Debridement, antibiotics, and implant retention may be considered a surgical treatment of acute hematogenous periprosthetic joint infection in a medically infirm patient unable to undergo exchange arthroplasty.
Ms. Senah E. Stephens, Eastern Virginia Medical School, P.O. Box 1980, Norfolk, VA 23501-1980. E-mail: stephese@evms.edu
Introduction: Periprosthetic joint infection (PJI) is an unfortunate but frequent complication following total hip arthroplasty, with an incidence of 1%. Debridement, antibiotics, and implant retention is a treatment option for acute hematogenous PJI, with success rates reported up to 70%. Here, we present a case demonstrating short-term success using this treatment approach in a 74-year-old medically infirm patient.
Case Report: The patient – a 74-year-old male with well-functioning bilateral total hip arthroplasties performed 14 years prior – presented to a rural emergency department with an acute onset of right groin pain and dizziness. The patient was found to have sepsis, a right hip joint effusion, and periarticular abscesses on assessment. Synovial fluid aspiration from the right hip grew methicillin-sensitive Staphylococcus aureus. The patient was transferred to an outside hospital for limited debridement of the right hip joint, followed by transfer to our tertiary hospital. On arrival, consideration was given to performing an exchange arthroplasty. However, given the patient’s medical frailty, it was felt that the risks were prohibitive, as supported by the presence of ileus, severe electrolyte imbalance, anemia requiring transfusion, anasarca, and vancomycin-resistant Enterococcus faecium infection of a sacral wound. The patient underwent surgery utilizing an established protocol of aggressive debridement and cleaning of the hip space, exchange of the modular arthroplasty components, and placement of antibiotic calcium sulfate beads for local delivery. The patient was treated with parenteral antibiotics followed by chronic oral antimicrobial suppression for 10 months after the final surgery. During treatment, the patient’s inflammatory markers have normalized. The patient is ambulatory without assistive devices but uses an ankle orthosis due to a post-operative foot drop that did not resolve. The patient has regained satisfactory mobility with an Oxford hip score of 27.
Conclusion: This case demonstrates short-term success in the treatment of acute hematogenous PJI in a medically infirm patient utilizing debridement, antibiotics, and implant retention and may serve to inform future patient counseling.
Keywords: Joint infection, debridement, antibiotics, and implant retention, antibiotics, total hip arthroplasty, revision arthroplasty.
Total joint arthroplasty (TJA) is the definitive treatment option for aging adults faced with debilitating osteoarthritis of the hip and knee. Total joint replacement surgeries are increasing in incidence as the population ages, life expectancy increases, and obesity persists [1, 2]. Periprosthetic joint infection (PJI) is one of the most expensive and difficult-to-treat complications following TJA [1, 2]. Although PJI affects approximately 1.2% of patients after total hip arthroplasty (THA), it is the third most common cause for revision, accounting for at least 14.8% of cases [2, 3]. PJI can be divided into four classifications: acute, delayed, acute hematogenous, and positive intraoperative cultures [4]. Treatment decisions are often dictated by classification [4]. For acute or acute hematogenous PJI, surgical management may include debridement, antibiotics, and implant retention (DAIR) [4]. The gold standard for complete eradication of PJI is implant removal in a one or two-stage exchange arthroplasty [4]. There are mixed reports in the literature surrounding the effectiveness of DAIR in the treatment of PJI. In a meta-analysis of 65 studies, Gerritsen et al. reported a pooled overall success rate of 70% [5]. If initial DAIR fails and infection recurs, subsequent treatment options include repeat DAIR, one- or two-stage exchange arthroplasty, permanent resection arthroplasty, or amputation [6, 7]. PJIs treated with exchange arthroplasty typically follow a two-stage reimplant protocol over several months duration [6, 8]. In a two-stage exchange arthroplasty, the first stage involves the removal of the infected implant components, debridement of soft tissues, insertion of an antibiotic spacer, and administration of parenteral antibiotics [6]. The antibiotic-impregnated cement spacer is inserted to maintain the joint space, affording the patient some level of functional mobility throughout the duration of treatment [6]. After 6 weeks of antibiotic treatment, the second stage proceeds with removal of the antibiotic spacer, collection of tissue for culture, repeat debridement and irrigation of the joint, bone grafting if necessary, and reimplantation of hip prosthesis [6]. Barton et al. reported a mortality risk of 23.6% and a reinfection rate of 14.8% in patients who underwent two-stage exchange arthroplasty [9]. Uchiyama et al. reported a higher success rate of 91.7% for two-stage exchange arthroplasty [6]. Consideration must be given to the total number of operations and length of recovery patients face when undergoing two-stage exchange arthroplasty. In comparison, DAIR may be a conservative treatment option for acute hematogenous PJI to reduce blood loss, total operative time, length of recovery, and bone and soft-tissue damage [10]. In this case report, we describe a previously healthy 74-year-old male with bilateral well-functioning total hip arthroplasties presenting with sepsis and periarticular abscesses from PJI of the right hip. The case aims to demonstrate the short-term success of DAIR in the treatment of acute hematogenous PJI in a critically ill patient not deemed a medical candidate for staged revision arthroplasty. Few studies have assessed the utility of DAIR in the treatment of acute hematogenous PJI occurring >10 years after index THA.
