Hemorrhagic ligamentum flavum cyst can occur not only in a spondylolisthetic segment but also in an adjacent level and should not be missed on imaging before deciding management.
Dr. Mayukh Guha, Spine Services, Indian Spinal Injuries Centre, Sector C, Vasant Kunj, New Delhi - 110070, India. E-mail: drmayukhguha@yahoo.com
Introduction: Occurrence of hemorrhagic cyst inside ligamentum flavum is a very rare phenomenon and presents with back pain, radiculopathy, or neurogenic claudication. Various causes reported in the literature are trauma, anticoagulant therapy, and increased micromotion in the setting of unstable and degenerated motion segment.
Case Report: We report a case of 41-year-old male patient who presented with claudication pain in both lower limbs for the past 6 months associated with bilateral calf atrophy. Plain radiograph with dynamic films showed lytic spondylolisthesis at L4-L5 level. Magnetic resonance imaging revealed a hemorrhagic cyst inside ligamentum flavum at the L3-L4 level occupying the posterior epidural space severely compressing the thecal sac. After a thorough diagnostic and therapeutic work up, we did a midline sparing decompression of L3-L4 level under microscope without fixing the listhetic segment. The patient had significant pain relief after surgery and doing well till now.
Conclusion: In general, hemorrhagic cyst of ligamentum flavum is seen in a degenerated lumbar spine at the areas of increased micromotion and instability. Our case has shown that it can also occur in an adjacent segment of spondylolisthesis or instability. The obvious finding like listhesis in the adjacent segment may hinder a spine surgeon from diagnosing the cyst component and may guide to a erroneous treatment outline. Hence, it should not be missed in the imaging.
Keywords: Ligamentum flavum cyst, hemorrhagic flavum cyst, lytic spondylolisthesis.
Ligamentum flavum cysts, along with cysts of the posterior longitudinal ligament and facet joints, constitute a less prevalent subgroup within the classification of juxtafacet cysts [1]. Synovial cyst and ganglion cysts are most common types of epidural cyst reported in the literature and were first reported by Moiel et al. [2] in 1967. There is still an uncertainty regarding pathophysiological mechanism of these cysts [3]. Flaval cysts are mostly seen in the dorsolateral aspect in the canal causing back pain, radicular pain, or claudication pain. Myxomatous degeneration with collection of myxoid material between the layers of flavum is seen in flaval cyst [4]. However, occurrence of the hemorrhagic cyst within the ligamentum flavum is a very rare phenomenon. In general, it is seen in the setting of degenerative lumbar spine especially at the level of significant instability or micromotion. We report the case of a 41 years young male having hemorrhagic ligamentum flavum cyst one segment above lytic spondylolisthesis causing claudication pain and numbness with atrophy of both calf muscles.
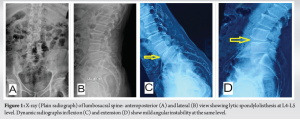
A 41–year-old young male patient, a doctor by profession, presented to us with complaints of claudication pain in both lower limbs (predominantly both calf muscles) since past 6 months without any walking imbalance. Gradually, the claudication distance was decreasing over the past 2 months and he could hardly able to walk more than 100 m when he presented to us. There was very minimal associated low back pain with no aggravating factors. The patient had no subjective weakness of any lower limb or any bladder bowel symptoms such as urinary straining, incontinence, or constipation. The patient was on conservative treatment in the form of gamma-aminobutyric acid (GABA)-analogs and various modalities of physiotherapy, but there was hardly any symptomatic relief. On examination, there was no midline or paraspinal tenderness seen over the lumbosacral (LS) spine. We noticed atrophy of both of his calf muscles. Neurological evaluation revealed grade 4 power in both ankle plantar flexion (S1 myotome) according to Medical Research Council scale, other myotomes being normal. There were no upper motor neuron signs on examination. Plain radiograph of LS spine showed grade 1 lytic spondylolisthesis at L4–L5 segment with moderate radiographic instability (Fig. 1). Computed tomography scan also confirmed the radiographic picture (Fig. 2).
