Isolated Diaphyseal Malrotation deformities of Tibia (post Intra-medullary nailing) can be attempted for correction in a minimally invasive fashion without disturbing the intramedullary implants.
Dr. Tarkik Thami, Senior Resident, Department of Orthopedic Surgery, Post Graduate Institute of Medical Education and Research, Chandigarh -160012, India. E-mail: thamitarkik@gmail.com
Introduction: Intramedullary nailing is a commonly performed surgery for tibia diaphysis fractures. However, in selected cases, this procedure can get complicated with rotational malalignment if not checked carefully intra-operatively.
Case Report: A 29 year-old male sustained polytrauma and was treated with intramedullary nailing for bilateral femur and right-side tibia fractures. Postoperatively, the patient noticed extreme in-toeing suggesting an internal rotation deformity, which caused great difficulty in walking. The patient was planned for a revision surgery to correct the internal rotation deformity, 6 months after the index surgery. A minimally invasive metaphyseal osteotomy was performed, away from his fracture site by drilling multiple holes. The distal locking bolts of the interlocking nail were removed, and two K wires used to achieve the desired correction angle. After rotating the distal fragment, locking bolts were reinserted in new holes. We kept the patient on our regular follow-up till he achieved sound union at the osteotomy site, after which we allowed him unrestricted activities.
Conclusion: The presence of an intramedullary nail can hence help the surgeon in correcting such isolated rotational deformities without getting into the hassle of implant removal to achieve the same.
Keywords: Minimally invasive osteotomy, tibia malrotation deformity, polytrauma.
Diaphyseal Tibia fracture is a commonly encountered injury for a trauma surgeon. Most of these fractures are commonly subjected to intramedullary nailing, which acts like a load sharing implant and helps in early mobilization of the patient. Although a simple procedure, it has its own share of possible complications such as non-union, malunion, and malalignment in certain circumstances [1-3]. Multi-fragmentary mid shaft tibia fractures and open fractures with loss of bone fragments have a higher chance of developing post-nailing axial malrotation [4]. In contrast, the absence of a fibula fracture is favorable in terms of preventing rotational malalignment. Symptomatic cases of malalignment may require deformity corrective surgery [5]. We would like to report a case of a segmental tibia fracture fixed with intramedullary nailing which mal-united in internal rotation. This mal-rotational deformity was subsequently corrected through a minimally invasive osteotomy away from the fractured site.
A 29-year-old male sustained a road traffic accident and presented to our trauma emergency with multiple fractures. The was diagnosed with closed fractures of the right shaft of the femur, left ipsilateral neck with the shaft of femur, left patella fracture, and an open fracture of right shaft of tibia. Patient was planned for damage control orthopedics and temporary external fixators were applied for all fractures of the lower extremities at approximately 36-h post-injury. The patient subsequently underwent definitive fixation for all the fractures after 7 days. Cannulated cancellous screws were used for fixation of neck of femur fracture; interlocking nails for the fixation of bilateral femora shaft fractures and tibia shaft fracture and tension band wiring for patella fracture. Post-surgery, he was allowed partial weight bearing (as tolerated) with a walking aid in view of multiple fractures. He was discharged in a satisfactory condition on 4th post-operative day. Our patient was put on a structured physiotherapy program to ensure an unaided gait at 6-week postoperatively. Regular follow-up visits revealed that all fractures went on to unite (Fig. 1 a, b).
However, the patient noticed in-toeing gait on the right-sided lower limb after 6 months and complained that he needed to abduct his right leg to prevent it from obstructing his left leg (during walking). This internal rotation deformity hindered his activities of daily living. His physical examination revealed a thigh-foot angle of 15° in internal rotation and a 1 cm shortening (Fig. 2). The ipsilateral knee range of motion was slightly restricted (0-110 of flexion). After a thorough discussion with the patient regarding treatment options, a Derotation osteotomy of the leg was planned at the junction of the proximal and middle third of the tibia.
Surgical steps
The procedure was performed in a supine position under the effect of pneumatic tourniquet. Under fluoroscopic guidance, the osteotomy site was marked on the skin at the junction of the proximal and middle 1/3rd of the tibia, 6 cm away from the original fracture site. Subsequently, a 3 cm longitudinal incision was given directly over the crest of tibia and centered at the skin marking. Multiple bi-cortical holes were drilled on the antero-medial and lateral surface of the tibia with a 2 mm drill bit. Corticotomy (Fig. 3 a) of the antero-medial and lateral cortices was performed with a corticotome, carefully maneuvering around the intramedullary nail. Another incision of 2 cm length was given on the medial aspect of the leg along the postero-medial border of the tibia (Fig. 3 b). The gastro-soleus muscle was retracted posteriorly, and corticotomy of the posterior cortex of the tibia was performed. All instrumentation was performed carefully to avoid damaging the nail in situ. Fibular osteotomy was also done at the same level with a separate incision on the posterolateral aspect. Two K-wires were inserted perpendicular to the anteromedial cortex of the tibia parallel to each other in the sagittal plane (Fig. 3 a-c). These K-wires served as a measure of the degree of rotational correction obtained. The distal locking bolts were removed through an incision over the previous scar mark. The removal of distal bolts of the nail made the entire fragment distal to the osteotomy mobile. The correction was achieved by external rotation of the segment distal to the osteotomy site by an angle of 30° to achieve a thigh foot angle of 15° external rotation (-15° to +15°). After ensuring proper alignment under fluoroscopic guidance, the distal locking screws were reinserted in new holes. The immediate post-operative radiographs (Fig. 4) were obtained after 24 h and partial weight bearing (as tolerated) was allowed in the immediate postoperative period.