Background
A 74-year-old male presented to a rural emergency department with an acute onset of right groin pain and dizziness. The patient’s chronic medical conditions included primary hypertension controlled with lisinopril, Vitamin D deficiency treated with ergocalciferol, and obesity with a BMI of 33.39. The patient reported a 35-year history of chewing tobacco use with cessation 22 years prior. The patient denied alcohol or recreational drug use. Physical exam was positive for tachypnea, hypotension, tachycardia, and bilateral lower extremity edema. Laboratory testing demonstrated toxic metabolic encephalopathy, lactic acidosis, acute kidney injury, hypomagnesemia, hyponatremia, hypochloremia, hypocalcemia, and leukocytosis.
Orthopedic assessment
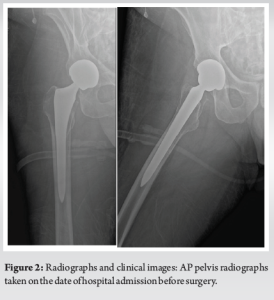
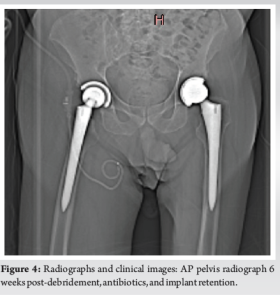
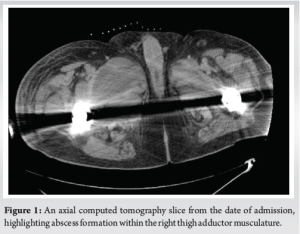
On presentation, an axial computed tomography scan of the abdomen and pelvis was also obtained, which demonstrated an abscess in the right adductor compartment measuring 9.1 × 5.8 cm and an abscess between the gluteus medius and maximus measuring 5.6 × 12.8 cm (Fig. 1). An X-ray of the right hip and lumbar spine was also obtained (Fig. 2). Initial laboratory results showed a serum C-reactive protein of 43 mg/L, erythrocyte sedimentation rate of 68 mm/h, white blood cell count of 24,000 cells/μL, and a D-dimer of 2.15 μg fibrinogen equivalent units/mL. After initial evaluation in the rural emergency department, the patient was transferred to a larger hospital for consultation by orthopedic surgery. The patient underwent several aspirations of the right hip at both the outside hospital and tertiary center. Aspirates grew methicillin-sensitive Staphylococcus aureus (MSSA) on culture with a segmented neutrophil count of 96% and a total nucleated count of 564,000/μL. These findings met the major criteria for PJI according to guidelines from the Musculoskeletal Infection Society [11].
Intervention
At the outside hospital, the patient was started on parenteral vancomycin and meropenem after diagnosis of MSSA PJI and bacteremia. The patient underwent an urgent but limited debridement of the right hip joint space with the placement of calcium sulfate antibiotic beads. This hospitalization was complicated by lung atelectasis, ileus, anasarca, and severe electrolyte imbalance. Eight days after admission, the patient was transported to our tertiary care facility for further orthopedic evaluation.
On arrival, consideration was given to performing an exchange arthroplasty. Despite improvements noted in the patient’s overall medical status as compared to the initial presentation, the patient remained medically frail with leukocytosis (ASA 4). A shared discussion was held with the patient and family regarding the risks and benefits of exchange arthroplasty versus DAIR. Based on this informed discussion, the decision was made to proceed with DAIR. On day 4 of admission to our tertiary hospital, the patient underwent DAIR. At our institution, the DAIR protocol involved complete synovectomy, followed by exhaustive debridement of residual synovial tissue. Tissue samples were collected aseptically for culture. Next, an antiseptic solution of povidone-iodine was used to copiously irrigate the wound. The sterile field was replaced with a clean setup. Then, we performed an aseptic exchange of the modular components–including the femoral head and acetabular liner. Calcium sulfate antibiotic beads were loaded with 1 g vancomycin and 240 mg gentamicin and inserted into the right hip joint for local delivery (Fig. 3). The patient was noted to have a metal-on-metal bearing joint with no metallosis. The wound was closed, and negative pressure wound therapy was applied due to concerns of delayed healing. There were no intraoperative complications. However, the patient developed a right foot drop immediately following the procedure.