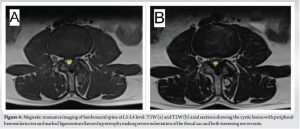
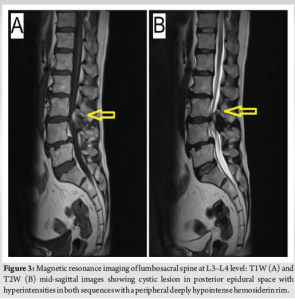
Magnetic resonance imaging (MRI) of LS spine revealed a well-defined cystic lesion in midline of the spinal canal at L3–L4 level in the posterior epidural space with hyperintense signals in both T1- and T2-weighted sequences with a peripheral deeply hypointense hemosiderin rim, pointing toward a hemorrhagic cyst which was compressing the thecal sac and both the traversing L4 nerve roots. It was also accompanied by marked hypertrophy of ligamentum flavum and facetal arthropathy at the same level (Fig. 3 and 4).
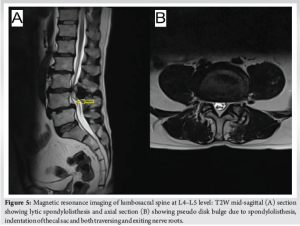
As expected, we noted bilateral spondylolysis at L4 with grade 1 anterolisthesis of L4 over L5 with pseudo disk bulge indenting the thecal sac and both L4 exiting and L5 traversing nerve roots (Fig. 5).
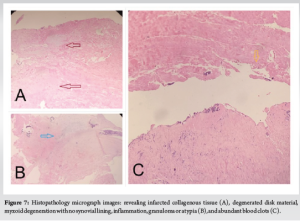
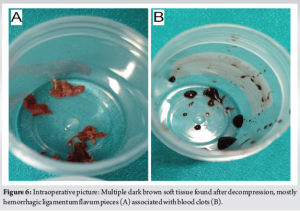
Hence, either L3–L4 or L4–L5 or both the segments contributed to his claudication symptoms. After discussing all the treatment options, at first, we went ahead with bilateral L4–L5 transforaminal epidural steroid injection (TFESI) which caused no symptomatic relief to the patient. After that, we gave bilateral L3–L4 TFESI which gave the patient significant pain relief, his walking distance improved but unfortunately it lasted for 2 days only. Hence, we deducted that his present symptoms were mainly due to central canal stenosis at L3–L4 level. As his profession demanded long standing and walking, we offered him surgery after thorough prognostication. As he had very minimal low back pain and that pain did not aggravate with change of posture or bending, we decided to go ahead only with decompression of L3–L4 segment without any instrumentation at any level and not addressing spondylolisthesis at L4–L5 as of then. As planned, we did a midline sparing L3–L4 decompression from the left side under the operating microscope. Contralateral right side was also decompressed by “over the top” method. Intraoperatively, a cyst extending into the ligamentum flavum containing dark brown muddy tissue and blood clots was found compressing the thecal sac and nerve roots (Fig. 6). The wall of the cyst was not communicating with the facet joint capsule. Thorough decompression was done, cyst contents along with the ligamentum flavum were excised and we could free the central canal, both lateral recess and both foramen. Tissue samples were sent for culture and histopathology. The patient was mobilized the next day and he reported total relief of claudication symptoms with walking distance improving significantly. He was discharged the same day. Histopathological analysis revealed blood clots, infarcted collagenous tissue, degenerated disk material, myxoid degeneration with no synovial lining, inflammation, and granuloma or atypia (Fig. 7). All procedures performed were in accordance with the ethical standards of the institutional and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Juxtafacet cysts are present in 0.5–0.6% of the population [5]. They present most commonly with radicular pain, less commonly with acute or chronic back pain and rarely with neurogenic claudication [6]. There are three potential origin of these cysts – facet joint, ligamentum flavum, and posterior longitudinal ligament. They are most commonly found in degenerative mobile lumbar spine with over 50% occurring at L4/5 and the remainder mostly found at L5/S1 and L3/4 [7]. Hemorrhagic complications occur in <10% of juxtafacet cysts [8]. Ligamentum flavum cysts are diagnosed by their location and contents and can be easily differentiated by their histopathology pictures. In general, ligamentum flavum cysts originate from the inner surface of the ligament and are not closely related to the facet joint [9]. Histologically, they usually have myxoid degeneration and do not show a synovial cell layer on the inner surface of the cyst wall [10]. Hemorrhagic complications are quite rare in ligamentum flavum cyst or for that matter in any kind of juxtafacet cysts. Normal ligamentum flavum is highly resistant to any injury, it is thought that degenerative changes in the ligamentum flavum make them more susceptible to bleed secondary to any kind of trauma or stretching force to the back or repetitive micromotion [11]. Xu et al. found out a clear history of physical trauma in eight of 30 patients