Outcome and follow-up
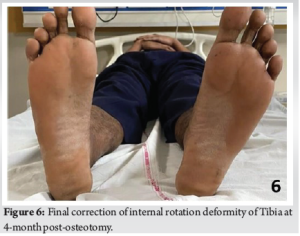
The patient was examined on serial follow-up visits and a sound union was achieved at the osteotomy site (Fig. 5a and b) at 3-month post-procedure (de-rotation osteotomy) with a complete return to function with respect to activities of daily living and correction of the deformity (Fig. 6).
Mikulicz and Le Damany have defined tibial torsion as a rotation of the proximal versus the distal articular axis in the transverse plane [5]. The incidence and severity of tibial malrotation deformity after IM nailing are not well documented in the literature [5]. The available literature is also sparse as far as the acceptable range of axial mal-rotation deformity is concerned. Usually, a limb shortening greater than 1 cm and angular/ rotational deformities greater than 10° are considered unacceptable [3]. The reported incidence of tibia malrotation deformity following clinical measurement alone varies from 0 to 6% [6]. However, the incidence of this deformity measured with CT scan ranges between 22 and 36% [7]. Malrotation deformity of the tibia may lead to significant limitation of function and gait disturbance for patients [8, 9]. However, there is no clear consensus about the indications for re-operating such patients to correct their deformity. There was a significant amount of tibia malrotation in our patient, hindering his activities of daily living. In such a scenario, deformity corrective surgery involving a nail removal is associated with longer surgical duration and has no added benefit over retaining the nail. Retaining the nail in situ (like in our case) has several advantages such as reduced surgical time, lesser post-operative pain, and minimally invasive nature [5]. To the best of our knowledge, only one such case has been reported where an external rotation deformity of tibia was corrected with minimal invasive osteotomy at the fracture site [10]. However, in our case, we corrected the tibia internal rotation deformity by a minimally invasive osteotomy proximal to the fracture site. Our decision was based on the fact that osteotomy of the metaphyseal bone has a better union rate as compared to a diaphyseal osteotomy.
The actual prevalence of malrotation deformities is grossly underestimated in patients with concomitant ipsilateral tibia and femur shaft fractures, multi-fragmentary fractures, or polytrauma patients. It is imperative that the operating surgeon keep a high index of suspicion to prevent fixation of these fractures in mal-rotation during intramedullary nailing. Since there is limited literature concerning deformity correction with a nail in situ, our report further strengthens the usefulness of this technique for the correction of diaphyseal rotational deformities with minimal or no shortening.
It is crucial to avoid fixation of lower extremity long bone fractures in Malrotation to prevent Gait disturbances which can further lead to loss of ability to perform activities of daily living.
References
- 1.Zelle BA, Boni G. Safe surgical technique: Intramedullary nail fixation of tibial shaft fractures. Patient Saf Surg 2015;9:40. [Google Scholar]
- 2.Kyrö A. Malunion after intramedullary nailing of tibial shaft fractures. Ann Chir Gynaecol 1997;86:56-64. [Google Scholar]
- 3.Puloski S, Romano C, Buckley R, Powell J. Rotational malalignment of the tibia following reamed intramedullary nail fixation. J Orthop Trauma 2004;18:397-402. [Google Scholar]
- 4.Coelho Fernandes AR, Sagoo KS, Oluku J, Cheema KS. Tibial malrotation following intramedullary nailing: A literature review. Cureus 13:e19683. [Google Scholar]
- 5.Jakob RP, Haertel M, Stüssi E. Tibial torsion calculated by computerised tomography and compared to other methods of measurement. J Bone Joint Surg Br 1980;62-B:238-42. [Google Scholar]
- 6.Buckley R, Mohanty K, Malish D. Lower limb malrotation following MIPO technique of distal femoral and proximal tibial fractures. Injury 2011;42:194-9. [Google Scholar]
- 7.Prasad CV, Khalid M, McCarthy P, O’Sullivan ME. CT assessment of torsion following locked intramedullary nailing of tibial fractures. Injury 1999;30:467-70. [Google Scholar]
- 8.Puno RM, Vaughan JJ, Stetten ML, Johnson JR. Long-term effects of tibial angular malunion on the knee and ankle joints. J Orthop Trauma 1991;5:247-54. [Google Scholar]
- 9.Van der Werken C, Marti RK. Post-traumatic rotational deformity of the lower leg. Injury 1983;15:38-40. [Google Scholar]
- 10.Takase K, Lee SY, Waki T, Fukui T, Oe K, Matsumoto T, et al. Minimally invasive treatment for tibial malrotation after locked intramedullary nailing. Case Rep Orthop 2018;2018:4190670. [Google Scholar]