Post-operative management
Once stabilized by day 18 of admission, the patient was transferred to an in-patient rehabilitation facility for daily physical and occupational therapy. Within a week, the patient’s laboratory results demonstrated up-trending leukocytosis. The patient became febrile, had worsening of a sacral decubitus ulcer, and developed warmth and redness of the rip hip surgical site, prompting readmission to the hospital for an infection workup.
On readmission, the patient was diagnosed with cellulitis of the abscess drainage site in the right adductor compartment. The patient also developed vancomycin-resistant Enterococcus faecium infection of a sacral wound. Parenteral cefepime was added to the patient’s antibiotic regimen for 1 week. This readmission was complicated by anemia requiring transfusion and an acute episode of pain and edema of the right hand, concerning septic arthritis. Arthrocentesis with crystal analysis of the fluid demonstrated calcium pyrophosphate dihydrate crystal accumulation, suggestive of pseudogout due to hypomagnesemia. On day 9 of hospital readmission, pelvic imaging demonstrated repeat abscess formation in the right medial thigh. Interventional radiology removed 33 mL of purulent fluid from the right medial thigh and placed a pigtail drain. Parenteral nafcillin and oral rifampin were added to the patient’s antibiotic regiment by infectious disease consult. On day 11 of hospital readmission, the patient was discharged to another in-patient rehabilitation center with orders to receive continued parenteral antibiotic treatment and daily therapy. The pigtail drain in the right adductor compartment was removed 22 days after placement once imaging showed the resolution of the periarticular abscesses (Fig. 4). After regaining the ability to perform activities of daily living, the patient was discharged home at 15 weeks post-DAIR. The patient continued oral doxycycline and rifampin daily. At 6 months after the final surgery, the patient was decreased to oral doxycycline daily. At 10 months after the final surgery, infectious disease discontinued chronic antimicrobial suppression.
Outcomes
Over the course of treatment, the patient showed normalization of inflammatory markers. The patient is ambulatory without assistance and has returned to some of their previous activities. The patient’s right foot drop persists along with atrophy and dysesthesias of the anterior lower leg. Possible etiologies of sciatic nerve injury during posterior hip exposures include direct injury, ischemia, traction, compression, and heat, among other causes. Special consideration should be taken to optimize limb placement and padding during surgery. In addition, retraction around the acetabulum must be carefully performed to reduce mechanical stress on the nerve, thus lowering the risk of iatrogenic nerve injury. The patient utilizes an ankle-foot orthosis as needed. The patient is being monitored for signs of reinfection following cessation of antibiotic therapy.
Success rates for DAIR used in the treatment of hip PJI are reported up to 70% [5]. Although single operations such as one-stage exchange arthroplasty or resection arthroplasty provide benefits such as decreased morbidity and mortality, decreased economic burden, and decreased length of hospitalization, the patient was not deemed a candidate for either procedure. One-stage exchange arthroplasty was contraindicated due to the presence of systemic sepsis. Resection arthroplasty was not considered after a discussion with the patient’s family due to the patient’s level of mobility and functional goals. Another treatment option, considered the gold standard for PJI, is two-stage exchange arthroplasty which has been reported to control infection in 89% of first revisions [5, 7, 12]. However, two-stage exchange arthroplasty poses risks of massive blood loss and increased mortality in comparison to DAIR, especially in a well-fixed prothesis like this [10, 13]. In comparing patients who underwent revision total knee arthroplasty due to PJI vs. non-infectious causes, the OR for death in patients undergoing revision for PJI was 3.25, and the OR for sepsis was 8.73 [13]. These factors were incorporated into the informed consent process, resulting in the decision to proceed with DAIR in this medically frail patient. The results for this patient, thus far have been favorable, with no indication of treatment failure. It may reason, therefore, that a single-stage DAIR, while not commonly utilized, may be considered a valid treatment option that can offer sufficient treatment of infection while avoiding potential complications associated with more invasive procedures. With suboptimal success rates reported for DAIR around 70%, we must discuss the implications for patients treated with DAIR who fail treatment and must undergo two-stage exchange arthroplasty. Huffaker et al. found that patients treated with initial DAIR had a higher risk for septic re-revision (hazard ratios [HR] 3.09, 95% CI 2.22–4.42) [14]. However, septic re-revision rates were similar between patients treated with two-stage exchange arthroplasty alone and those treated with DAIR followed by two-stage exchange arthroplasty (HR 1.11, 95% CI 0.58–2.12) [14]. A complication of the patient’s final DAIR procedure was a development of a motor nerve injury to the sciatic nerve. Motor nerve palsy is an uncommon complication following primary THA with an incidence of 0.6–3.7% [15]. However, in the revision hip surgery setting, the incidence is as high as 7.6%, perhaps due to nerve entrapment in scar tissue [15]. This case of revision surgery utilized a posterior hip exposure to follow the previous approach used in index THA which may have increased the risk of sciatic nerve injury [15]. Regardless of etiology, the likelihood of nerve recovery following complete nerve palsies is 36% [15]. Documenting a detailed pre-operative neurological exam and discussing the risk of nerve injury are crucially important parts of the informed consent process. Caution must be taken to protect the sciatic nerve when positioning and retracting during revision surgery, especially in a medically vulnerable patient such as ours. This report has limitations on follow-up potential. Reinfection has been reported to occur up to years after initial treatment [7].
