ACL injury in genu recurvatum with neuromuscular weakness can be challenging, however, it can be treated successfully with the right pre-operative planning, intraoperative execution, and post-operative therapy.
Dr. Jignesh Y Tandel, Department of Orthopaedics, Murup Hospital, Changwon, Gyeongnam, South Korea. E-mail: drjigneshtandel@gmail.com
Introduction: People with post-polio syndrome usually have some residual deformities. Genu recurvatum is very commonly seen in such cases which are a risk factor for anterior cruciate ligament (ACL) injury due to the altered biomechanics. To the best of our knowledge, this is the first report in literature presenting ACL reconstruction in a limb with genu recurvatum deformity treated with supracondylar osteotomy.
Case Report: A 49-year-old female with genu recurvatum and history of polio presented with pain and instability. Staged procedure of supracondylar osteotomy and ACL reconstruction Achilles allograft was done.
Conclusion: ACL tears in a poliotic limb with genu recurvatum deformity can be a challenging case. Precise pre-operative preparation can aid in managing the case successfully.
Keywords: ACL injury, polio, ACL reconstruction, Achilles allograft, genu recurvatum deformity.
Genu recurvatum is a sagittal deformity of the knee and is defined as hyperextension more than 5° [1]. In physiological limits, hyperextension helps in locking the knee which is useful during walking, standing, and also stabilizing legs which are paralytic. Hyperextension 5° or more leads to structural changes in anatomy which results in progressive deformities such as genu recurvatum, knee pain, muscle weakness, and instability during motion [2]. Genu recurvatum maybe congenital or present with acquired disorders such as paralysis, poliomyelitis, rheumatoid arthritis, or other knee deformities [3]. The causes can be broadly divided into neurological (polio, cerebral palsy, spastic lesions, multiple sclerosis, etc.) and non-neurological (rheumatoid arthritis, osteoarthritis, post-HTO, post-traumatic, tibial epiphyseal plate injury, limb length discrepancies, etc.). The pathoanatomy of the deformity is related to overstretching of soft tissues or bony deformities. Due to hyperextension, there is posterior stretching of the capsule, associated with strain on the cruciate ligaments. These changes convert the posterior soft-tissue structures into a hammock. This leads to progressive ligament laxity causing instability. Bony changes such as femoral condyle flattening and tibia slope anomalies are also seen. In cases of chronic anterior knee pain resulting due to trauma or post-surgery, patients often walk with a quadriceps avoidance gait [4]. In this, the knee is pushed backwards during walking to avoid excessive load on patella which again causes posterior capsular stretching. One of the most common causes of genu recurvatum is polio in which the quadriceps are affected [5]. In these cases, there is alteration of the weight-bearing line to prevent anterior collapse of the knee. Such patients lock the knee through hyperextension, leading to continuous stretching of the posterior capsule and strain on the anterior ligaments of the joint. This leads to increasing energy expenditure during walking due to increased vertical movements of the center of gravity of the body [6] and progressive genu recurvatum caused by chronic stretching of the posterior soft tissues of the knee. Femoral condylar flattening and tibial slope anomalies are common in polio which poses a high risk for anterior cruciate ligament (ACL) injury. Genu recurvatum is a manifestation of post-polio syndrome and can be managed by conservative or surgical measures. Selecting the treatment depends on identifying the cause of deformity. Various surgical procedures such as tendon transfers, ligamentoplasties, patella bone blocks, proximal tibial osteotomies, and femoral osteotomies have been described in literature. For deformities arising from tibia, an oblique anterior opening-wedge proximal tibial osteotomy is the widely accepted treatment for osseous GR. Supracondylar femoral flexion osteotomy is another method of treatment for genu recurvatum arising from femur, which is commonly performed. In this technique, an open-wedge osteotomy is made in the supracondylar area of the femur, and an allograft is used to fill the resulting gap and fixed with a plate. The ACL is one of the most frequently injured ligaments of the knee in Asian population [7]. The ACL is considered as the main restraint on the tibia’s anterior translation relative to the femur. The ACL contributes to the stability of the knee during rotation in both the frontal and transverse planes due to its specific alignment. Injury to the ACL may also result from a loss of neuromuscular control during dynamic movements [8].
