracture.
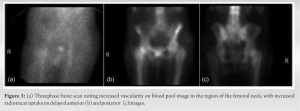
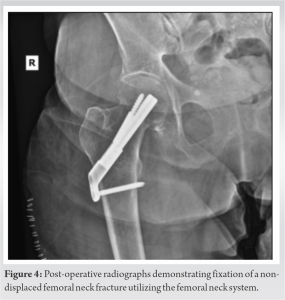
An 82-year-old female presented with right hip/groin pain and an inability to ambulate after a ground-level fall from standing at home. Persistent pain on clinical examination prompted advanced imaging for suspicion of occult femoral neck fracture despite a negative radiographic workup utilizing plain radiographs (Fig. 2a) and a CT scan (Fig. 2b).
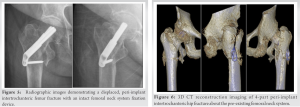
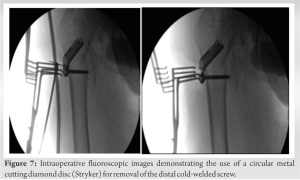
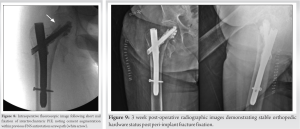
Non-displaced and valgus-impacted femoral neck fractures, classified as Garden I or II, are routinely treated with multiple cannulated screws or DHS constructs. Several studies have examined the complications associated with such fixation devices, estimating 3–13% complication rate of implant cut-out, varus collapse, and/or subtrochanteric PIF [5, 6]. PIFs reported with cannulated screw and DHS fixation historically occur distal to the implant within the subtrochanteric region. This is due to the increased stress secondary to the stiff implants used to obtain compression through the femoral neck. With axial loading coupled with abductor muscle distraction, the stiff construct creates a weak point concentrated in the subtrochanteric region, lending to the predictable PIF pattern [7]. Biomechanical evaluation of 2-hole and 4-hole DHS constructs placed under cyclic loading demonstrate similar PIF patterns, with failure occurring either just distal to the plate or at the level of the lag screw hole within the subtrochanteric region [8]. A tip-to-apex distance of <25 mm has been shown to increase the risk of screw cutout but has not been associated with a similar fracture pattern to our case [9]. The same subtrochanteric fracture pattern is also noted in studies evaluating PIFs in the setting of DHS and cephalomedullary implants used to treat intertrochanteric hip fractures [10]. These complications can be devastating, having shown severe complications in elderly osteopenic patients [4]. Rates of reoperation following fixation of stable femoral neck fractures, including conversion to arthroplasty or removal of the instrumentation with cephalomedullary nailing, range from 4 to 12% [11, 12]. Bhandari et al. identified a 21% overall reoperation rate when comparing DHS and cannulated screw fixation of non-displaced femoral neck fracture [13]. This complication profile drives the development of biomechanically superior implants. The FNS, developed by DePuy Synthes, was recently introduced in hopes to reduce such complications and reoperation rates through its reported stronger integrated rotational stability and minimally invasive compact design [5]. Moreso, the lateral locking plate of the FNS serves as a means of preventing lateral bolt prominence and subsequent abductor irritation commonly encountered with cannulated screw fixation and DHS devices. Several case studies and reports have demonstrated good outcomes utilizing the FNS for non-displaced, and even displaced femoral neck fractures in elderly and young patient populations alike [1]. However, to date, there are no reports of PIF in the setting of the novel FNS system. Based on previously published data, one would expect similar subtrochanteric fracture patterns associated with the FNS as seen with cannulated screws, DHS s, and cephalomedullary implants. We hypothesize the derotational screw divergence of the FNS may act as a stress riser within the intertrochanteric region leading to the fracture pattern discussed in this case report. Weaknesses of this article include those inherent to a single patient case report as well as a lack of literature surrounding complications of the FNS. Furthermore, we acknowledge the optimal treatment of minimally displaced femoral neck fractures is debated in the literature. Treatment with hemiarthroplasty has been shown to have lower reoperation rates as well as improved post-operative mobility [14, 15]. This case highlights an unexpected complication seen with the FNS: an intertrochanteric PIF in the setting of a previous non-displaced femoral neck fracture stabilized with the FNS. While our proposed treatment option appeared to be successful in the fixation of the PIF while avoiding conversion to hemiarthroplasty, long-term follow-up is not available at this time as the patient was lost to follow-up.
Newer implant designs such as the FNS combine the advantages of minimally invasive cannulated screw fixation with the higher mechanical stability seen with laterally fixated dynamic compression devices [1]. With higher stability and stiffness, concerns may arise with forces transferred to the surrounding bone. Subtrochanteric fractures encountered in cases of PIFs about cancellous screws and DHS constructs have been reported in the literature. To the best of our knowledge, this case is the first presented in the literature to report an intertrochanteric PIF associated with the newer FNS. A larger powered study is needed to form a proper correlation with our anecdotal findings, however, this report may be the first in potentially identifying unique PIF pattern association.