This case demonstrates short-term success with the utilization of debridement, antibiotics, and implant retention in the treatment of hip PJI in a medically infirm patient. Surgeons must carefully weigh the goal of infection eradication with the significant risks of massive blood loss and increased mortality associated with exchange arthroplasty. This report may serve to inform future patient counseling.
In a patient with septicemia from acute hematogenous PJI, DAIR may be a sufficient treatment option when exchange arthroplasty is otherwise strongly contraindicated due to a significant risk of mortality.
References
- 1.Sloan M, Premkumar A, Sheth NP. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am 2018;100:1455-60. [Google Scholar]
- 2.Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am 2009;91:128-33. [Google Scholar]
- 3.Alp E, Cevahir F, Ersoy S, Guney A. Incidence and economic burden of prosthetic joint infections in a university hospital: A report from a middle-income country. J Infect Public Health 2016;9:494-8. [Google Scholar]
- 4.Lee HD, Prashant K, Shon WY. Management of periprosthetic hip joint infection. Hip Pelvis 2015;27:63-71. [Google Scholar]
- 5.Gerritsen M, Khawar A, Scheper H, van der Wal R, Schoones J, de Boer M, et al. Modular component exchange and outcome of DAIR for hip and knee periprosthetic joint infection: A systematic review and meta-regression analysis. Bone Jt Open 2021;2:806-12. [Google Scholar]
- 6.Uchiyama K, Takahira N, Fukushima K, Moriya M, Yamamoto T, Minegishi Y, et al. Two-stage revision total hip arthroplasty for periprosthetic infections using antibiotic-impregnated cement spacers of various types and materials. ScientificWorldJournal 2013;2013:147248. [Google Scholar]
- 7.McQuivey KS, Bingham J, Chung A, Clarke H, Schwartz A, Pollock JR, et al. The double DAIR: A 2-Stage debridement with prosthesis-retention protocol for acute periprosthetic joint infections. JBJS Essent Surg Tech 2021;11:e19.00071-e19.00071. [Google Scholar]
- 8.Lange J, Troelsen A, Søballe K. Chronic periprosthetic hip joint infection. A retrospective, observational study on the treatment strategy and prognosis in 130 non-selected patients. PLoS One 2016;11:e0163457. [Google Scholar]
- 9.Barton CB, Wang DL, An Q, Brown TS, Callaghan JJ, Otero JE. Two-stage exchange arthroplasty for periprosthetic joint infection following total hip or knee arthroplasty is associated with high attrition rate and mortality. J Arthroplasty 2020;35:1384-9. [Google Scholar]
- 10.Goel R, Buckley P, Sterbis E, Parvizi J. Patients with infected total hip arthroplasty undergoing 2-stage exchange arthroplasty experience massive blood loss. J Arthroplasty 2018;33:3547-50. [Google Scholar]
- 11.Goswami K, Parvizi J, Maxwell Courtney P. Current recommendations for the diagnosis of acute and chronic PJI for hip and knee-cell counts, alpha-defensin, leukocyte esterase, next-generation sequencing. Curr Rev Musculoskelet Med 2018;11:428-38. [Google Scholar]
- 12.Bejon P, Berendt A, Atkins BL, Green N, Parry H, Masters S, et al. Two-stage revision for prosthetic joint infection: Predictors of outcome and the role of reimplantation microbiology. J Antimicrob Chemother 2010;65:569-75. [Google Scholar]
- 13.Boddapati V, Fu MC, Mayman DJ, Su EP, Sculco PK, McLawhorn AS. Revision total knee arthroplasty for periprosthetic joint infection is associated with increased postoperative morbidity and mortality relative to noninfectious revisions. J Arthroplasty 2018;33:521-6. [Google Scholar]
- 14.Huffaker SJ, Prentice HA, Kelly MP, Hinman AD. Is there harm in debridement, antibiotics, and implant retention versus two-stage revision in the treatment of periprosthetic knee infection? Experiences within a large US health care system. J Arthroplasty 2022;37:2082-9.e1. [Google Scholar]
- 15.Hasija R, Kelly JJ, Shah NV, Newman JM, Chan JJ, Robinson J, et al. Nerve injuries associated with total hip arthroplasty. J Clin Orthop Trauma 2018;9:81-6. [Google Scholar]