In this report, we present a case of genu recurvatum with ACL injury in a poliotic limb, treated with supracondylar femur flexion osteotomy and ACL reconstruction with Achilles allograft in a staged procedure.
A 49-year-old female, known case of poliomyelitis, came with complains of pain and right knee instability. The pain and deformity were gradually progressing. On clinical examination, genu recurvatum deformity of 20° was seen. Lachman’s and anterior drawer test were positive. The power of the quadriceps was 4+ and there was no other deformity in the right lower limb. Long leg standing films showed severe hyperextension of 20° and varus with femoral condyle flexion deformity and flattening (Fig. 1a).
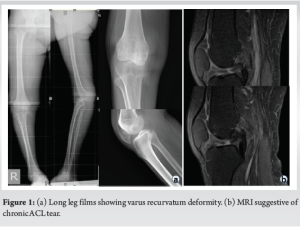
Radiological investigations revealed complete ACL tear with complex tear of both menisci and osteoarthritis (Fig. 1b).
The patient was planned for a two-stage procedure with supracondylar femur osteotomy first for correction of recurvatum, followed by ACL reconstruction.
To protect the quadriceps, a lateral incision was taken for the osteotomy. After incising periosteum, the anterior two-thirds of the femur was osteotomized just above the trochlea level, and opened to correct the deformity leaving the posterior cortex intact. Iliac strut bone graft was filled in the osteotomy gap and fixed by a plate (Fig. 2a).

The deformity was corrected clinically and radiologically (Fig. 2b).
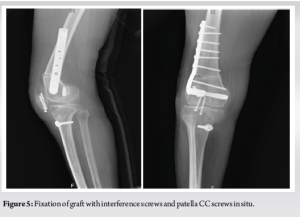
The patient was being followed up regularly but after 3 months post-operative suffered a lower pole patella fracture which was fixed with CC screws.

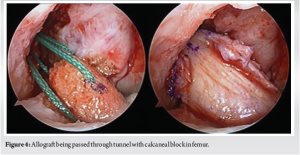
At a later stage, ACL reconstruction was planned. The author WHJ routinely does ACLR with bone patella tendon graft using a custom-made scalpel of 1 cm width (Fig. 3). However, due to the history of patella fracture, it was decided to avoid the BTB graft and Achilles allograft was chosen. Under spinal anesthesia, using high anterolateral and anteromedial portals, diagnostic arthroscopy was performed which revealed complete ACL tear with complex tears of both menisci. Partial medial and lateral meniscectomy was done. Tibial and femoral tunnels were prepared using transtibial technique. Graft was prepared as per standard procedure and passed through the tunnels with the calcaneal bone block placed in the femur (Fig. 4). Femoral fixation of graft was done by Kurosaka screw and with bio screw in tibia (Fig. 5).
The patient was kept on knee brace initially and started on physiotherapy. Gradually, the patient progressed from partial weight-bearing to full weight-bearing and within 1 month was able to do 90° flexion. There was improvement in laxity and Lachman’s test was negative.