We present this case of a unique PIF pattern with the hope of identifying a potential complication associated with the novel FNS. Furthermore, we present a successful treatment option avoiding the need for conversion to hemiarthroplasty.
References
- 1.Stoffel K, Zderic I, Gras F, Sommer C, Eberli U, Mueller D, et al. Biomechanical evaluation of the femoral neck system in unstable Pauwels III femoral neck fractures: A comparison with the dynamic hip screw and cannulated screws. J Orthop Trauma 2017;31:131-7. [Google Scholar]
- 2.Estrada LS, Volgas DA, Stannard JP, Alonso JE. Fixation failure in femoral neck fractures, clinical orthopaedics and related research. Clin Orthop Relat Res 2002;399:110-8. [Google Scholar]
- 3.Biz C, Tagliapietra J, Zonta F, Belluzzi E, Bragazzi NL, Ruggieri P. Predictors of early failure of the cannulated screw system in patients, 65 years and older, with non-displaced femoral neck fractures. Aging Clin Exp Res 2020;32:505-13. [Google Scholar]
- 4.Jansen H, Frey SP, Meffert RH. Subtrochanteric fracture: A rare but severe complication after screw fixation of femoral neck fractures in the elderly. Acta Orthop Belg 2010;76:778-84. [Google Scholar]
- 5.Matsumura T. FNS Case Study: Valgus Impacted Non-displaced Subcapital Femoral Neck Fracture in Elderly Patient. JnJ Medical Devices., Synthes USA Products, Monument, CO.; 2020. Available from: ??? [Last accessed on 2021 May 14]. [Google Scholar]
- 6.Zhang LL, Zhang Y, Ma X, Liu Y. Multiple cannulated screws vs. dynamic hip screws for femoral neck fractures: A meta-analysis. Orthopade 2017;46:954-62. [Google Scholar]
- 7.Tsai AG, Reich MS, Bensusan J, Ashworth T, Marcus RE, Akkus O. A fatigue loading model for investigation of iatrogenic subtrochanteric fractures of the femur. Clin Biomech (Bristol, Avon) 2013;28:981-7. [Google Scholar]
- 8.Rog D, Grigsby P, Hill Z, Pinette W, Inceoglu S, Zuckerman L. A biomechanical comparison of the two- and four-hole side-plate dynamic hip screw in an osteoporotic composite femur model. J Orthop Surg (Hong Kong) 2017;25:2309499017717199. [Google Scholar]
- 9.Rubio-Avila J, Madden K, Simunovic N, Bhandari M. Tip to apex distance in femoral intertrochanteric fractures: A systematic review. J Orthop Sci 2013;18:592-8. [Google Scholar]
- 10.Müller F, Galler M, Zellner M, Bäuml C, Marzouk A, Füchtmeier B. Peri-implant femoral fractures: The risk is more than three times higher within PFN compared with DHS. Injury 2016;47:2189-94. [Google Scholar]
- 11.Kain MS, Marcantonio AJ, Iorio R. Revision surgery occurs frequently after percutaneous fixation of stable femoral neck fractures in elderly patients. Clin Orthop Relat Res 2014;472:4010-4. [Google Scholar]
- 12.Bigoni M, Turati M, Leone G, Caminita AD, D’Angelo F, Munegato D, et al. Internal fixation of intracapsular femoral neck fractures in elderly patients: Mortality and reoperation rate. Aging Clin Exp Res 2019;32:1173-8. [Google Scholar]
- 13.Bhandari M, Devereaux PJ, Guyatt G, Thabane L, Walter SD, Heetveld MJ, et al. Fracture fixation in the operative management of hip fractures (FAITH): An international, multicentre, randomised controlled trial. Lancet 2017;389:1519-27. [Google Scholar]
- 14.Dolatowski FC, Frihagen F, Bartels S, Opland V, Šaltytė Benth J, Talsnes O, et al. Screw fixation versus hemiarthroplasty for nondisplaced femoral neck fractures in elderly patients: A multicenter randomized controlled trial. J Bone Joint Surg Am 2019;101:136-44. [Google Scholar]
- 15.Ma HH, Chou TA, Tsai SW, Chen CF, Wu PK, Chen WM. Outcomes of internal fixation versus hemiarthroplasty for elderly patients with an undisplaced femoral neck fracture: A systematic review and meta-analysis. J Orthop Surg Res 2019;14:320. [Google Scholar]