in their series [12]. Nourbakhsh and Garges [13] reported the anticoagulant therapy as a potential causative factor for hemorrhagic facet cysts. In our case, a 41-year-old active male presented with bilateral neurogenic claudication and bilateral calf atrophy which were gradually worsening. Detailed imaging revealed lytic spondylolisthesis at L4–L5 and suspected hemorrhagic cyst occurring inside ligamentum flavum at L3–L4. We tried to find out which is the symptomatic level and after staged TFESI, we were sure that L3–L4 stenosis were causing his symptoms. Degenerative changes were very prominent at L3–L4 with superadded hypermobility and degeneration due to L4–L5 lytic spondylolisthesis. L3–L4 segment had become highly stressed and had to overwork due to instability at L4–L5 which may have caused hemorrhage inside ligamentum flavum. These associations of spondylolisthesis, facet arthropathy, and disk degeneration are found consistently in literature, pointing toward degenerative changes and instability in hemorrhagic cyst pathogenesis [6]. Lyons et al. found that cyst hemorrhage more often seen in relatively young active males, further supporting a microtrauma hypothesis if occupation and lifestyle is considered as seen in our case also [5]. Recently, Watanabe et al. reported a case of hemorrhagic ligamentum flavum cyst in the upper disk level of a LS transitional vertebra [10]. Increased stress and hypermobility between the upper instrumented disks of transitional vertebra have been speculated as the culprit behind the hemorrhage. Although diagnoses may be different, the pathogenesis of hemorrhagic cyst may be exactly same in our case as well. MRI picture of a hemorrhagic juxtafacet cyst depends on factors including protein content, blood products, and timing of hemorrhage within the cyst [5]. T2-weighted image of these cysts shows varying signal intensity due to previous old hemorrhages, elevated protein content, and calcification [14]. In our case, MRI showed a well-defined cystic lesion in the midline of the posterior epidural space with hyperintensity in both the sequences with a peripheral hypointense hemosiderin rim, strongly pointing toward an acute on chronic hemorrhagic cyst. Pathologically, facet joint cysts are composed of cuboid or pseudocolumnar epithelium and have synovial lining. Gazzeri et al. reported a 59-year-old woman presenting with sudden onset severe radicular pain and neurodeficit secondary to acute hemorrhage into a ligamentum flavum cyst at L3–L4 level [9]. Histopathology revealed myxoid degeneration of the ligamentum flavum with hemorrhage in the cystic cavity without a synovial layer. The cyst in our case had no continuity between the cyst and the facet joints on imaging and gross macroscopic finding. Histopathology also did not show a synovial cell layer on the inner surface of the wall of the cyst. The intraoperative finding of hemorrhage inside a cystic cavity extending into the ligamentum flavum and histopathologic finding of blood clots with degenerative changes are consistent with hemorrhagic cyst arising from ligamentum flavum. To treat symptomatic juxtafacet cysts, conservative management has been tried in the form of anti-inflammatory, GABA-analogs, oral steroids, or transforaminal injections but literature is in the favor of surgical management [5, 7]. In general, laminotomy or laminectomy followed by cyst excision is performed. Decompression along with posterior fixation has been done very rarely [15]. The major diagnostic dilemma in our case was to ascertain the symptomatic level of the patient, L3–L4 or L4–L5 or both. We deducted L3–L4 hemorrhagic cyst as the culprit pathology by giving serial transforaminal injections as stated earlier. Then, the therapeutic dilemma was to whether decompress and/or fix the listhetic L4–L5 segment as well. Considering his bare minimum low back pain and absence of any instability pain, we decided to skip that level. Furthermore, to minimize iatrogenic instability, we have done a microscopic procedure with midline sparing left L3 laminotomy and decompression. As of now 4 months after surgery, the patient is completely pain free, has started his regular daily activities and he does not complain of any back pain as well. He has been counseled properly that he may need future surgery of L4–L5 spondylolisthesis if that segment causes him back pain or neurologic symptoms.