On reviewing the literature, we did not find any report or data of such a case of ACLR with Achilles tendon in GR with supracondylar osteotomy. Saita et al., found that the load on the ACL is relatively higher in patients with genu recurvatum than in those without genu recurvatum [9]. According to Cooper et al., mechanical load on the reconstructed ligament is high in the patients with genu recurvatum [10]. Guimarães et al. found that patients with more than 5° of contralateral knee hyperextension with single-bundle ACL reconstruction had a higher failure rate than patients with <5° of knee hyperextension [11]. Noyes et al. have described triple varus deformity (tibiofemoral varus + lateral compartment separation + varus hyperextension) [12]. In their study, they have suggested that osseous deformity should be corrected followed by ligament reconstruction procedures. According to Perry, the treatment of significant bone deformities in the femur or tibia should occur first, followed by the correction of soft-tissue laxities, using an osteotomy [13]. This was followed in our case also in which a femoral supracondylar osteotomy was done to correct the recurvatum deformity and ACL reconstruction at a later stage. Genu recurvatum is a common manifestation of post-polio syndrome. The nonsurgical treatment like a hinged leg orthosis is used occasionally. Surgical treatment options are selected after evaluation of the cause of deformity (osseous, ligamentous, or mixed). Early treatment options used to comprise tendon transfers and ligamentoplasties [14]. The failure of these methods led to creation of bony blocks to extension. Campbell fused the lower end of patella to anterior aspect of the tibia [15]. Mayer took a graft from femur or tibia and attached it on the upper surface of tibia and fused the protruding end with denuded surface of lower pole of patella [16]. Brett suggested an incomplete osteotomy of the tibia just below the capsular attachment, filling it with bone graft and immobilization in cast [17]. Osseous genu recurvatum arising due to tibia is typically treated by an oblique anterior opening-wedge proximal tibial osteotomy. Kim et al. showed a modified proximal tibia anterior wedge osteotomy for correction of deformity [18]. Mehta and Mukherjee did femoral supracondylar flexion osteotomy in their patients of genu recurvatum and concluded that there was remodeling in flattened femoral condyles and it also provided a bony block to hyperextension [19]. During walking, the shortening produced by recurvatum causes an increased vertical excursion of the center of gravity at each step. Correction of the deformity, therefore, reduces the energy expenditure of walking [19]. Some of the challenges in ACL reconstruction in recurvatum limbs with neuromuscular disorder include: Pre-operative planning should take into account the patient’s expectations and demands in addition to assessing all abnormalities, grading muscular strength, and taking radiographs to determine the quality of the patient’s bones. Graft selection: We decided to use Achilles allograft due to previous history of patella fracture and avoid complications seen with hamstrings graft and also the fact that there was mild quadriceps weakness. Difficulty in assessing joint stability: Assessing joint stability can be challenging in recurvatum patients due to the bony and ligamentous changes of the affected limb. Before surgery, adequate radiographic investigations should be made. To correlate the clinical and radiological data, a diagnostic arthroscopy should always be carried out first. Rehabilitation: Following surgery, rehabilitation and physical therapy may need to be altered to meet the patient’s specific needs. Risk of complications: Recurvatum patients may be at increased risk of complications following ACL reconstruction surgery as discussed above.
In conclusion, the case presented here underscores the complexity and challenges involved in managing genu recurvatum with concomitant ACL injury, especially in patients with neuromuscular disorders such as poliomyelitis. The staged approach involving femoral supracondylar osteotomy followed by ACL reconstruction with Achilles allograft proved to be effective in correcting the deformity and restoring knee stability. This report highlights the importance of individualized treatment strategies tailored to the patient’s unique circumstances, including prior surgical history and neuromuscular status. Furthermore, it emphasizes the significance of thorough preoperative planning, careful graft selection, and postoperative rehabilitation to optimize outcomes and minimize complications. While this case adds to the growing body of literature on managing complex knee pathologies, further research is warranted to refine treatment algorithms and improve patient outcomes in similar challenging scenarios.
A salient feature of this article is the efficacy of a methodical progression, commencing with corrective osteotomy prior to ligament reconstruction for tackling the combined challenges of genu recurvatum and ACL injury.