Hemorrhagic ligamentum flavum cyst is a rare entity. Normally, it occurs in degenerated lumbar spine with areas of increased stress and micromotion and may be missed in imaging due to overwhelming presence of other obvious degenerative entities. Literature shows that it can occur in a same spondylolisthetic segment but we have seen the incident in the upper adjacent level of the lytic spondylolisthesis in a young adult patient. Hence, the presence of this type of pathology can occur not only in the degenerated segment, but also in the adjacent segment and one should not miss it in MRI before planning the treatment options.
Although hemorrhagic ligamentum flavum cyst is a rare cause of radiculopathy or neurogenic claudication, it should be suspected if MRI shows a cystic lesion in a degenerated lumbar spine. Literature shows that it occurs in the same spondylolisthetic segment, but it may occur in an adjacent segment of a listhesis also, as in our case.
References
- 1.Nizamani WM. Ligamentum flavum cyst: An uncommon but recognizable and surgically correctable category of juxtafacet cyst. Radiol Case Rep 2018;13:302-4. [Google Scholar]
- 2.Moiel RH, Ehni G, Anderson MS. Nodule of the ligamentum flavum as a cause of nerve root compression. Case report. J Neurosurg 1967;27:456-8. [Google Scholar]
- 3.Cakir E, Kuzeyli K, Usul H, Peksoylu B, Yazar U, Reis A, et al. Ligamentum flavum cyst. J Clin Neurosci 2004;11:67-9. [Google Scholar]
- 4.Baker JK, Hanson GW. Cyst of the ligamentum flavum. Spine (Phila Pa 1976) 1994;19:1092-4. [Google Scholar]
- 5.Lyons MK, Atkinson JL, Wharen RE, Deen HG, Zimmerman RS, Lemens SM. Surgical evaluation and management of lumbar synovial cysts: The Mayo Clinic experience. J Neurosurg 2000;93:53-7. [Google Scholar]
- 6.Boviatsis EJ, Stavrinou LC, Kouyialis AT, Gavra MM, Stavrinou PC, Themistokleous M, et al. Spinal synovial cysts: Pathogenesis, diagnosis and surgical treatment in a series of seven cases and literature review. Eur Spine J 2008;17:831-7. [Google Scholar]
- 7.Khan AM, Synnot K, Cammisa FP, Girardi FP. Lumbar synovial cysts of the spine: An evaluation of surgical outcome. J Spinal Disord Tech 2005;18:127-31. [Google Scholar]
- 8.Gong K, Wang Z, Chen MM, Luo Z. Diagnosis and surgical management of intraspinal hemorrhagic juxtafacet cysts in lumbar spine: Experience of eight cases. Neurol India 2010;58:288-91. [Google Scholar]
- 9.Gazzeri R, Canova A, Fiore C, Galarza M, Neroni M, Giordano M. Acute hemorrhagic cyst of the ligamentum flavum. J Spinal Disord Tech 2007;20:536-8. [Google Scholar]
- 10.Watanabe K, Mitsui K, Sasaki J, Kumaki D. Subacute hemorrhagic cyst of the ligamentum flavum occurred in the lumbosacral transitional vertebra presenting as progressive lumbar nerve root compression: A case report. J Spine Surg 2021;7:238-43. [Google Scholar]
- 11.Sweasey TA, Coester HC, Rawal H, Blaivas M, McGillicuddy JE. Ligamentum flavum hematoma. Report of two cases. J Neurosurg 1992;76:534-7. [Google Scholar]
- 12.Xu R, Solakoglu C, Maleki Z, McGirt MJ, Gokaslan ZL, Bydon A. Hemorrhagic synovial cyst: The possible role of initial trauma and subsequent microtrauma in its pathogenesis: Case report. Neurosurgery 2011;68:E858-65. [Google Scholar]
- 13.Nourbakhsh A, Garges KJ. Lumbar synovial joint hematoma in a patient on anticoagulation treatment. Spine (Phila Pa 1976) 2007;32:E300-2. [Google Scholar]
- 14.Apostolaki E, Davies AM, Evans N, Cassar-Pullicino VN. MR imaging of lumbar facet joint synovial cysts. Eur Radiol 2000;10:615-23. [Google Scholar]
- 15.Cruz-Conde R, Berjano P, Buitron Z. Ligamentum flavum hematoma presenting as progressive root compression in the lumbar spine. Spine (Phila Pa 1976) 1995;20:1506-9. [Google Scholar]