References
- 1.Zein AM, Mahmoud Hassan AZ, Saleh Elsaid AN. Biological bone plate and iliac bone autograft for proximal tibial slope changing osteotomy in genu recurvatum. Arthrosc Tech 2022;11:e989-98. [Google Scholar]
- 2.Dean RS, Graden NR, Kahat DH, DePhillipo NN, LaPrade RF. Treatment for symptomatic genu recurvatum: A systematic review. Orthop J Sports Med 2020;8:2325967120944113. [Google Scholar]
- 3.Appasamy M, De Witt ME, Patel N, Yeh N, Bloom O, Oreste A. Treatment strategies for genu recurvatum in adult patients with hemiparesis: A case series. PM R 2014;7:105-12. [Google Scholar]
- 4.D’Ambrosi R, Meena A, Raj A, Ursino N, Hewett TE. Anterior knee pain: State of the art. Sports Med Open 2022;8:98. [Google Scholar]
- 5.Joseph B, Watts H. Polio revisited: Reviving knowledge and skills to meet the challenge of resurgence. J Child Orthop 2015;9:325-38. [Google Scholar]
- 6.Bagherifard A, Rahbar M, Shahsavari A, Moaiedfar M, Bahrabadi M. Flexion Osteotomy in genu recurvatum following post-polio syndrome: Use of an old technique in a new condition. Shafa Ortho J 2017;4:e10530. [Google Scholar]
- 7.Tandel JY, Wagh AA, Girde V, Jagtap KR, Chaudhari N. ACL reconstruction in a poliotic limb with peroneus longus graft. J Orthop Case Rep 2023;13:133-7. [Google Scholar]
- 8.Kakavas G, Malliaropoulos N, Pruna R, Traster D, Bikos G, Maffulli N. Neuroplasticity and anterior cruciate ligament injury. Indian J Orthop 2020;54:275-80. [Google Scholar]
- 9.Saita Y, Schoenhuber H, Thiébat G, Ravasio G, Pozzoni R, Panzeri A, et al. Knee hyperextension and a small lateral condyle are associated with greater quantified antero-lateral rotatory instability in the patients with a complete anterior cruciate ligament (ACL) rupture. Knee Surg Sports Traumatol Arthrosc 2019;27:868-74. [Google Scholar]
- 10.Cooper DE, Dunn WR, Wright RW, Haas A, Huston LJ. Knee hyperextension as a predictor of failure in revision ACL reconstruction: A prospective cohort study. Orthop J Sports Med 2016;4:2325967116S00187. [Google Scholar]
- 11.Guimarães TM, Giglio PN, Sobrado MF, Bonadio MB, Gobbi RG, Pécora JR, et al. Knee hyperextension greater than 5° is a risk factor for failure in ACL reconstruction using hamstring graft. Orthop J Sports Med 2021;9:23259671211056325. [Google Scholar]
- 12.Noyes FR, Barber-Westin SD, Hewett TE. High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Am J Sports Med 2000;28:282-96. [Google Scholar]
- 13.Perry J, O’Brien JP, Hodgson AR. Triple tenodesis of the knee. A soft-tissue operation for the correction of paralytic genu recurvatum. J Bone Joint Surg Am 1976;58:978-85. [Google Scholar]
- 14.Heyman CH. A method for the correction of paralytic genu recurvatum: Report of a bilateral case. JBJS 1924;6:689. [Google Scholar]
- 15.Campbell WC, Mitchell JI. Operative treatment of paralytic genu recurvatum. Ann Surg 1932;96:1055-64. [Google Scholar]
- 16.Mayer L. An operation for the cure of paralytic genu recurvatum. JBJS 1930;12:845. [Google Scholar]
- 17.Brett AL. Operative treatment of genu recurvatum. Am J Surg 1939;43:466-72. [Google Scholar]
- 18.Kim TW, Lee S, Yoon JR, Han HS, Lee MC. Proximal tibial anterior open-wedge oblique osteotomy: A novel technique to correct genu recurvatum. Knee 2017;24:345-53. [Google Scholar]
- 19.Mehta SN, Mukherjee AK. Flexion osteotomy of the femur for genu recurvatum after poliomyelitis. J Bone Joint Surg Br 1991;73:200-2. [Google Scholar]







